Geriatric Diseases
Table of Contents
What is a Geriatric Disease?
Geriatric diseases, also known as age-related diseases or geriatric syndromes, refer to a group of health conditions that are commonly associated with aging. As individuals grow older, their bodies undergo various physiological changes, and these changes can increase the risk of developing certain diseases or conditions. Geriatric diseases often have multiple causes and complex interactions, making them challenging to diagnose and manage effectively.
Age-Related Medical Conditions & Illnesses
Introduction
- According to the World Health Organisation (WHO), heart disease, cancer, and cerebrovascular disease are responsible for about 75% of deaths in people over 65 in industrialized nations. According to UN estimates, there will be approximately 1200 million people aged 65 or older in the world by 2026, and millions of them are not receiving the proper healthcare they require because society and the government are not aware of the issue enough. Today, 1.1 million Indians, or 7% of the population, are over 60.
- The average lifespan has increased significantly for both males (>65 years) and females (>75 years), and it is predicted that by the turn of the century, India will have the largest population of elderly people.
- Therefore, nurses and other healthcare professionals need to be aware of how difficult it is to care for elderly patients.
Definition
Age-related issues are a global concern and a social need.
- This condition cannot be cured.
- People need to be protected during this stage from injuries, illnesses, and disabilities.
- Sir Jamessterling claims old age (genu) in GreeTreatment = lateraGeriatrics is the area of medicine that deals with the illnesses and conditions that affect the elderly and those who are aging. Gerontology is the in-depth study of aging and the issues that affect the elderly.
- Old age:
- The stage of life when physical and mental impairments start to show up more frequently than they did in earlier years.
- In the US, the elderly population is rising quickly In actuality, there will be three times as many seniors by 2050. Additionally, because older adults have a higher risk of develop
Various aging-related changes are common, such as difficulty in vision and hearing, hypertension, generalized muscle weakness, or osteoporosis. However, some health issues in older adults are not thought to be a normal part of aging. Geriatric medicine should be used to treat chronic conditions that affect kidney function, cause cognitive impairment, or otherwise degrade an elderly person’s quality of life.
Geriatric Diseases
- Geriatric medicine focuses on treating ailments that older people frequently experience. Treatment of older adults differs from that of their younger counterparts due to various factors, including polypharmacy, hazy symptom presentation, and difficulties with attribution in situations where multiple health conditions are present simultaneously.
- Additionally, age-related diseases that younger people typically do not develop are more likely to affect older adults. Although conditions like cardiovascular disease, ischemic heart disease, urinary incontinence, vascular dementia, multiple sclerosis, and other illnesses are much more prevalent in older adults, high blood pressure may be a problem that crosses generations.
Typical Chronic Diseases
While by no means an exhaustive list, these and other chronic diseases are among the more widespread ailments that affect older people:
Arthritis
Cancer
- persistent kidney disease
- lung disease that is chronically obstructed
- Alzheimer’s,
- Parkinson’s Diseases
- Dementia
- Diabetes
- Osteoporosis
- Stroke
- Arthritis
- One of the most prevalent age-related conditions affecting older adults is this chronic disease. Joint pain and ongoing inflammation are symptoms of arthritis. The two types are rheumatoid arthritis and osteoarthritis. Osteoarthritis, the more common of the two, is brought on by regular wear and tear. An autoimmune condition called rheumatoid arthritis causes the lining of the joints to be attacked by the immune system.
Although arthritis cannot be cured, it can be managed with painkillers and corticosteroids. These signs include:
- Joint ache,
- stiffness, and tenderness
- swelling around joints movement is limited or restricted.
persistent kidney disease
- Chronic kidney disease may be brought on by kidney infections, kidney inflammation, high blood pressure, or diabetes. There is currently no cure for this kidney condition, which can cause kidney failure. Another unfortunate fact is that the condition is typically only discovered through urine tests that have been requested for other medical conditions. The most effective treatment for chronic bronchitis is to stop smoking because it is one of the main risk factors for its onset. Along with rest, hydration, and the management of headaches, a healthy diet is crucial.
Bronchitis symptoms include:
- pain in the chest
- exhaustion, coughing productively
- Headaches
- sniffles or congestion
- Throat pain
Parkinson’s disease, Alzheimer’s disease, and dementia
A syndrome, or a group of chronic conditions, that affects older adults’ memory and cognition is referred to as dementia under the general term. This happens when the brain’s cells are harmed or lose their ability to communicate with one another, leading to their demise. Dementia symptoms include:
- No memory
- difficulty speaking
- clearly difficulties with vision or spatial awareness
- difficulty with logic or problem-solving
- Complex task management,
- critical thinking abilities, planning, and organization challenges
- the decline in motor function coordination
- Disorientation and confusion
- Behavioral shifts
- inappropriate conduct
- Depression, agitation, anxiety, and paranoia
- Hallucinations
Up to 70% of cases of a particular type of dementia are called Alzheimer’s disease. Alzheimer’s disease symptoms include the following and are brought on by unruly protein buildups in the brain:
- Having trouble recalling specifics of people, places, or events
- difficulty paying attention
- changes in one’s personality, such as apathy, mistrust, or aggression
- Depression and passivity
- Mood shifts
- Confusion
- impaired capacity for judgment or decision-making
- speaking, swallowing, or walking difficulties
Another form of dementia is Parkinson’s disease. The loss of brain nerve cells, which lowers the amount of dopamine required for typical cognitive function, is the underlying cause of this progressive disease. Despite the lack of treatment, the symptoms can be managed. pay attention for the following:
- Muscles that are rigid and unyielding cause certain body parts to shake uncontrollably moving slowly
- Diabetes Diabetic complications can arise in middle age and occasionally even earlier.
- It must, however, be managed as a lifelong condition since it most frequently affects older adults.
- The inability of the body to produce enough insulin to maintain normal function leads to this disease.
Osteoporosis
- One of the most prevalent diseases among older adults is osteoporosis. This condition often goes undiagnosed until a fall results in a break or fracture and manifests as a decrease in bone density.
- Losing bone strength is a natural part of aging, just like losing muscle mass, but people with osteoporosis notice this decline more quickly than the average person.
- Osteoporosis can be treated with medication and dietary supplements like calcium and vitamin D. Exercises that involve lifting weights and those intended to build muscle strength can also help older people manage their condition.
Stroke
- When the brain’s vital blood flow is interrupted, a stroke happens. This can result in permanent disability, the death of brain cells, and even pose a threat to life. Older adults are more likely than younger adults to experience strokes, so it’s crucial to be aware of the warning signs and symptoms so you can get help as soon as possible. It is simpler to remember thanks to the useful acronym (FAST).
Face: Does the face have a droop to one side?
Is the subject unable to raise both arms?
Slurred speech: Is it present?
Time: If so, get medical help right away. Do not waste any time.
Managing Chronic Illness
Chronic illnesses demand ongoing care because they are persistent and occasionally even permanent. To support them in achieving their health goals and maintaining their quality of life, older adults should think about putting a chronic care management team in place. This is particularly true for elderly patients who are simultaneously managing several chronic conditions.
Geriatric medicine will play a bigger role in older adults’ medical care as more of them experience age-related changes. A home healthcare team can assist older patients who are managing a chronic condition. Regular contact with reputable medical professionals can help prevent poor health in addition to healthy eating and a healthy lifestyle.
Sensory Changes
- loss of hearing Age-related increases in cerumen production and hearing loss (presbycusis) also affect hearing. Hearing loss is more common as people age and develop additional risk factors, and it is strongly correlated with a lower quality of life. Hearing impairment affects about 50% of adults over 85.
Speech processing can be hampered by mild hearing loss, especially if speech is spoken quickly or if there are many talkers in a large room creating reverberant noise. Therefore, environments, where people congregate, are those where verbal communication difficulties are most noticeable.
The observed relationships between hearing loss and depression, cognitive deterioration, and decreased quality of life are mediated by increased social isolation.
- The use of hearing aids could counteract negative effects on elderly adults’ quality of life and cognitive function. Unfortunately, only 14.6% of those with hearing loss who participated in one study said they were currently using a hearing aid. Frequently, these devices are not covered by health insurance.
- Vision Clarity Age-related presbyopia causes a normal decline in visual acuity.
- Older adults frequently experience glare issues, which increases the danger of nighttime driving. In the UK, a longitudinal survey of people aged 75 and older revealed that the prevalence of severe visual impairment peaked at age 90, when it rose to 37%, from 23% at age 85 to 89.
- At older ages, visual acuity deteriorates more quickly. The majority of the time, cataract surgery is risk-free and even beneficial.
- Vestibular Mechanism Falls are frequently caused by the multifactorial geriatric syndrome of dizziness. With age, vestibular function gradually deteriorates. Vestibular rehabilitation is another treatment option.
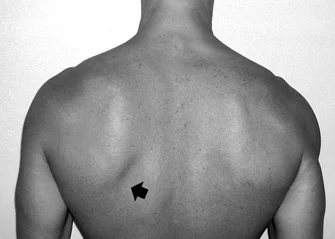
Strength of Muscle and Fat Changes
- Beginning in the fourth decade of life, muscle mass and strength begin to decline. Approximately 20% of people by the age of 85 have sarcopenia, which is characterized by a significant loss of muscle mass and strength. Sarcopenia is likely caused by a combination of factors including chronic inflammation, waning hormone levels, compromised mitochondrial function, and impaired muscle stem cell function. The decrease in muscle mass and rise in fat mass cause significant pharmacokinetic changes. Compared to younger adults, older adults might require lower medication dosages. Both muscle weakness and a swift decline in strength (14) indicate impending death.
Immunosenescence
- The immune system experiences a wide range of age-related changes, some of which are mediated by chronic inflammation and a persistently pro-inflammatory state. B cell function is declining, T cell generation is declining, T cell activation is changing, and innate immunity is malfunctioning (including reduced neutrophil function and chemotaxis and an unbalanced proinflammatory monocyte response). The body’s ability to fight infection is weakened by these modifications. For instance, older adults are more susceptible to influenza infections, which can be more severe and occur more frequently. Herpes zoster is more common in older adults due to cellular immune dysfunction. In general, older adults do not respond as well to vaccinations. The influenza vaccine may be more effective at high doses than at standard doses. Older adults who have chronically slowed inflammatory processes also have slower wound healing.
Urinary changes
- In older adults, the urinary bladder is frequently not sterile but rather is colonized with bacteria that do not cause infection. Women are more likely than men to have asymptomatic bacteriuria, and up to 50% of women in high-risk groups like long-term care facility residents and hospitalized patients experience this condition. Antibiotic use in this circumstance is inappropriate and could increase the development of antimicrobial resistance.
Somatic illness and several ongoing conditions
Chronic Heart Disease
- Despite a decline in death rates over the past 20 years, cardiovascular disease continues to be the leading cause of death in older adults. This group includes arrhythmia, congestive heart failure, and chronic ischemic heart disease. The oldest-old may have underdiagnosed ischemic heart disease. Vascular remodeling and vascular stiffness are characteristics of normal aging. Inflammation and additional vascular changes brought on by atherosclerosis increase the risk of cardiac and cerebrovascular events, peripheral vascular disease, cognitive decline, and other organ damage.
Cancer
- The second most common cause of death for older adults is cancer. However, the cancer death rate starts to decline by the age of 85. In this population, slow-growing tumors appear to be common.
- Functional status rather than age determines how well cancer treatment works. Aggressive cancer treatment should not be withheld from people in their ninth or tenth decade for no good reason.
- Breast cancer screening is not advised after the age of 75 due to a lack of benefit-related evidence, though it might be advantageous for women with long life expectancies. Similar to this, colon cancer screening for people over 75 is only advised in cases where there is a long-anticipated life expectancy and a strong perceived capacity to tolerate cancer treatment, if necessary. Life expectancy in older adults is quite variable at any age, depending on comorbidities and other factors.
- Prostate cancer screening is not advised due to the high frequency of burdensome false positives and the detection of slow-growing tumors.
- This is one of the most prevalent problems that older people deal with because there are more than 200 different types of cancer, including prostate cancer, breast cancer, and lung cancer. Cancer develops when cells in the body replicate quickly and abnormally, creating tumors that can spread through the bloodstream.
- Cancer treatment can be very invasive and has a significant negative impact on the body, despite the fact that many types of cancer now have cures. However, the likelihood of beating it increases with time after it is discovered. It is wise to think about performing routine cancer screenings. Here are some typical signs:
- finding a lump or mass unexpectedly
- mysterious weight loss
- A person’s stool, urine, vomit, or coughing may contain blood.
Osteoarthritis
- In older adults in America, osteoarthritis is the second most prevalent chronic condition and a leading contributor to chronic pain and disability. In one study, osteoarthritis was diagnosed in 52% of 85-year-olds. Women appear to be more likely than men to have osteoarthritis. Obesity is a risk factor for osteoarthritis, and the prevalence of severe hip and knee arthritis will rise as the population ages, especially as the overweight population does.
- Since virtually all analgesics have notable risks in older adults, pain management will continue to be a challenging clinical and health policy issue. Treatments for osteoarthritis also include pricy joint replacement surgery, which frequently comes with demanding rehabilitative therapies. The cause of low back pain is frequently multifactorial, and it is a common symptom, especially in older women. Nonpharmacologic therapies may be beneficial.
Diabetes Mellitus
- The disease’s most common form is type II diabetes. When the pancreas is unable to produce the necessary quantity of insulin, this occurs. The likelihood of developing diabetes can be decreased by making certain lifestyle changes, such as:
- a balanced diet
- a suitable weigh
- routine exercises
- With aging and rising obesity rates, diabetes rates have been rising. By 2050, there could be a 400% increase in the prevalence of diabetes among older adults in the United States. Even at the age of 85, diabetes is still a significant cardiovascular disease risk factor. Diabetes also increases the risk of peripheral neuropathy and peripheral arterial disease, which can lead to diabetic foot ulcers and amputations. 6% of diabetic patients experience diabetic foot ulcers each year, and 0.5% require amputations Diabetes management techniques that are specific to each patient should be used.
- Sulfonylureas and insulin use in frail older adults should be carefully considered because of the significant risk of hypoglycemia they carry. For patients taking hypoglycemic medications, going from the hospital to their home or receiving post-acute care can be risky because their dosing requirements may change. For people with diabetes, routine foot exams are essential to preventing amputations. Walking frequently can enhance leg circulation.
Osteoporosis
- Osteoporosis is the normal aging-related loss of bone density. Osteoporosis, a more severe weakening of bone density, affects many adults over the age of 85. While osteopenia is unrelated to an increased risk of bone fractures, osteoporosis is. For women over 65, bone density testing is advised. The importance of osteoporosis screening for men has not been conclusively proven, despite the fact that the prevalence of fractures in men increases by the age of 85. Supplementing calcium and vitamin D to prevent fractures is still debatable in terms of its efficacy and safety.
Several Chronic Illnesses
- The prevalence of multiple chronic conditions is rising due to population aging and rising diabetes rates, with 62% of Americans over 65 having more than one chronic condition. The majority of health spending is on older people who have several chronic conditions. This population should be the focus of research and quality-improvement efforts in order to enhance care and lower costs.
Physical Activity
Functional changes that come with aging are a result of both typical age-related changes and accumulated pathology.
Walking speed
- Normal aging causes a decline in walking speed, but diseases also cause additional declines. Measurements of walking speed can be used to forecast future community ambulation, falls, disability, and mortality risk. It is quick, safe, doesn’t call for any specialized equipment, and doesn’t significantly increase the cost of clinical care to measure walking speed. According to one study, men in the 85–89 age group walk at an average speed of 1.1 m/s and women at an average speed of 0.8 m/s. Mean walking speeds for men and women fell to 0.9 m/s and 0.8 m/s, respectively, after age 90. Interventions involving exercise can quicken walking.
Mobility Impairment
- According to a US Census study, 73% of Americans over the age of 85 have some difficulty walking. Disability-related to mobility is linked to depression, falls, and social isolation. Over 85 and disabled, one-third of residents live alone.
Disability
in Daily Living Activities Adults over the age of 85 have comparatively high disability rates. Disability rates increase with age over 80 in both instrumental daily living activities like cooking and activities like dressing and bathing. Typically, difficulty bathing comes before difficulty dressing or using the lavatory. According to one study, 25% of people over the age of 85 had trouble using the loo and 75% of those over the age of 85 had trouble bathing. Disability-related issues are frequently compounded by ongoing pain, depression, and difficult medication schedules. In recent decades, there has been a slight decline in the proportion of older adults with disabilities.
Falls
- Among older adults, falls are a significant contributor to morbidity and disability. Every year, 30–40% of adults over 70 experience a fall, and rates are especially high for senior citizens living in long-term care facilities. More than half of injuries among older adults are caused by falls. Adults over the age of 85 have higher fall-related death rates than people of other ages. The incidence of falls has been shown to decrease with physical activity, vitamin D supplementation, balance training, and home safety assessment as part of a multifactorial fall prevention program. A multifactorial fall risk assessment should be done on people who have balance issues or frequently fall.
Frailty
- Weakness, sluggishness, exhaustion, and weight loss are all signs of fragility, which is defined as a particular susceptibility to stressors. In one study, 38% of those between the ages of 85 and 89 were frail. It is simple to determine a person’s level of fragility, and this fragility predicts future disability, falls, hospitalizations, and subpar surgical results. Targeted interventions for frail populations would probably consist of reviewing medications as well as physical activity and nutritional components.
Continence
- Urinary incontinence affects 30% of women over 65 and 50% of senior citizens living in nursing homes. Overactive bladder, stress incontinence, and functional incontinence are common causes of incontinence in women. Reduced quality of life and well-being are effects of urinary incontinence. Common incontinence drugs, however, have troublesome side effects.
Psychological and cognitive aging
- By the age of 85, mild short-term memory loss, trouble finding words, and slower processing speed are common signs of aging. Driving safety can be impacted and the risk of financial exploitation is increased by changes brought on by normal brain aging. Additionally, these changes may make it more difficult to comprehend complex medical information. Genetic and social factors (such as education and occupation) may be protective against brain aging because it does not occur at a uniform rate. Dementia is not caused by aging normally in the brain.
- Not all mental abilities deteriorate with aging. It is well known that wisdom and knowledge increase with normal aging, which helps to explain why community elders should be treated with respect. Aging may also lead to an increase in empathy and altruism.
Dementia
- With advancing age, dementia rates rise. Alzheimer’s disease has a higher mortality rate than cardiovascular disease, which has a lower mortality rate. The number of people with dementia may increase globally from 47 million in 2015 to 131 million in 2050. In 2015, the estimated global cost of dementia was $818 billion, and by 2030, that cost is projected to reach $2 trillion. Despite the fact that medications for dementia are only marginally effective, screening may still be beneficial for public health.
- Numerous elderly people with dementia may be living or driving dangerously and may have unmet needs. The Folstein Mini-Mental State Examination is the most frequently used dementia diagnostic tool, but it has some drawbacks, including an adjustment for educational background. For instance, the mean MMSE score for 85-year-olds with poor education was 25.2 while the mean score for 85-year-olds with good education was 28.0 in the Irish Longitudinal Study on Ageing. To increase safety and independence, people with dementia require opportunities for cognitive stimulation, carer support, and perhaps assistive technologies.
Depression
- Depression is not a typical side effect of getting older. The loss of physical, social, or cognitive function as a result of illness, bereavement, retirement/income loss, and other aging-related life events can all cause grief. Throughout adulthood, major depression is common, but after age 60 and again after age 80, the incidence rates start to decline.
- Adults over 85 have twice as many depressive episodes as those between 70 and 74. Older adults and people with disabilities who are institutionalized frequently experience depression. Aggressive approaches to diagnosis and treatment are required to lessen suffering, improve general functioning, and prevent suicide. The majority of older American adults who commit suicide are white men over the age of 85.
Social/Environmental
- Marriage and wealth are indicators of longer survival. The advantages of marriage appear to be greater for men than for women. In contrast, social isolation among older adults is a predictor of mortality and other unfavorable outcomes. 5% of senior citizens are housebound, rarely leaving the house other than for crucial doctor’s appointments. The majority of these seniors are over 80. During a natural disaster, these elderly people are particularly vulnerable because they live alone and are in poor health.
- Even at advanced ages, the majority of older people reside in the neighborhood. In American households, there will be two times as many people over the age of 80 by 2035.
- Over the age of 85, about 13% of women and 8% of men reside in nursing homes or other institutional settings. These rates have decreased in recent years, most likely as a result of fewer disabilities and better in-home care options. Institutionalization can be reduced further by providing support for at-home carers and promoting at-home medical and social work services. In 2011, more than 17 million Americans provided family care for an elderly person. Being a carer is typically a long-term commitment, though the precise number of hours required varies significantly depending on the needs of the care recipient. Most care must be given to elderly people with dementia. Formal training, peer counseling, stress management, legal counsel, and employment flexibility are all resources for helping family carers.
Medical Decisions
initiating or stopping medications, ordering screening tests, sending people to the hospital, and suggesting to families about placement or end of the life care are complex discussions that health providers have with people over the age of 85. frequently family members play a central role in these complex discussions. The patient may have a hearing impairment or hearing problem, cognitive impairment, or communication impairment. Life expectancy is frequently a major consideration; however, numerous patients are skeptical of life expectancy estimates and don’t like to talk about it .
Polypharmacy
A single patient who uses five or more medications concurrently is said to be polypharmacy. The likelihood of a negative drug reaction or drug-drug interaction increases significantly when taking five medications. The risk of falls, disabilities, and other undesirable outcomes is increased by polypharmacy. When deciding whether to start or stop medication in patients over the age of 85, healthcare providers must consider the time to benefit, burden, risks of adverse effects, and goals of care.
Hospitalization
People over 85 are more likely to be hospitalized, and this is linked to functional decline. More urgent home care could aid in avoiding hospital complications like functional decline and iatrogenic infections. Medication errors and readmission to the hospital can be reduced with transitional care and prompt post-hospital medical follow-up visits.
Placement in Institution
Many senior citizens value being able to age in place in their own homes. Interventions carried out at home may halt the progression of a disability and avert the need for institutionalization. In conversations with families, all possible living arrangements are discussed, and after that, preferences and safety are evaluated.
Physiotherapy Treatment in Geriatric Diseases
What is the role of physiotherapy in geriatrics?
As we age or grow older, our bodies experience numerous physical changes. As a result of these modifications, muscle strength typically declines, joints become stiffer and falls and fractures occasionally result. Exercise, however, might be the secret to helping elderly people resume living. Physiotherapists are skilled professionals who help to lower the risk and effects of illness by identifying the factors that prevent the elderly from being active.
ailments that geriatric physical therapists treat Numerous musculoskeletal, neurological, and cardiopulmonary issues can occur in elderly people.
- Aching from persistent conditions Physiotherapy can aid in easing pain brought on by ailments like osteoporosis or arthritis.
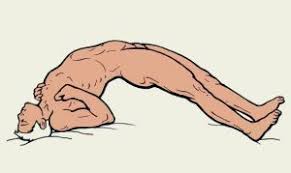
- Enhancing power and flexibility Reduced strength and flexibility with age are one of the most prevalent problems that almost everyone encounters.
- To prevent stiff muscles, stretching the lower back, hip flexors, and other areas can help to improve alignment and joint mobility.
- Their various stabilities while walking, standing, changing directions, and other activities are maintained with the aid of a balanced and regular exercise routine. These balance drills include marching, shifting your weight, tandem walking, and others.
- Exercise for the lower body can keep your body strong. So, if your physical condition has improved, you can try some of these exercises, such as leg lifts, sit-to-stands, and step-ups.
- Some common causes of pain and immobility loss include depression, sleep deprivation, diabetes, congestive heart failure, and medication side effects. A physiotherapist can help. Physiotherapy aids in regaining life strength. 3. Stability in Posture Age-related balance issues are brought on by the loss of normal bone and muscle function. Exercises for balance are part of the physiotherapy programme for people with neurological conditions like Alzheimer’s disease, ALS, Parkinson’s disease, or brain injuries.
4. Reducing the chance of a fall The most common accident type among elderly people that results in bone fractures and other injuries is falling. medical background Medical history It’s crucial to get a complete picture of a patient’s medical and surgical history, as well as their drug use, especially if they take any medications that may have a major impact on their mobility or risk of falling.
- Social background Historical Social, The informal or formal support of family and friends is frequently needed by active older adults.
- Physical therapy procedures Exercises, workouts, and the use of electric modalities like ultrasound, TEN, and shock wave therapy are all part of physiotherapy. Moderate-intensity exercise like brisk walking is advised. Stretchy bands can also be used to perform muscle-strengthening exercises against resistance!
- Goals Goals are crucial for keeping therapy person-centered and coordinating treatments. Rather than acting as a passive carer for an elderly person, goals should be focused on managing and improving a condition.
- Physiotherapy for the chest for ICU patients The thoracic cage’s musculoskeletal structures, lungs, and airways make up the respiratory system. A gas exchange occurs during respiration between the atmosphere, lungs, blood, and body tissues. This system’s job is to keep the body’s supply of oxygen flowing and remove carbon dioxide. Mechanical ventilation might be required if any respiratory system component fails.
The critically ill in the intensive care unit (ICU) frequently have respiratory dysfunction because they are confined to their beds, which causes general deconditioning that affects many body systems, including the respiratory system. Pulmonary complications are the main reason for hospital morbidity, so they are a major concern for ICU patients. Reduced lung volumes and expiratory airflow rates, weakened respiratory muscles, decreased lung and chest wall compliance, and impaired gas exchange are all common side effects of bed rest. The patient’s work of breathing increases as a result of all of these factors, which also raises the possibility of pneumonia and atelectasis. The cough mechanism may be hampered by the weakened respiratory muscles and the decreased tidal volume, raising the risk of pulmonary complications.
Physiotherapy for Pulmonary Diseases: Objectives
- Clearance of airway secretions
- Maintenance or improvement of oxygenation.
- Lung volume recruitment or atelectasis improvement
- Maintaining or increasing the strength of the inspiratory muscle Physiotherapy • Modalities for Airway Clearance • Modalities for Respiratory Care • Nebulization • Assisted Cough Techniques • Positioning (Postural Drainage) • Manual Chest Techniques (Percussion, Vibration, and Shaking) • Airway Suctioning (Open/Close) • Forced Expiratory Manoeuvre (Coughing/Huffin)
FAQ
The following are the most common ailments that older persons face:
Heart problems. Heart disease is the leading cause of death in adults aged 65 and up. … Diabetes…. Skin Issues…. Gastrointestinal Issues…. UTI or Urinary Tract Infection.Arthritis.
Significant Challenges To Expect When Caring For The Elderly Problems With Mobility And Everyday Tasks. People’s agility and mobility naturally deteriorate as they age… Navigating Healthcare… Deciding On Your Loved One’s Care… Mental Issues… Financial Matters… End-Of-Life Planning.
Geriatric assessments should involve a thorough medical history and physical examination, with a particular emphasis on issues unique to the aged, such as vision, hearing, diet, fall prevention, urine incontinence, osteoporosis, and preventative health
A review of the literature revealed that the five most common geriatric complaints are pressure ulcers, incontinence, falls, functional decline, and delirium.
Takeaways should be written down or printed.
Recognize that persons from various origins may have varying expectations.
It promotes good aging in older persons by preventing and treating diseases and impairments that typically accompany aging. Geriatric nursing is providing assistance to elderly persons at their homes, hospitals, or specific institutions such as nursing homes, psychiatric institutions, and so on.
The purpose of preventative geriatrics is to promote a condition of health that allows for the longest possible active life while retaining high levels of function. The physician’s responsibility in promoting such a state of health includes disease prevention and the management of aging-related chronic diseases.
Frailty, sarcopenia, functional decline, failure to thrive, frequent falls, incontinence, and inability to ambulate are all related to generalized weakness. Many of these disorders share common risk factors, related symptoms, and diagnostic markers.
Communication Strategies for Elderly Patients
Speak to the patient as if he or she were an adult.
Make older patients feel at ease.
Avoid rushing elderly patients.
Speak clearly…
Variation in older persons, Maximising activity in older adults are three main aspects to consider in geriatric rehabilitation. The idea is that optimal health is inextricably linked to optimal functional capacity.
More than half of all persons aged 65 and up have three or more chronic medical conditions, such as heart disease, diabetes, cancer, or arthritis.
From a chronological standpoint, medical treatment for the elderly (geriatrics) begins at the age of 65.
Geriatric medicine physicians and care teams assist older persons in improving their quality of life, particularly as they negotiate the often complex medical issues associated with aging.
The area of physiotherapy that deals with the care of senior citizens is known as geriatric physiotherapy. An important part of a physiotherapist’s job is to help older people maximize their body’s ability to improve mobility and independence.