Tibial Tubercle Osteotomy
Tibial tubercle osteotomy (TTO) is a surgical procedure performed on the tibia bone in the lower leg. It involves making a controlled cut in the tibial tubercle, which is the bony prominence located on the front of the tibia, just below the knee joint. The tibial tubercle is the attachment site for the patellar tendon, which is responsible for straightening the knee.
The bony protrusion on the anterior medial side of the tibia (shin bone) is called the tibial tubercle. It functions as a fulcrum for knee extension and as an attachment for the patellar tendon. The tibial tubercle is frequently too far lateral, or toward the outside of the knee when there is patellar instability or dislocation. The knee cap may dislocate as a result of this outside the lateral margin of the trochlea.
A surgical treatment called tibial tubercle transfer (TTT), also referred to as tibial tubercle osteotomy (TTO), or Fulkerson osteotomy, is used to treat the lateral displacement of the tibial tubercle. Enhancing patellar tracking and stability, reducing discomfort, and relieving strain on the cartilage are the objectives of the procedure.
TTT was initially discussed as a therapy for patellar instability in the early 1900s. With the development of numerous new procedures throughout the years, it has subsequently become a routine orthopedic treatment. These days, repeated patellar dislocation or subluxation, persistent patellofemoral discomfort, and patellar instability brought on by a lateralized tibial tubercle are the most typical indications for TTT.
Depending on the particular pathology being treated, the tibial tubercle is moved from its original place to a new site on the tibia using a surgical method. The new patellar tendon attachment site is often positioned immediately medial and slightly anterior to the original position.
Table of Contents
What is Tibial Tubercle Osteotomy?
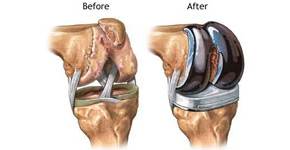
In addition to other surgical techniques, tibial tubercle osteotomy is a technique used to treat osteoarthritis, patellofemoral discomfort, and patellar instability. In a challenging primary or revision total knee arthroplasty, this approach is quite safe and offers great access and surgical exposure. When physical therapy and other nonsurgical treatments have failed and there has been a history of multiple knee dislocations, surgery is the recommended course of action. During the tibial tubercle transfer technique, the patella (knee cap) is realigned such that it slides directly into the center of the femoral groove. The tibial tubercle is a protrusion on the front of the shin bone. The tibial tubercle is moved medially, toward the inside of the leg, to address patellar maltracking. This lessens discomfort by removing pressure from the knee cap’s sensitive areas.
An individual may need a Tibial Tubercle Osteotomy if they have patellofemoral instability or patellar maltracking. The patellar tendon’s insertion location on the tibia is modified during a tibial tubercle osteotomy. Tibial tubercle osteotomy is also used by surgeons during total knee replacement and knee replacement revisions.
Tibial Tubercle Osteotomy Surgical Technique
Tibial Tubercle Osteotomy Surgical Technique
The procedure is done under general anesthesia, and a person will be completely unaware of the surgery until they wake up in the recovery room. At first, knee arthroscopy will be performed to check the inside portions of the knee joint. It involves tiny incisions or portals through which tiny devices are inserted, and a video camera is used to examine the patella tracking, analyze the patella cartilage, and observe the architecture of the knee joint.
Tibial tubercle osteotomy and transfer are done through an incision made in the front of your leg, just below the patella. In the osteotomy surgery, an 8–10 cm long periosteal incision is created 1 cm medial to the tibial tubercle. An oscillating saw is used to make medial and distal incisions that are both close to the tuberosity. The possibility of tibial fracture is eliminated by the distal cut’s tapered form. Similarly, a proximal cut is performed using the proper tools, such as a reciprocating saw or a curved osteotome. The lateral periosteum is not severed and an osteotomy is then conducted through the bone cortex. The osteotomy segment is attached to the lateral periosteum at this location. This results in the creation of an 8–10 cm long, more than 2 cm wide, and more than 1 cm thick portion of the tibial tubercle. It should include the whole patellar tendon insertion. The tibia segment is then levered with the aid of an osteotome to allow access to the medullary canal.
The osteotomy segment is then placed into a position that ensures correct tracking of the patella bone while being seen clearly. Arthroscopically, the tracking pattern can be verified. Then, using screws that can be later removed if they irritate the joint, the mobilized bone is secured into its new location.
For whom is a tibial tubercle osteotomy appropriate?
Patients with uncomfortable patellar maltracking or patellofemoral instability (PFI) are treated with tibial tubercle osteotomies. The patella’s misalignment in the trochlea of the femur (the thigh bone) can be fixed by repositioning the bone (the tibial tubercle), which also reduces arthritis symptoms and eliminates feelings of instability. Patients with patellar maltracking frequently experience persistent anterior knee pain. This frequently shows up as pain when climbing and descending stairs, as well as when sitting for extended periods of time. Only patients whose patellofemoral joint does not already have bone-on-bone osteoarthritis can benefit from tibial tubercle osteotomies.
TTO can be carried out in conjunction with cartilage repair surgery or medial patellofemoral ligament reconstruction (MPFL reconstruction). While the operation is carried out to treat instability in patients who have an unstable kneecap, it is also carried out to lessen arthritic symptoms in people who require this procedure. In other words, while a knee arthroscopy or this operation cannot cure arthritis, it can greatly lessen its symptoms by lessening the stresses acting on the patella.
Indications for Tibial Tubercle Transfer
When the patella moves off the lateral surface of the femur, a very complicated condition known as patellofemoral instability results. Orthopedic surgeons evaluate the overall situation rather than basing their surgical choices just on one factor. Recurrent patellar subluxation or dislocation, persistent patellofemoral discomfort, and patellar instability brought on by a lateralized tibial tubercle are the three most typical indications for tibial tubercle transfer.
The tibial tubercle-trochlear groove distance (TTTG) is the most popular method for determining the lateralization of the tibial tubercle. In contrast to anything more than 20mm, which is considered TTT, normal TTTG levels fall between 10 and 12mm.
Other, less frequent signs include:
- Patella alta, which occurs in patients with recurrent patellar instability and refers to the patella being excessively high on the femur.
- Loss of patellofemoral cartilage with or without a treatment to restore the tissue
- Trochlear dysplasia is characterized by an excessively shallow groove in which the kneecap rests.
- Symptomatic, full-thickness patellofemoral chondral or osteochondral lesions
- Previous failed patellofemoral cartilage restoration procedure
- Young individuals who are not candidates for arthroplasty can use the salvage technique.
- BMI
Contraindications:
- Medial or lateral knee osteoarthritis in Kellgren-Lawrence grade 3 or 4.
- Untreated patellofemoral instability (severe trochlear dysplasia, patella alta, and increasing TT-TG distance)
- Uncorrected lower extremity coronal/sagittal plane malalignment
- Ligamentous instability of the tibiofemoral joint
- Inflammatory arthritis
- Patient factors (smoking, drug, alcohol use, etc.)
What might a patient anticipate following a tibial tubercle osteotomy?
After surgery, a patient will have a brace on their leg to keep it straight when they awaken. When they are moving around, it will be crucial that they wear this brace at all times. You are not required to sleep with your brace on. Crutches will also be provided, and for the first six weeks, you are only permitted to bear a specific amount of weight on the injured leg. The rehabilitation protocol will provide a more detailed explanation of this. This implies that they will always use two crutches to walk, relying solely on the weight of one leg to maintain balance.
Once your pain is fully under control, most people can return home after one to two days. You can visit with physiotherapists during this hospital stay, receive some early exercise, and practice using crutches.
How will the discomfort after the procedure be managed?
To ease your pain during surgery, a local anesthetic will be given around the knee. While you are unconscious, the anesthetist will frequently administer a nerve block, a different anesthetic. This has a big impact on lowering the level of discomfort you feel. Long-acting analgesic medications will also be provided to you to lessen your pain. You’ll be given an oral painkiller prescription when you leave the hospital. The most frequently given drugs are breakthrough painkillers like Endone, routine panadol, and anti-inflammatories like Celebrex. After the third week, you’ll start cutting back on your painkiller use until just before physiotherapy and right before bed. Most people won’t need to use painkillers after six weeks.
Post-surgery Care Following Tibial Tubercle Osteotomy
Following surgery, you can experience light to moderate knee soreness for a few days or weeks. You’ll be given a prescription for oral painkillers to help manage your discomfort. Maintain an elevated position with the operated leg and apply ice to the area for 20 minutes. Both swelling and pain are reduced as a result. You’ll wear a leg brace that can only be taken off when you’re using the continuous passive motion (CPM) machine and sitting with your leg raised. Exercises from physical therapy should be carried out as they aid in restoring mobility. Consume nutritious foods and get enough water.
Risks and Complications of Tibial Tubercle Osteotomy
The following are the rare risk of the surgery:
- Compartment syndrome
- Deep vein thrombosis
- Infections and
- Delayed bone healing.
Physiotherapy treatment:
The rehabilitation parameters are laid out in a progression plan based on criteria. While average time frames are provided, individual patients will recover at varying rates based on their age, accompanying injuries, health status before the injury, compliance with rehabilitation, tissue quality, and degree of injury. To safeguard the surgical repair or reconstruction as well as the healing tissues, specific time limits, limitations, and precautions may also be advised. It shouldn’t be used in place of clinical judgment when determining how a patient’s post-operative course should develop based on their physical exam results, personal progress, and/or the presence of post-operative problems. If the therapist has any queries or concerns, they should speak with the recommending doctor. Disabilities that led to the initial issue require special attention. In the case of a patient who has undergone partial medial meniscectomy and has a varus alignment, for instance, post-operative rehabilitation should focus on addressing muscular imbalances or postures that put undue stress on the medial compartment.
(0–6 WEEKS AFTER SURGERY) PHASE I: IMMEDIATE POST-OP
Rehabilitation Goals:
- Protect the anatomic repair
- Monitor wound healing
- Minimize knee effusion
- Increase tibial-femoral and patella-femoral mobility
- Restore quadriceps control
- Gradually extend ROM in accordance with recommendations.
Precautions
- No active knee extension
- No resisted closed or open chains for the first six weeks after surgery.
Weight Bearing
- Week 0–4: NWB(Non-weight bearing)/TDWB brace locked in extension
- Weeks 4-6: TDWB with brace locked in extension moving to PWB
- If have full extension and good quadriceps control, progress to brace unlocked in PWB (Partial weight bearing).
- If you have adequate quadriceps control and full extension, you can advance to brace unlock in PWB.
Brace
- Up until at least four weeks after surgery, when complete knee extension has been obtained and strong quad control, the hinged knee brace must be locked in the 0 degrees extension position for all motion and gait.
- The brace may be released when seated or in bed.
Interventions
Range of Motion:
- Knee AAROM/PROM – Passive extension only
- Week 0-4: 0-90 degrees
- Week 4-6: 0-120 degrees
- Sitting knee flexion with P/AAROM for knee extension, supine knee extension with heel prop, heel slides with PROM for knee extension, and prone hangs
Strengthening
- Quad sets
- Gluteal sets
- Ankle pumps
- Side-lying hip ABD with a brace until quad lag is gone
- Prone Hip Extension – braced until quad lag is gone
- SLR – per doctor’s advice, although depending on the surgical technique, may not be appropriate 150
- When performing without a lag, use a D/C brace with the brace locked in extension.
- Side-lying hip adduction with a brace until the quad lag is gone
- Clamshell
- Hamstring stretch
- ITB stretch
- Gastroc-soleus stretch
- Bike – No resistance
Aquatic therapy – if available:
- Deep water walking and ROM exercises (chest/shoulder height).
- Core stability and UE exercises
Manual Therapy
- Patella mobilizations – immediately post-op
- Gentle STM – 2-3 weeks post-op
Modalities
- NMES for quadriceps re-education and biofeedback
- Cryotherapy for swelling and pain management
- Taping: pain and swelling management
Criteria to Progress
- Knee PROM: 0-120 degrees
- Adequate pain control
- Minimal swelling
- Able to perform Straight Leg Raise without quadriceps lag
PROTECTION PHASE: PHASE II (7–12 WEEKS AFTER SURGERY)
Rehabilitation Goals:
- Increase mobility
- Restore quadriceps control
- Full ROM restoration by weeks 8–12.
- Improve weight bearing
- Normalize gait without an assistance device with a target of 2 miles at a rate of 15 minutes per mile on a treadmill
- Gradual advancement of balance, stretching and strengthening exercises dual progression of therapeutic exercises for strengthening, stretching, and balance
Precautions:
- Avoid ascending and descending stairs back-to-back until appropriate quadriceps control is shown by SLR, which should not occur until week 8.
- Avoid deep squats and resisted open chain terminal knee extensions, which have significant patella-femoral compression stresses.
- Avoid medial collapse by engaging in strengthening and functional exercises.
- Wait 4-6 months after surgery before engaging in running, leaping, or plyometrics.
- Avoid overloading the surgical site. Modify activity level if increasing discomfort, edema, or catch occurs.
Weight Bearing
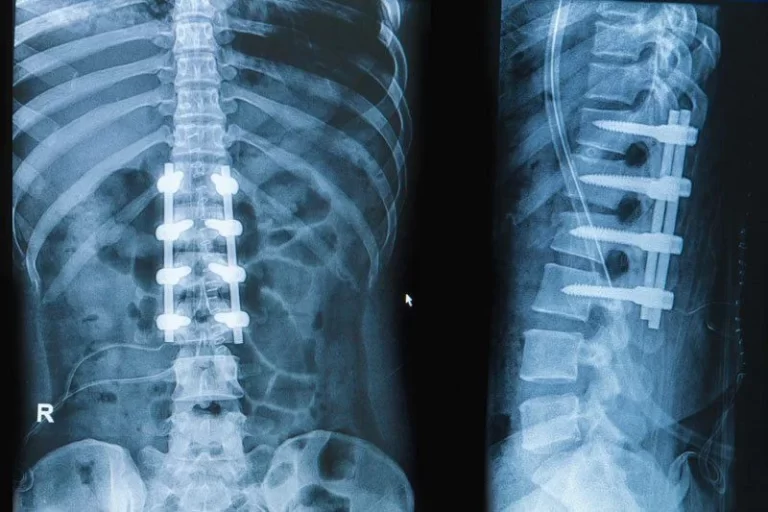
- WBAT as prescribed by the doctor, depending on X-ray
Brace:
- If there is good quad control, leave the brace unlocked and use crutches as necessary.
- Up until week 8, wear a hinge brace; after that, switch to a patellofemoral brace with a lateral buttress.
Additional Interventions:
Continue with Phase I interventions as needed
Modalities
- As needed, NMES for quadriceps re-education
- Cryotherapy for edema and pain management
Manual Therapy
- Patella mobilizations
- Soft tissue mobilization
Range of Motion
- Progress PROM/AAROM/AROM of the knee as tolerated
Stretching
- Hamstring
- Gastroc -Soleus
- Prone Quadriceps with strap
Strengthening
- TKE(Total knee extension) – 0-40 degrees
- Leg press
- Partial range wall squats
- 0-45 degrees
- Forward step-ups, Lateral step ups
- Forward, Lateral, Retro step downs
- Bridge with physioball
- Romanian Deadlifts – Week 7
- Stand upright with your weight just below your knees.
- Band walks – Week 8
- Stool walks – Week 8
- BOSU Partial squat – Week 9
- 0-60 degrees
- Prone Hamstring curl – 10 weeks
- Start with ankle weights before moving on to a weight machine.
- Cardiovascular Exercise
- Stationary Bike – light resistance
- Treadmill – forward and backward
- Elliptical – week 9-10
Aquatic Therapy
- Flutter kicks
- Straight leg scissor kicks
- Running in waist-deep water
Balance:
Converting from a two- to a single-legged balance
Progress from static to dynamic:
- BAPS
- Ball toss
- Body blade
- Fitter
- Slide board
Criteria to Progress
- Full range of motion
- Elimination of swelling
- Restoration of normal gait
- Quad strength > 70% of uninvolved leg
Advanced strengthening in Phase III (13–16 weeks after surgery)
Rehabilitation Goals
- Normal tibial-femoral and patella-femoral mobility
- Restoration of quadriceps control
- Increase your muscle endurance, strength, and balancing exercises.
Precautions
- No plyometrics, jogging, or leaping until 4-6 months after surgery
- A patellofemoral hinged brace may be worn for lighter-level activities up to 12 months after surgery, per the recommendation of the doctor.
Additional Interventions
Continue with Phase I-II Interventions
Strengthening
- Total leg strengthening
- Single leg strengthening
- Hamstring isotonic exercises through full ROM
- Quadriceps isotonic exercises
Proprioception
- Single leg balance
- Stable and unstable surfaces
- Single-leg balance with leg swings
- Single leg balance with ball toss
- Single leg balance with UE perturbations
Cardiovascular Exercise
- Bike, elliptical
- Treadmill Walking Criteria to Progress
- Full, symmetrical pain-free ROM
- Strength: 80%+ of uninvolved leg
- Satisfactory clinical exam
- MD permission to move on to the following stage
PHASE IV: EARLY RETURN TO SPORT PHASE
(16+ WEEKS AFTER SURGERY) Rehabilitation
Rehabilitation Goals:
- Increase the degree of activity based on functional requirements and MD approval.
- Resuming work, leisure, and/or athletic pursuits.
- If necessary, run 2 miles at a leisurely pace. Additional Interventions
Additional intervention:
Continue with Phase III interventions
Running: begin at 4 months
- Start with light gentle slow-paced running
- Treadmill running
- Must run for five minutes with proper form and a rhythmic foot strike that can be heard.
- Aquatic running
- Backward and forward running
- Initiate Return to running protocol
Plyometrics: 4.5 –to 5 months
- Start with double-leg drills
- Progress slowly to single-leg drills
- Maintain adequate posture and hip and knee alignment.
Agility Drills: 4.5 to 5 months
- Sub-max foot placement drills
- Ladder drills
- Line hops
Criteria to Progress:
Return to sport/play: 7 to 9 months
- Quad and hamstring strength 90% of uninvolved
- Full symmetrical knee range of motion
- No knee joint effusion
- A single-leg hop test results in 90% limb symmetry.
- 90 percent limb symmetry on the triple hop test.
- 90% limb symmetry on the cross-over hop test
- Refer to lower extremity functional assessment
Conclusion:
The risk of future chondral and soft tissue injury increases with each episode of patellar instability, despite the fact that the incidence of the condition is not exceptionally high (43/100,000). The risk of recurrence and danger of additional soft tissue and cartilage injuries can be reduced by prompt diagnosis and treatment of this condition. By minimizing an otherwise abnormal and unstable patellofemoral joint, a tibial tubercle osteotomy can effectively alter the natural history of lateral patellar instability, keep the athlete active, and possibly reduce the risk of developing patellofemoral osteoarthritis.
Although excellent results can be obtained, this technique is not without risk. Risks include anterior skin necrosis, infection, and hardware complications/irritation. Complications include delayed healing and nonunion. The purpose of the tibial tubercle osteotomy must be the main consideration during preoperative planning. This surgery is widely used to correct for patellar maltracking and consequent patellar instability—or a combination of both—because it is advised for off-loading the patellofemoral joint in the presence of chondral injury or osteoarthritic alterations. As a result, selecting the right patients becomes crucial.
FAQs:
How successful is a tibial tubercle osteotomy?
The underlying cause of the tibial tubercle transfer affects the tibial tubercle osteotomy’s success rate. A medial patellofemoral ligament reconstruction (MPFL) is often performed concurrently with other procedures, and in these situations, the success rate of the surgery is thought to be higher than 80%.
What are the different types of tibial tubercle osteotomy?
The medialization osteotomy (Elmslie-Trillat) and AMZ osteotomy (Fulkerson) are the two osteotomies that are most frequently employed.
What are the risks of tibial osteotomy?
The most frequent side effects, despite the modest risk, are:
Infections.
Clots of blood.
The knee joint is stiff.
Damage to the nerves and vessels.
Osteotomy that did not heal.How long is a TTO surgery?
Two screws are inserted to anchor the bone in its new position; if the patient finds the screws irritating, the screws may be taken out later. The surgery takes around an hour to complete, and the incision needed to execute the procedure is about 3 inches long.
What is the success rate of TTO surgery?
90% success rate for surgeries. Can resume their regular activities more quickly.