Chronic bronchitis
Table of Contents
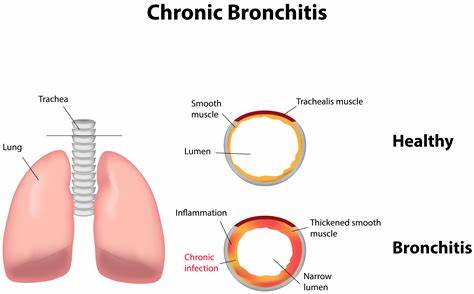
What is chronic bronchitis?
- Bronchitis is inflammation of the breathing tubes.
- These are the airways called bronchi.
- This inflammation causes too much mucus production and another change.
- There are various types of bronchitis.
- But the most usual are acute and chronic.
- Chronic bronchitis is the condition of long-term inflammation of the bronchi.
- It is usual among smokers.
- People with chronic bronchitis protect themselves to get lung infections more easily.
- They too have episodes of acute bronchitis, when symptoms are poor.
- Bronchitis is an inflammation of the border of the bronchial tubes.
- These are the tubes that bring air to and from your lungs.
- People who have bronchitis sometimes have a persistent cough that brings up thick, discolored mucus.
- They may too experience wheezing, chest pain, and shortness of breath.
To be classified as chronic bronchitis:
- You must have a cough and mucus most of the days for at least three months a year, for two years in a row.
- Other causes of symptoms, like tuberculosis or other lung diseases, must be ruled out.
- If you are suffering from chronic bronchitis it is also called chronic obstructive pulmonary disease (COPD).
- This is a big group of lung diseases that includes chronic bronchitis.
- These diseases can block airflow in the lungs and causes breathing problems.
- The two most common conditions of chronic obstructive pulmonary disease (COPD) are chronic bronchitis and emphysema.
Bronchitis may be either acute or chronic:
- Acute bronchitis: Acute bronchitis develops from a cold or another respiratory infection. Symptoms last less than three weeks trusted source, often improving within a few days without lasting effects.
- Chronic bronchitis: Bronchitis is classified as chronic when symptoms — primarily productive cough — last more than 3threemonths trusted source within a span of two years.
- The continuous inflammation in the lining of the bronchial tubes causes excessive amounts of sticky mucus to build up in the airways, restricting the amount of airflow into and out of the lungs.
- Chronic bronchitis is a type of chronic obstructive pulmonary disease (COPD).
- Many people who have chronic bronchitis eventually develop emphysema, which is also a type of chronic obstructive pulmonary disease (COPD).
- According to the American Lung Association, more than 16.4 million people in the United States live with chronic obstructive pulmonary disease (COPD).
- However, there are many more people who do not know they have developed it.
- The majority of chronic obstructive pulmonary disease (COPD) symptoms take a while to develop, so people may mistakenly believe that the condition is not life-threatening and ignore the symptoms up to the condition has progressed to a more advanced stage.
- Although the condition can not be cured, the symptoms can be managed with treatment once a diagnosis is made.
What are causes of the chronic bronchitis?
- Chronic bronchitis is not caused by viruses or bacteria.
- Most experts agree that the important cause of chronic bronchitis is cigarette smoking.
- Air pollution and your work environment may play a role.
- This is especially true if you also smoke.
- Chronic bronchitis happens when the lining of the bronchial tubes repeatedly becomes irritated & inflamed.
- The continuous irritation & swelling can damage the airways and cause a buildup of sticky mucus, making it difficult for air to move through the lungs. This leads to breathing difficulties that slowly get worse.
- The inflammation can also damage the cilia, which are the hair-like structures that help to keep the air passages free of germs and other irritants. When the cilia do not work properly, the airways often become a breeding ground for bacterial and viral infections.
Causes of chronic bronchitis involve:
Infections: Infections generally trigger the initial irritation and swelling that lead to acute bronchitis.
Smoking tobacco: Smoking is the leading risk factor for developing chronic bronchitis. Over ninety percent of those with the disease have a history of smoking.
Secondhand smoke: Exposure to secondhand smoke can increase a person’s risk of developing chronic bronchitis.
Air pollution: Exposure to air pollution, chemical or industrial fumes, dust, & toxic gases can increase the risk for chronic bronchitis.
Bronchitis symptoms often occur with other lung diseases, such as:
- Asthma,
- Pulmonary emphysema,
- Scarring of the lungs (pulmonary fibrosis),
- Sinusitis,
- Tuberculosis,
- Upper respiratory infections,
- Disability,
- Frequent and severe infections that affect your airways,
- Narrowing and plugging of your breathing tubes (bronchi),
- Trouble breathing.
What are the symptoms of chronic bronchitis?
- Below are the most usual symptoms of chronic bronchitis.
- Yet each person may have slightly different symptoms.
- Later a long period of inflammation and irritation in the bronchial tubes, chronic bronchitis can result in several hallmark symptoms.
Symptoms may involve:
- Cough, often called smoker’s cough,
- Coughing up mucus (expectoration),
- Wheezing,
- Chest discomfort,
- People with chronic bronchitis often have a cough and make mucus for many years previous they have shortness of breath.
- As time passes, the amount of mucus slowly increases due to the increased production of mucus in the lungs.
- The mucus builds up after sometimes the bronchial tubes, resulting in difficulty breathing, especially during physical activity.
Other symptoms of chronic bronchitis can involve:
- fatigue,
- fever,
- frequent and severe respiratory infections,
- wheezing and crackling sounds when breathing,
- bluish fingernails, lips, and skin caused to low oxygen levels,
- swelling in the legs & ankles (peripheral edema).
- As chronic bronchitis progresses, symptoms can differ in severity and frequency.
- For example, a cough may vanish temporarily, only to be followed by a period of more intense coughing.
More severe episodes may be triggered by various factors, involving:
- respiratory tract infections, like as cold or flu,
- infections elsewhere in the body,
- exposure to environmental irritants, like as air pollution or dust,
- heart conditions.
How is chronic bronchitis diagnosed?
- Your healthcare provider will take a complete health history & do a physical exam.
He or she may order the following tests:
Pulmonary function tests
- These tests assist to measure the lung’s ability to move air in & out of your lungs.
- The tests are sometimes done with special machines that you breathe into.
They may involve:
Spirometry
- This test uses a spirometer device to look at how well your lungs are working. It is one of the simplest, most usual pulmonary function tests.
It may be used for any or all of these reasons:
- To look out how well your lungs take in, hold, & move air,
- To keep looking at lung disease,
- To look at how well the treatment is working,
- To look out how serious your lung disease is,
- To look out if your lung disease is restrictive or obstructive. Restrictive means less air will require into your lungs. Obstructive means less air will exhale from your lungs.
Peak flow monitor
- This test counts the fastest speed you can blow air out of your lungs. Inflammation & mucus in the large airways in the lungs small the airways. This less the speed of air leaving the lungs. It can be counted with a peak flow monitor. This measurement is very much important in asking how well your disease is being controlled.
Arterial blood gas
- This blood test is used to check the amount of oxygen & carbon dioxide (CO2) in your blood. It too measures the acidity of your blood.
Pulse oximetry
- An oximeter is a less machine that measures the amount of oxygen in your blood. To get this measurement, a less sensor is taped or clipped onto a finger or toe. When the machine is on, less red light can be seen in the sensor. The sensor is painless, & the red light does not get hot.
Chest X-ray
- This test makes pictures of your internal tissues, bones, & organs, involving the lungs.
CT scan
- This imaging test uses a combination of X-rays & computer technology to make images of the body. A CT scan shows detailed images of any part of the body, involving the bones, muscles, fat, and organs. CT scans are more detailed than typical X-rays.
How is chronic bronchitis treated?
- Treatment for chronic bronchitis is aimed at treating the causes & symptoms.
- Although there is no cure for chronic bronchitis, the disease can be managed with medical treatment and lifestyle adjustments, especially when a diagnosis is made early on.
It may involve:
- Quitting smoking,
- Staying away from secondhand smoke & other lung irritants,
- Taking medicines by mouth (oral) to open airways and assist clear away mucus,
- Taking inhaled medicines, like bronchodilators & steroids,
- Getting oxygen from portable containers,
- Having lung reduction surgery to take out damaged parts of the lung,
- Getting a lung transplant, in some cases,
- Humidifying the air,
- Pulmonary rehab to assist you to learn how to live with your breathing problems & stay active.
Medical treatments
Depending on the severity of your condition, your treatment plan may consist of the following:
Bronchodilator: A bronchodilator is a type of medication that opens the airways in the lungs, making it easier to breathe. The substance is commonly breathed in through an inhaler, which is a device that pumps the medicine into the lungs. A doctor or other healthcare professional (HCP) will show you how to use your inhaler correctly so you get the most out of the bronchodilator.
Theophylline: Theophylline is an oral medication that relaxes the muscles in the airways so that they open up more. These assists relieve any breathing difficulties. A doctor or other healthcare professional (HCP) may prescribe theophylline if you have severe shortness of breath.
Steroids: If your symptoms do not improve with a bronchodilator or theophylline, a doctor or other healthcare professional (HCP) might prescribe steroids. These medications can be taken either with an inhaler or in pill form.
Pulmonary rehabilitation: Pulmonary rehabilitation is a program that is meant to improve your breathing and overall well-being. It sometimes consists of exercise, nutritional counseling, and breathing strategies. Certain programs also include counseling. You may also be referred to the pulmonary rehabilitation program at a hospital in your area.
Oxygen therapy: This is for serious cases, where your lungs are so damaged that blood oxygen levels are extremely low. You can inhale oxygen from the portable machine at home as required.
Specialized rehab program: If you are sometimes short of breath, rehab therapy can teach you ways to manage your disease. For example, you might learn a better way to breathe while you exercise.
Physical Therapy:
- Some postures, methods of coughing, and ways of striking the chest and back can help keep air passages clear of mucus.
- Some techniques can help people with bronchitis to keep their airways clear of mucus.
The physical therapist will be able to teach these techniques to the patient (and a family member or caregiver):
Postural drainage – prescribed positions that allow gravity to help in draining secretions from different areas of the lungs, making secretions easier to cough out.
Chest percussion – lightly clapping your chest and back to assist dislodge secretions.
Controlled coughing – techniques that assist you to cough up mucous.
Postural Drainage (PD)
- Postural drainage (PD) includes positioning a person with the assistance of gravity to aid the normal airway clearance mechanism.
- Postural drainage (PD) positioning varies based on specific segments of the lungs with a big amount of secretions.
- Postural drainage (PD) is the drainage of secretions, by the effect of gravity, from one or more lung segments to the central airways (where they can be removed by a cough or mechanical aspiration).
- Each position consists of placing the target lung segment(s) superior to the carina.
- Positions should commonly be held for 3 to 15 minutes (longer in special situations).
- Standard positions are modified as per the patient’s condition & tolerance warrant.
- Previous to determining the postural drainage (PD) position, it is very important to auscultate the lungs and identify the lung segments where added sound (Crepitus, Ronchi) is heard.
- Postural drainage (PD) can be facilitated with percussion and vibration in the postural drainage position.
Percussion
- Percussion is also referred to as cupping, clapping, and tapotement.
- The purpose of percussion is to intermittently apply kinetic energy to the chest wall and lungs.
- This is accomplished by rhythmically striking the thorax with a cupped hand or mechanical device directly over the lung segment(s) being drained.
Vibration
- Vibration includes the application of a fine tremorous action (manually performed by pressing in the direction that the ribs and soft tissue of the chest move during expiration) over the draining area.
- In this technique, a rapid vibratory impulse is transmitted through the chest wall from the flattened hands of the therapist by isometric alternate contraction of the forearm flexor & extensor muscles, to loosen & dislodge the airway secretions.
Coughing
- Coughing involves directed coughing and various assisted coughing techniques.
Forced Expiratory Techniques (FET)
- Forced expiratory techniques include diaphragmatic inspiration, relaxing the scapulohumeral region, and expiring forcefully from mid to low lung volumes whilst maintaining an open glottis (“huffing” exercises).
- It is more effective than coughing.
Lifestyle remedies: Making some lifestyle changes & trying natural remedies can also help alleviate the symptoms of chronic bronchitis.
You may want to consider the following:
- Breathing in warm, moist air from a humidifier can assist ease coughs and loosen the mucus in your airways. Make sure you wipe the humidifier regularly according to the manufacturer’s instructions. Bacteria and fungi can grow in the water container if it is not cleaned properly.
- Taking steps to limit the number of irritants you inhale may also assist reduce inflammation and coughing. For example, if you smoke cigarettes, cutting back may be helpful. If you live in an area with high levels of air pollution, consider wearing a medical mask whenever you go outside. You should also wear a mask if you work in an industry where you are exposed to paint or household cleaners with strong fumes.
- Physical activity can assist strengthen the muscles that help you breathe. Consider getting at least five minutes of movement a day, slowly increasing the length & intensity of your routine. If you are not sure where to start, you may find it helpful to consult with a doctor or other healthcare professional (HCP). They assist you to create an exercise plan that works for you.
- Pursed-lip breathing can sometimes provide relief when you are having difficulty breathing. In pursed-lip breathing, you take a deep breath and then gradually breathe out through your mouth. As you breathe out, hold your lips as if you are about to kiss. Doing this can assist regulate your breathing.
Lung transplant: A new lung or lungs may assist you to live longer.
What you can do?
Exercise: Just like with your biceps, you can build up the muscles that help you breathe. Try biking or walking three times a week. Workouts make you cough up mucus better.
Avoid bad air: Stay away from smokers. Do not step into crowds during flu season. Wear a face mask if you are working with things that have strong fumes, like varnish and house paint.
Get vaccinated: A yearly flu vaccine lowers your odds of a potentially deadly infection. Your doctor may also recommend you get the vaccine that protects you from pneumonia.
“Purse” your breaths: This trick makes it easier to breathe by opening up your airways. First, inhale through your nose to a count of two. Then pucker your lips as if you are about to kiss. Release your breath through your mouth to a count of four. Practice pursed breathing whenever you are in the middle of something hard, like climbing stairs.
What is the outlook for someone with chronic bronchitis?
- There is no cure for chronic bronchitis, but there are several treatments and therapies available to assist you to manage your symptoms.
- Certain lifestyle changes may also assist make you more comfortable.
The outlook for chronic bronchitis can differ significantly from person to person depending on variables such as:
- the severity of the disease,
- how well a person responds to treatment,
- a person’s overall health,
- whether a person has smoked or currently smokes tobacco,
- Following your healthcare professional’s (HCP’s) treatment advice can assist you to manage your condition & improve your quality of life.
When should you see a doctor or other healthcare professional (HCP)?
- Many people dismiss symptoms of chronic bronchitis, believing they simply have a smoker’s cough.
- However, it is important to contact your doctor right away if you have even the slightest suspicion that you might have bronchitis.
- Failing to receive timely treatment for chronic bronchitis greatly increases your risk of high lung damage, which can lead to respiratory problems or heart failure.
Call your doctor or other healthcare professional (HCP) right away if your cough:
- lasts longer than three weeks,
- prevents you from sleeping,
- is accompanied by a fever above 100.4°F (38°C),
- produces discolored mucus or blood,
- causes wheezing or shortness of breath.
How do you prevent chronic bronchitis?
- The most important thing you can do to reduce the risk of your chronic bronchitis is to avoid or stop smoking. Severe lung damage can happen when you inhale smoke over an extended period.
- If you quit smoking, your lungs will begin to heal and you will be able to breathe much easier.
- You will also lower your risk of developing lung cancer.
- Talk with a doctor or another healthcare professional (HCP) about quitting smoking or visit the American Lung Association website for tips.
- It is also important to avoid other lung irritants, including paint, toxic fumes, and dust.
- If you work in an industry where you are frequently exposed to such irritants, wear a mask over your nose and throat to help protect your lungs.
FAQs
Chronic bronchitis is a lower respiratory tract disease, defined by a productive cough that lasts for three months or more per year for at least two years. The cough is sometimes referred to as a smoker’s cough since it often results from smoking.
Chronic bronchitis is a condition that causes a productive cough that lasts for 3 or more months and happens multiple times over 2 years. There is no cure, but treatment may help to reduce the severity of symptoms. A person should talk to their doctor if they have a cough that lasts longer than a few weeks.
Chronic bronchitis is often part of chronic obstructive pulmonary disease (COPD). This is a group of lung diseases that cause airflow blockage and breathing problems. The most important cause of chronic bronchitis is cigarette smoking.
Smoking can increase a person’s risk of developing chronic bronchitis. According to the American Lung Association, chronic bronchitis and emphysema are the two conditions that commonly comprise chronic obstructive pulmonary disease (COPD). According to some reports, as many as 74% of people diagnosed with COPD have chronic bronchitis.
This condition causes a cough that’s often called a smoker’s cough.




3 Comments