Os trigonum Syndrome
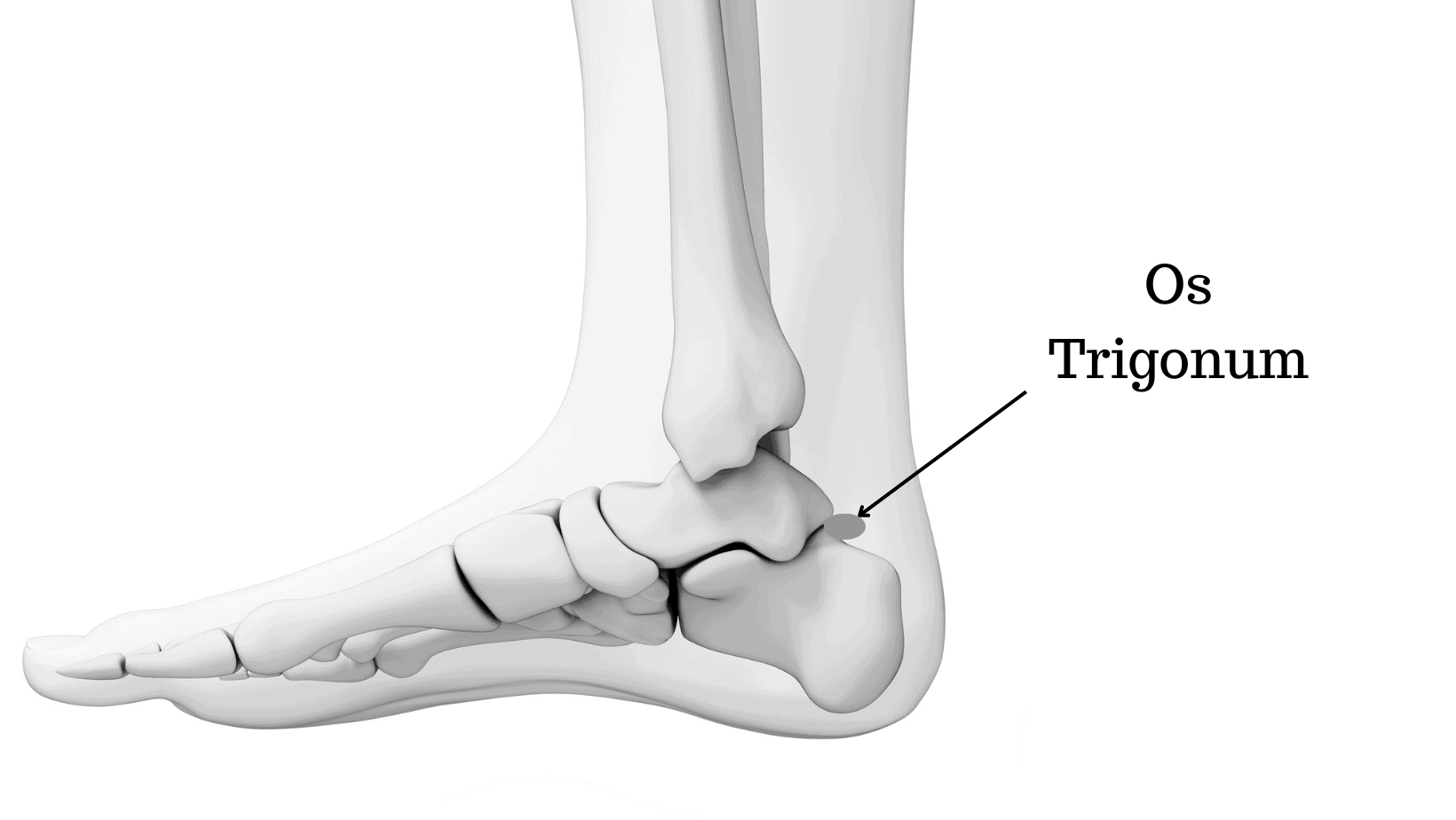
OS trigonum syndrome, also known as posterior ankle impingement syndrome, is a condition characterized by pain and inflammation in the back of the ankle. It is caused by the presence of an extra bone called the os trigonum, which is located behind the talus bone in the foot.
Three bones make up the actual ankle joint, which enables movement and weight bearing. The talus, or heel bone, is one of these bones. The os trigonum is an additional bone that can grow below the talus in some people. There may be no symptoms from this extra bone. But in certain people, especially after repeated downward toe pointing, it can lead to the painful disease known as os trigonum syndrome.
Table of Contents
Clinically Relevant Anatomy
The body of the talus and the posterior talar process are different ossification centers from an embryological perspective. The posterior talar process manifests as a distinct ossicle called the os trigonum between the seventh and thirteenth years of life. Normally, it unites with the talus within a year of its formation, however, 7% of adult humans still have this OS trigonum. Its borders may be smooth or serrated, and it may be bilaterally or unilaterally present. The os trigonum is typically viewed as a single bone, however, it can also come in pairs or more. The size is less than 1 cm, but it might vary.
The anterior, inferior, and posterior surfaces of the os trigonum are typically triangular in shape. A cartilaginous synchondrosis links the anterior surface to the lateral tubercle. The calcaneus and the inferior side may articulate. Although not articular, the posterior surface serves as a point of attachment for capsuloligamentous structures. The os trigonum can also be round or oval in shape.
The flexor hallucis longus tendon is located in the sulcus between the medial and lateral tubercles, medial to the os trigonum.
What is Os Trigonum Syndrome?
The “nutcracker phenomenon” is what is referred to as “the nutcracker phenomenon” when it causes pain posterior to the ankle and decreased plantarflexion. This additional ossicle, along with the nearby soft tissues, can become trapped between the tibia, talus, and calcaneus when an os trigonum is present. The affected structures may become inflamed as a result of this.
The talar compression syndrome, symptomatic os trigonum, and posterior tibial talar impingement syndrome are other names for the os trigonum syndrome.
Ankle discomfort that develops at the rear of the ankle is known as os trigonum syndrome. An additional bone behind the ankle bone is the cause of this ache. Os trigonum syndrome is a common name for the disorder because of the additional bone. Additionally known as:
- Posterior ankle impingement syndrome.
- Hindfoot impingement syndrome.
- Nutcracker-type impingement (Because pointing your toes downward compresses the os trigonum).
- Posterior tibiotalar impingement syndrome.
- Talar compression syndrome.
Os trigonums are congenital, meaning the extra bone is present from birth. Either one or both feet could be affected. The os trigonum is immobile because it is joined to your talus bone (the lower portion of your ankle joint) by a thick cartilaginous tissue. An os trigonum affects 15–30% of persons, and the majority of those who have one don’t exhibit any symptoms.
Posterior implies behind. Impingement is another word for pressure or pinching.
Epidemiology /Etiology
An os trigonum can develop by one of three mechanisms:
- Ossification center fusion failure
- Fracture of the tibia’s posterior edge
- Fracture of the talus’s posterior process.
The syndrome cannot be caused by just having an os trigonum. It must go along with a horrific experience.
Overuse or trauma might result in the os trigonum syndrome. Ballet dancers and runners are most likely to discover it when it results from overuse. Running downhill and performing an “en pointe” or “demi-pointe” position both cause a strong plantar flexion, which compresses the ankle joint’s posterior surface. Forced plantarflexion might shift the os trigonum as a result of trauma.
The ankle joint capsule and encircling ligaments are examples of soft tissue components that may respond by developing a hypertrophic mass.
Causes and risk factors:
Os Trigonum Syndrome may manifest if the unfused bone is present in addition to an ankle injury. It is typically brought on by one of the following:
Os trigonum syndrome is a congenital condition that can affect one or both ankles and is present at birth. While the exact cause of this condition is unknown, overuse and acute injuries, such as sprains, are known to be major contributing factors.
When someone possesses an additional bone and injures the attachment, such as with a sprained ankle, Os trigonum syndrome results. And it frequently happens when your ankle experiences repeated stress, such as:
- Ballet dancers: A dancer-like habit of frequently pointing the toes downward.
- Soccer players: Kicking a ball over and over again as a soccer player would.
- Basketball players
- Like a runner, pushing off the back of the ankle.
- Other types of dancers and athletes
- Overuse: caused by repetitive plantarflexion (foot pointing down). Runners, football players, and ballet dancers are frequently afflicted by Os Trigonum Syndrome.
- Trauma: an ankle injury caused by severe plantar flexion of the foot
- The unfused Os Trigonum bone and the surrounding soft tissues can become jammed between the ankle and heel bones (tibia, talus, and calcaneus), resulting in what is described as a “nutcracker injury” (nutcracker fracture). Pain and stiffness result from the inflammation of the soft tissues. Os Trigonum Syndrome is brought on by a soft tissue irritant.
When someone points their toes, the bone becomes squeezed, stretching and rupturing the fibrous attachment, which usually results in pain. Bruising and soreness are brought on by the motion.
The excess bone becomes squeezed or pulls away from its attachment site as a result of trauma or misuse. This may stretch and rip the tissue in the area, resulting in discomfort, inflammation, and symptoms.
Os Trigonum Syndrome is solely tied to activities; neither a particular age nor gender is more prone to it.
Signs and Symptoms of Os trigonum syndrome:
Pain in the rear of the ankle, especially while moving or pointing the toes, is the most typical sign of os trigonum syndrome. In most cases, this also causes irritation and inflammation. Moving one’s big toe may also cause discomfort. This is due to the big toe tendon’s proximity to the os trigonum. Pain frequently gets better with rest and worsens with action.
Another typical reason for posterior ankle impingement is the os trigonum. When someone complains of pain at the back of their ankle, this is referred to. In specifically, when a person hyperextends their ankle, it frequently happens when the top of the foot points away from the leg.
The first sign of the syndrome is a load-dependent, enduring ache between the peroneal tendons and the Achilles tendon. In this area, stiffness, weakness, and edema are also apparent. Reduced plantarflexion compared to the untreated ankle is the second significant symptom. The bony protrusion may occasionally be audible.
Movements involving eversion or inversion could be uncomfortable. Plantarflexion of the foot or dorsiflexion of the great toe will cause pain towards the back of the ankle.
Because an os trigonum rarely causes issues, the majority of people who have one are unaware of it.
However, individuals with os trigonum syndrome will experience symptoms in the rear of the ankle, such as:
Pain, especially while pointing the toes downward or pushing off the big toe.
- Pain: A deep, throbbing ache in the rear of the ankle that is particularly noticeable when pointing the toes downward or pushing off with the big toe when walking
Decreased range of motion (foot’s ability to move less fully). - Tenderness: When touched, the area feels delicate
Stiffness.
Swelling: Swelling may occur as a result of soft tissue inflammation. At the ankle’s back
Sensitivity to touch. - Foot pain: Ankle pain on the back of the foot is typical. The discomfort usually worsens with plantarflexion (pointing the toes) during the push-off stage of walking and subsides with rest.
- Tenderness: The ankle’s rear and outside side are typically sensitive to touch.
- Lump: A person might occasionally be able to feel a little, firm lump close to the Achilles tendon. This bone is not fused.
- Some sufferers of this disorder alter their gait when they run, kick, dance, or otherwise exert themselves. They might be doing this knowingly or unconsciously.
However, altering the foot’s normal position could result in pain or discomfort in other body parts. For instance, when elevating onto the toes, a ballerina with os trigonum syndrome may spin the foot inward or outward. However, over time, this may result in toe, leg, knee, or hip pain.
Normally, just one foot is afflicted, but around one-third of the time, both feet are.
Diagnosis:
In order to evaluate ankle discomfort, a clinician will:
Ask you about the signs and your daily routine.
Examine the medical background, mentioning any injuries.
In order to determine what hurts and what doesn’t, move, stretch, rotate, and flex the foot and ankle.
A talus fracture or an Achilles tendon injury are two conditions that share symptoms with os trigonum syndrome. Imaging studies are frequently requested by medical professionals to establish the existence of the os trigonum and rule out alternative reasons. These tests could consist of:
- X-ray: Lateral view X-ray, mainly in a weight-bearing position, with the foot in full plantar flexion.
- MRI: The optimum method for determining the presence and size of the ossicle, concurrent diseases, and soft tissue and bone injury is magnetic resonance imaging (MRI). Flexion/extension MRI provides details regarding the os trigonum’s movement.
- CT scan.
- Ultrasound.
Os trigonum syndrome frequently exhibits signs that resemble those of other diseases and injuries. Similar kind of symptoms can be seen in the following conditions:
- Ankle sprain
- Achilles tendon injury
- Talus fracture
A doctor will frequently check a patient’s medical history and do a physical examination when they appear with symptoms. They’ll probably enquire as to when and how the pain first appeared. This could assist in eliminating some possible causes.
An X-ray or other imaging test will probably be requested by a medical practitioner in order to identify the source of the pain. On the imaging exam, they ought to be able to see the os trigonum and establish the proper diagnosis.
Examination:
Pain and swelling may be felt while palpating between the Achilles tendon and peroneal tendons on the posterolateral side.
The passive forced plantarflexion test should be performed using fast, repeating hyper plantarflexion movements in neutral alignment, maybe accompanied by exo- or endorotation movements at the moment of maximum plantarflexion. Thus, the ossicle between the tibia and the calcaneus is ground.
Differential Diagnosis:
Although Os Trigonum is a relatively uncommon cause of foot discomfort, there are several other disorders that exhibit symptoms very much like Os Trigonum:
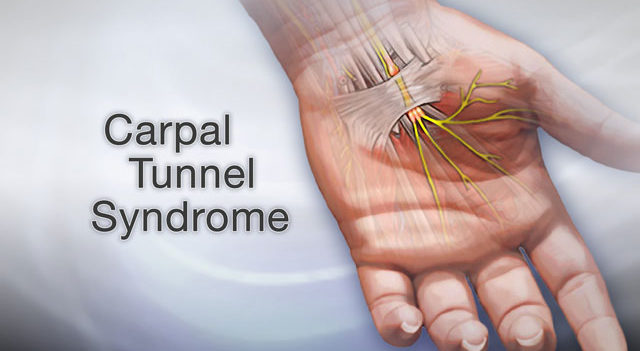
- tarsal tunnel Syndrome
- Heel bursitis
- Achilles tendonitis
To ensure you receive a correct diagnosis, it is crucial to seek medical guidance.
Recovery Process:
If treatment is initiated quickly after an acute episode of os trigonum syndrome, recovery typically takes 4-6 weeks.
It may take considerably longer for things to calm down if symptoms have been present for a few months or if you are an extremely busy person, especially a sports player.
Resting from all activities that aggravate your symptoms is crucial, and once they have completely subsided, you should resume your previous activities very slowly to avoid your symptoms returning.
Treatment of Os trigonum syndrome:
Treatments that may involve a combination of the following can frequently relieve the symptoms:
Simple nonsurgical techniques are the first step in anterior impingement syndrome ankle treatment. Treatment options could combine:
- A few days of abstinence from the painful activity.
- To strengthen your feet and legs’ muscles or restore ankle alignment, try these at-home exercises or physical therapy.
- To lessen swelling, apply ice many times each day.
- Use of a walking boot to immobilize the injured limb and limit foot and ankle motion while the damage heals.
- NSAIDs, or non-steroidal anti-inflammatory medications.
- injections of steroids.
- For the majority of patients with posterior ankle impingement, these techniques work. However, surgery can be required if you still experience discomfort after receiving treatment for several months in order to engage in some activities.
The os trigonum and surrounding tissue can be surgically removed (resected) either arthroscopically or with an open incision. Athletes typically return to full activity levels within six months of recovery, which takes one to two months.
Treatments that may involve a combination of the following can frequently relieve the symptoms:
The primary goal of os trigonum treatment is to promote soft tissue healing so that the inflammation can subside. This is accomplished by combining:
The recommended course of treatment for os trigonum is rest, ice, compression, and elevation.
- Rest. To allow the inflammation to go down, it’s crucial to keep the wounded foot off the ground.
- Ice. Applying an ice pack to the affected area and covering it with a light towel reduces swelling.
- Compression: Compression reduces swelling
- Elevation: Elevation also reduces swelling.
Immobilization. A walking boot is frequently used to limit ankle motion and promote the healing of the affected tissue.
To give the inflammation time to subside, it is strongly advised that you completely abstain from all activities for four to six weeks. A walking boot may be prescribed to you to wear to prevent your ankles from moving while you are moving around.
Applying ice to the back of the ankle on a regular basis also helps to lessen swelling and inflammation. Learn how to use ice therapy in a secure and efficient manner by visiting the ice section.
2. Medicine
Your doctor could advise you to take NSAIDs like ibuprofen, which are anti-inflammatory drugs, to aid with the discomfort and swelling associated with os trigonum syndrome. Before taking any new drug, always with your doctor or pharmacist.
Drugs taken orally. Ibuprofen is one example of a nonsteroidal anti-inflammatory medicine (NSAID) that may be useful in lowering pain and inflammation.
Injections. To lessen the discomfort and inflammation, cortisone may occasionally be injected into the affected area.
3. Injections of steroids:
Injections of corticosteroids are occasionally used to treat pain and inflammation. On our sister site’s injections page, you can read more about how they function and common side effects.
Injections of corticosteroids or nonsteroidal anti-inflammatory drugs are used to lessen inflammation in soft tissue.
For 4-6 weeks, a below-knee cast is utilized in cases of fracture.
4. Workouts:
Working with a physiotherapist on a rehabilitation program of stretching and strengthening exercises can also be very beneficial.
By making the foot and ankle muscles stronger, the talus will be able to go forward more easily during plantarflexion, which will relieve pressure on the Os Trigonum and prevent irritation of the soft tissues.
5. Surgery:
Surgery to remove the fragment of bone may be indicated if symptoms continue. Physiotherapy should be used as a follow-up to this. After four to eight weeks, you can typically resume athletic activities with a full resolution of symptoms as the conclusion.
The os trigonum and any soft tissue causing discomfort are often removed during surgery by making tiny incisions on either side of the Achilles tendon using keyhole procedures. Since it is not required for ordinary foot function, it should aid in symptom relief.
Surgery is used if the symptoms don’t go away. (High evidence; positive outcomes are mentioned in all research.)
The os trigonum must be taken out in order to do this. Following surgery, we put on a plaster cast for five days. Physiotherapy is then started and lasts for 4 to 8 weeks.
Sports activities can thereafter be resumed in their entirety. Up to 6 months will pass before a full recovery.
Physical Therapy Treatment of Os trigonum Syndrome:
Inflammation can be reduced with rest, cold, and massage.
Modalities:
Ultrasound, IFT (Interferential Therapy)
Exercises:
Strengthening exercise for lower-leg muscles. Strengthen with the help of weight cuffs, dumbbells, and theraband.
Several physical therapy activities can help gradually improve the ankle’s range of motion. A person must heed the advice given to them by their doctor. The following are some exercises that can help strengthen the ankle:
- Towel scrunches:
Repetitions: 20 every day
Muscle: The plantar fascia is mostly engaged.
Your toes and the top of your foot should feel this workout.
Resources required: An hand towel
Detailed instructions:
- Put a little towel on the ground in front of you as you sit with your feet flat on the ground.
- Relax after grabbing the towel’s center with your toes and curling it in your direction. Repeat.

- Ankle eversion and Ankle inversion
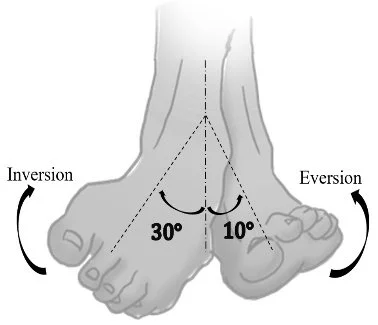
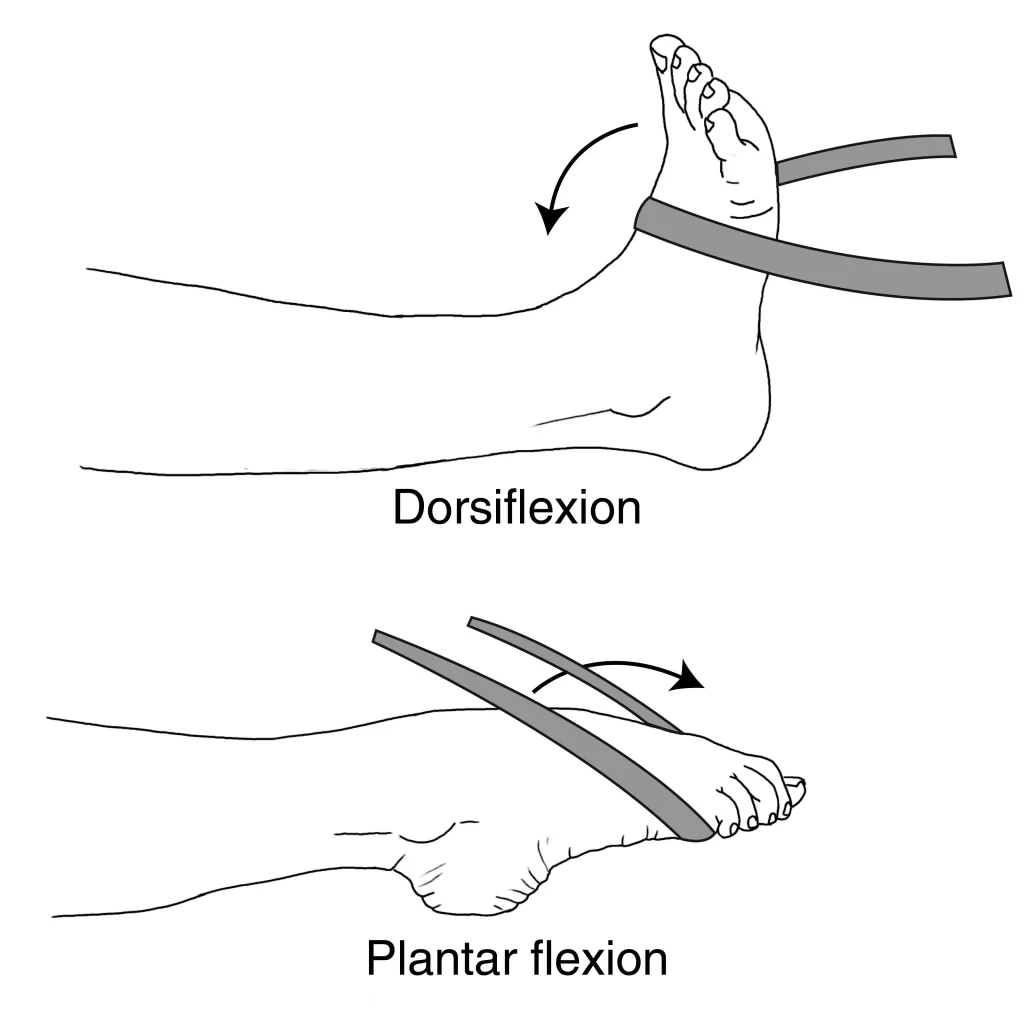
- Plantar flexion and Dorsiflexion
Repetitions: Three sets of ten days per week.
Principal muscles engaged: Gastrocnemius-soleus complex and anterior tibialis
This exercise should feel good in your calf, shin, back of your heel, and top of your foot.
Resources required: Use a comfortable resistance elastic stretch band.
Step-by-step directions:
- Sit on the floor with the legs extended in front. A person can perform this workout while seated on a chair as well.
- Anchor the elastic band to a table or chair leg, then wrap it around your foot to perform dorsiflexion. Return to the starting posture slowly by pulling your toes in toward you. Repeat.
- Wrap the elastic band over your foot and hold the ends in your hands to perform plantar flexion. Point your toes gently, then slowly revert to the starting position. Repeat.
- Tip Maintain a straight leg with your heel on the ground for stability.
- Tibialis posterior exercises
- Heel raises

- Seated toe taps
- Calf raises:
Repetitions: Several Times 2 sets of 10 days a week, from days 6 to 7.
Muscle: Gastrocnemius-soleus complex is the major muscle group used. Your calf should feel this exercise.
Resources required: chair for assistance
Detailed instructions
- Put equal weight on each of your two feet as you stand. Hold on to the back of a chair or a wall for support to maintain your equilibrium.
- Your unaffected foot should be raised off the ground such that the affected foot bears all of your weight.
- As high as you can, lift the heel of the affected foot, then bring it back down.
- Repeat.
- Tip: Your working leg’s knee should not be bent. Start with both legs if necessary, then switch to the injured leg when you can.
Stretching using eccentric and isometric movements.
Additionally, specific exercises are recommended to enhance deep muscle activity during plantarflexion.
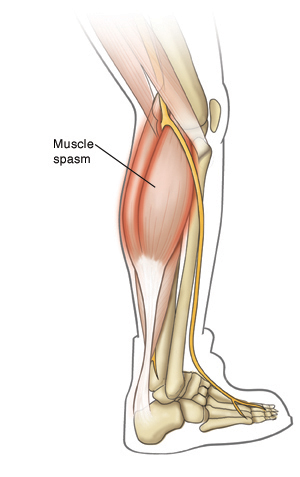
The M. gastrocnemius is opposed by the deep muscles of the lower leg, such as the tibialis posterior, flexor digitorum longus, flexor hallucis longus, and the peroneals. In contrast to employing the M. gastrocnemius, which results in raising the calcaneus and compressing the os trigonum, engaging the deep muscles causes the talus to be pushed forward during plantarflexion, which will lessen the effect of the os trigonum on the posterior tibia.
Developing the deep muscles. holding the calcaneus in position with the hands while performing demipointe and en pointe. 90-degree knee flexion will stop the M. gastrocnemius from contracting.
Additionally, tilt-board proprioceptive exercises are used to treat lower limb misalignments. Only one study, which had 11 dancers with posterior ankle impingement, including 6 people with an os trigonum, incorporated all of these activities. Nine of them responded well to these workouts, while the other two required surgical removal.
A recent systematic review found that physiotherapeutic therapies can be used to treat injured ballet dancers since they have favorable impacts in a number of areas, such as pain, range of motion, and functional status. However, while thinking about physiotherapy options for treating injuries in a ballet dancer, one should proceed with caution due to the scant available evidence and methodological limitations of this review.
Conclusion:
Os trigonum is a supplementary bone located behind the ankle. Many individuals with this extra bone don’t experience any symptoms. However, clinicians refer to the os trigonum as os trigonum syndrome if it causes pain.
Health professionals are now unsure of what triggers the development of this bone. However, overusing the ankle, especially in people who dance or play sports, is a common risk factor for causing discomfort. Pointing the toes down generally causes pain.
Initial therapies frequently include rest, ice, immobility, and potential painkillers. If they don’t work, surgery might be necessary. Os trigonum syndrome might take weeks or even months to fully recover from.
FAQs:
What does os trigonum pain feel like?
The common symptoms of Os Trigonum Syndrome include ankle discomfort and stiffness, which are frequently made worse by toe pointing. You may notice some swelling and a little, sensitive lump behind the ankle that is frequently present.
Is os trigonum syndrome rare?
People who have an os trigonum bone may develop the uncommon and painful ailment known as os trigonum syndrome. About 15 to 30 percent of persons have an accessory (extra) bone in at least one foot called the os trigonum. Located right behind the ankle joint, it is a little, spherical bone.
What is os trigonum surgery called?
The surgical removal of an os trigonum using an open posteromedial approach with concurrent FHL tenolysis/tenosynovectomy is a secure and efficient procedure that enables the detection and treatment of accompanying FHL disease.
What age is os trigonum for?
The posterolateral side of the talus is home to the accessory bone known as the os trigonum. It manifests as a secondary ossification nucleus that typically fuses in less than a year between the ages of eight and eleven.
How long is os trigonum recovery?
After posterior ankle arthroscopy and os trigonum excision, athletes typically need eight to 12 weeks to return to play, however, this period can vary.