Craniotomy
Table of Contents
What is a Craniotomy?
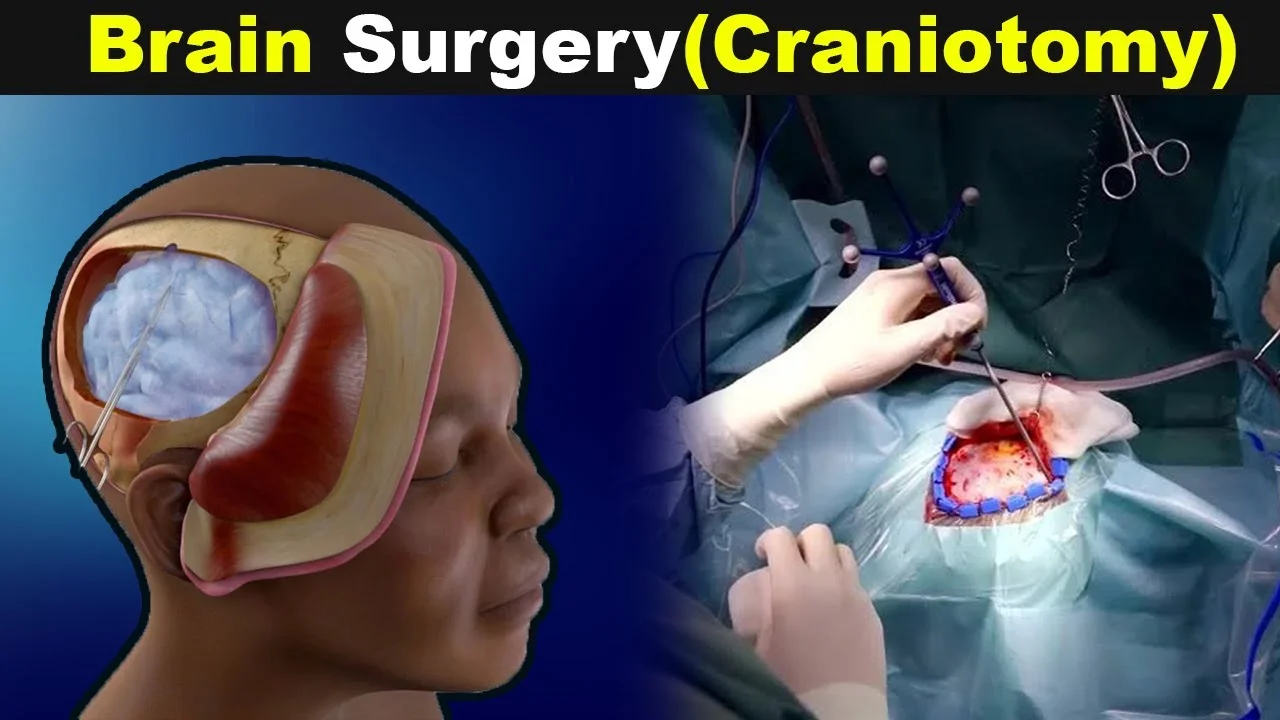
- A craniotomy is the surgical removal of part of the bone from the cranium to expose the brain.
- Specialized tools are used to remove the section of bone called the bone distraction. The bone delirium is temporarily removed, and also replaced after the brain surgery has been done.
- Some craniotomy procedures may use the guidance of computers and imaging (magnetic resonance imaging [MRI] or computerized tomography [CT] reviews) to reach the precise position within the brain that is to be treated. This technique requires the use of a frame placed onto the cranium or a frameless system using superficially placed markers or landmarks on the scalp. When either of these imaging procedures is used along with the craniotomy operation, it is called a stereotactic craniotomy.
- reviews made of the brain, in confluence with these computers and localizing frames, give a three-dimensional image, for example, of a tumor within the brain. It is useful in producing the distinction between tumor tissue and healthy tissue and reaching the even situation of the abnormal tissue.
- Other uses contain stereotactic biopsy of the brain (a needle is guided into an abnormal area so that a number of tissue may be removed for testing under a microscope), stereotactic aspiration (removal of fluid from abscesses, hematomas, or excrescencies), and stereotactic radiosurgery (similar as gamma cutter radiosurgery).
- An endoscopic craniotomy is another type of craniotomy that involves the insertion of a lighted compass with a camera into the brain through a small incision in the cranium.
- Craniectomy is an analogous procedure during which a portion of the cranium is permanently removed or replaced later during an alternate surgery after the swelling has gone down.
- Craniotomy involves a surgeon removing a piece of the cranium to pierce the brain for brain surgery. They may perform craniotomy for reasons, including:
- Removing a brain tumor
- Repairing an aneurysm
- Removing a blood clot
- Treating epilepsy
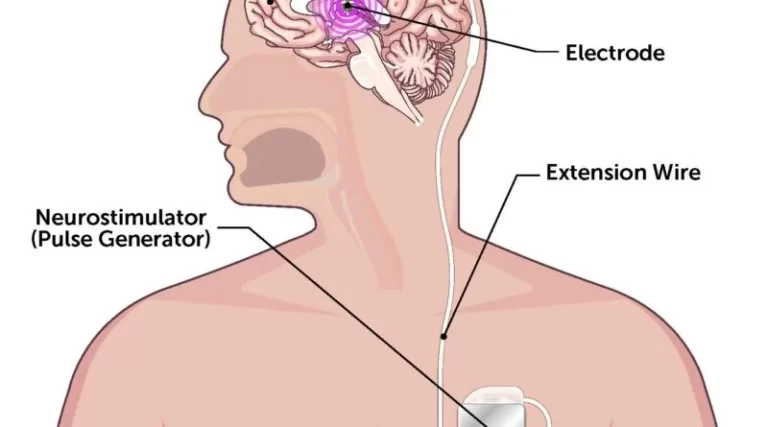
- Implanting stimulator devices
- Repairing Cranium fractures
- Positioning a tear in the membrane lining the brain
Types of Craniotomy
- Extended Bifrontal Craniotomy
- Minimally Invasive Supra-Orbital “Eyebrow” Craniotomy
- Retro-Sigmoid “Keyhole” Craniotomy
- Orbitozygomatic Craniotomy
- Translabyrinthine Craniotomy
- Stereotactic Craniotomy
- Endoscopic Craniotomy
- Keyhole Craniotomy
- Awake Craniotomy
- Frontotemporal Craniotomy
- Posterior Fossa Craniotomy
Extended Bifrontal Craniotomy
- The extended bifrontal craniotomy is a traditional cranium base approach used to target sensitive tumors toward the front of the brain. It is grounded on the concept that it is sure to remove extra bone than unnecessarily manipulate the brain.
- The extended bifrontal craniotomy involves making an incision in the scalp behind the hairline and putting off the bone that forms the figure of the pathways and the forepart. This bone is replaced at the cutoff of surgery. Temporarily removing this bone allows surgeons to create space between and right behind the eyes without holding to unnecessarily manipulate the brain.
- An extended bifrontal craniotomy is generally used for those tumors that are not an applicant for removal by minimally invasive approaches because of either the deconstruction of the tumor, the possible pathology of the tumor, or the aims of surgery.
- Types of tumors treated with extended bifrontal craniotomy involve meningiomas, esthesioneuroblastomas, and mean cranium base tumors.
Minimally Invasive Supra-Orbital “Eyebrow” Craniotomy
- Supra-orbital craniotomy (frequently called “eyebrow” craniotomy) is a course used to remove brain tumors. In this procedure, neurosurgeons make a slight incision within the eyebrow to pierce tumors in the front of the brain or around the pituitary gland, which is deeper in the brain behind the nose and eyes. This way is used rather than endonasal endoscopic surgery when a tumor is actually large or close to the optic nerves or vital arteries.
- Because it is a minimally invasive course, supra-orbital “eyebrow” craniotomy may offer
- Less pain than open craniotomy
- Faster recovery than open craniotomy
- Minimal scarring
- The supra-orbital craniotomy may be part of the treatment for Rathke’s split tumors, cranium base tumors, and some pituitary tumors.
Retro-Sigmoid “Keyhole” Craniotomy
- Retro-sigmoid craniotomy (frequently called “keyhole” craniotomy) is a minimally-invasive surgical procedure achieved to put off brain tumors. This procedure allows for the removal of cranium base tumors through a slight incision behind the ear, giving access to the cerebellum and brainstem. Neurosurgeons may use this way to reach certain tumors, similar to meningiomas, aural neuromas (vestibular schwannomas), cranium base tumors, and metastatic brain tumors.
- Benefits of “keyhole” craniotomy include minor pain after the procedure than after an open craniotomy, minor scarring, and a more rapid-fire recovery.
Orbitozygomatic Craniotomy
- The orbitozygomatic craniotomy is a traditional cranium base way applied to target sensitive tumors and aneurysms. It is grounded on the conception that it is sure to remove extra bone than unnecessarily exploit the brain.
- generally used for those lesions that are too complex for removal by further minimally invasive ways, orbitozygomatic craniotomy involves manufacturing an incision in the scalp behind the hairline and removing the bone that forms the figure of the route and impertinence. This bone is replaced at the close of surgery. Temporarily removing this bone allows surgeons to pass deeper and more difficult parts of the brain while minimizing severe injury to the brain.
- Brain tumors that may exist treated with orbitozygomatic craniotomy involve craniopharyngiomas, pituitary tumors, and meningiomas.
Translabyrinthine Craniotomy
- A translabyrinthine craniotomy is a procedure that involves making an incision in the scalp behind the ear, also removing the mastoid bone and some of the inner ear bone (especially, the semicircular channels which contain receptors for balance). The surgeon also finds and removes the tumor or as much of the tumor as achievable without risk of severe injury to the brain.
- When there is no useful hearing or hearing is to exist sacrificed, the translabyrinthine way is frequently considered for the removal of aural neuromas. During the translabyrinthine craniotomy, the semicircular canals of the ear are removed in setup to pierce the tumor. perfect hearing loss occurs as a result of the removal of the semicircular canals.
- Although the hearing is lost with the translabyrinthine craniotomy, the risk of facial nerve damage may exist reduced.
Stereotactic Craniotomy
- Still, it’s called a stereotactic craniotomy, If a craniotomy uses an MRI or CT scan
- In this operation, your surgeon uses imaging tests to produce three-dimensional images of your brain. It allows them to differentiate between healthy and abnormal tissue.
- Stereotactic methods also help your surgeon find the best spot for a scalp incision. This makes it simple to make minor cuts and perform minimally invasive procedures.
Endoscopic Craniotomy
- In an endoscopic craniotomy, your surgeon makes a tiny incision in your cranium. They insert an endoscope, which is a little lighted device with a camera. This method is much used with keyhole craniotomies.
Keyhole Craniotomy
- A keyhole craniotomy is operated on to remove brain tumors. It’s a minimally invasive surgery that’s associated with minor scarring and a shorter recovery time.
- Your surgeon makes a minor cut behind your ear. They remove the brain tumor through this tear.
Awake Craniotomy
- An awake craniotomy is done while you’re awake. During the surgery, your surgeons ask you questions while covering your brain activity.
- As you react, they’ll indicate what parts of the brain are involved in speech, movement, and vision. This helps them avoid these regions while performing the surgery.
Frontotemporal Craniotomy
- In the cranium, the pterion is where the frontal, temporal, sphenoid, and parietal bones meet. It’s set up on the side of your cranium near your temple.
- A Frontotemporal craniotomy, or frontotemporal craniotomy, involves removing a piece of the pterion. Your surgeon makes an incision behind your hairline, letting them access multitudinous parts of the brain.
Posterior Fossa Craniotomy
- The posterior fossa is the lower part of the cranium. It’s near the brainstem and cerebellum, which controls balance and collaboration.
- still, it can place pressure on the cerebellum, brainstem, and spinal cord, If there’s a tumor in the posterior fossa
- A posterior fossa craniotomy can remove the tumor and palliate this pressure. This is done through an incision at the base of your cranium.
Reasons For The Surgery
- A craniotomy may exist for a variety of reasons, involving, but not limited to, the following:
- Diagnosing, putting off, or treating brain tumors
- Cutting or repairing an aneurysm
- Removing blood or blood clots from a blatting blood vessel
- Removing an arteriovenous contortion(AVM) or addressing an arteriovenous fistula (AVF)
- bleeding a brain abscess, which is an infected pus-filled pocket
- Repairing skull fractures
- Repairing an incision in the membrane lining the brain
- Relieving stress within the brain (intracranial pressure) by removing damaged or swollen areas of the brain that may exist caused by traumatic injury or stroke
- Treating epilepsy
- Implanting stimulator devices to treat movement diseases similar to Parkinson’s disease or dystonia (a type of movement complaint)
- There may be different reasons for your doctor to recommend a craniotomy.
Risks Of The Surgery
- As with any surgical procedure, complications may occur. Brain surgery risk is tied to the specific position in the brain that the operation will affect. For example, if the region of the brain that controls speech is operated on, also speech may be affected. Some moreover general complications involve, but are not limited to, the following:
- Infection
- Bleeding
- Blood clots
- Pneumonia (infection of the lungs)
- Unstable blood pressure
- Seizures
- Muscle weakness
- Brain swelling
- Leakage of cerebrospinal fluid (the fluid that surrounds and fenders the brain)
- Risks associated with the use of overall anesthesia
- The following difficulties are rare and generally relate to specific locations within the brain, so they may or may not exist as valid risks for certain individuals:
- Memory problems
- Speech difficulty
- Paralysis
- Abnormal balance or coordination
- Coma
- There may exist other risks depending on your specific medical condition. Be sure to argue any concerns with your doctor previous to the Surgery.
Before The Surgery
- Your doctor will explain the operation to you and you can ask questions.
- You will be asked to sign a permission form that gives the authorization to do the surgery. Read the form strictly and ask questions if something is not clear.
- In addition to a perfect medical history, your doctor will do a physical test to insure you are in good health before you suffer the surgery. You may also need blood tests and different diagnostic tests.
- You will take a preoperative neurological test that will be used to compare with postoperative examinations.
- You will be asked to diet before the operation, naturally after midnight.
- If you are pregnant or suppose you may be, describe your healthcare provider.
- describe to your doctor if you are sensitive to or are allergic to any drugs, latex, tape, and anesthetic agents (original or general).
- describe your doctor of all drugs(specified and over-the-counter) and herbal supplements that you are taking.
- describe your doctor if you have a history of bleeding diseases or if you are taking any anticoagulant (blood-thinning) drugs, aspirin, or other drugs that affect blood clotting. It may be necessary for you to stop these drugs before the operation.
- If you smoke, you should stop smoking as soon as possible before the operation to help your chances for a successful recovery from surgery and to help your overall health status.
- You may be asked to wash your hair with antiseptic shampoo the night before the surgery.
- You may receive a painkiller before the operation to help you relax.
- The areas around the surgical spot will be shaved.
- Grounded on your medical condition, your doctor may request other special medication.
During The Surgery
- A craniotomy normally requires a hospital stay of 3 to 7 days. You may also come to a recovery unit for several days after your hospital stay. operations may vary depending on your health and your doctor’s practices.
- Generally, a craniotomy follows this process:
- You will be asked to remove any clothing, jewelry, or other things that may interfere with the procedure.
- You will be given a dress to put on.
- An intravenous (IV) line will be fitted into your arm or hand.
- A urinary catheter will be fitted to drain your urine.
- You will be positioned on the operating table in a manner that provides good access to the side of the brain to be operated on.
- The anesthesiologist will continuously cover your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
- Your head will be shaved and the skin over the surgical point will be cleansed with an antiseptic solution.
- There are many types of incisions that may be used, depending on the affected area of the brain. An incision may exist from behind the hairline in front of your ear and the nape of your neck, or in another position depending on the position of the problem. If an endoscope is used, the incisions may be fewer.
- Your head will be held in location by a device which will be removed at the end of the surgery.
- The scalp will exist pulled up and clipped to control bleeding while providing access to the brain.
- A medical drill may use to make burr holes in the cranium. A special saw may exist used to carefully cut the bone.
- The bone delirium will be removed and saved.
- The dura mater (the thick external covering of the brain directly underneath the bone) will be separated from the bone and carefully cut open to expose the brain.
- Excess fluid will be permitted to flow out of the brain if needed. Microsurgical instruments, similar to a surgical microscope magnify the area being treated, may be used. This can enable the surgeon a better view of the brain structures and the difference between abnormal tissue and healthy tissue. Tissue samples may be transferred to the lab for testing.
- A device, similar to a drain or a special type of monitor, may be placed in the brain tissue to measure the pressure inside the cranium, or intracranial pressure (ICP). ICP is the pressure created by the brain tissue, cerebral spinal fluid (CSF), and blood supply inside the closed cranium.
- Once the surgery is completed, the surgeon will sew the layers of tissue together.
- The bone flap will exist reattached using plates, sutures, or wires.
- Still, the flap may not be replaced, If a tumor or an infection is constituted in the bone, Also, if relaxation(to reduce pressure in the brain) is needed, the bone flap may not be replaced.
- The skin incision will be closed with sewing and surgical staples.
- An impotent bandage or dressing will exist applied over the incision.
After The Surgery
- In The Hospital
- At Home
In The Hospital
- Immediately after the operation, you will be taken to a recovery room for observation before being taken to the ICU (intensive care unit) to be nearly monitored. You may be taken straight to the ICU (intensive care unit) from the operating place.
- In the ICU, you may be given drugs to decrease brain swelling.
- Your recovery process will differ depending on the type of operation done and the type of anesthesia given. Once your blood pressure, pulsation, and breathing are stable and you are careful, you may be taken to the ICU or your hospital room.
- After staying in the ICU, you will transfer to a room in a neurosurgical nursing unit in the hospital. You will stay in the hospital for several further days.
- You may take oxygen for a period of short time after surgery. Normally, the oxygen will exist discontinued before you go home.
- You will be taught deep-breathing practices to help re-expand the lungs and help against pneumonia.
- Regular neurological checks will be done by the nursing and medical staff to test your brain function and to make sure your body complexes are performing correctly after your surgery. You will be asked to follow a variety of introductory commands, similar to moving your arms and legs, to assess your brain function. The strength of your legs and arms will be similarly tested.
- The head of your bed may be elevated to help to swell your face and head. Some swelling is normal.
- You will be encouraged to move around as permitted while in bed and to get out of bed and walk around, with assistance help at first, as your strength improves. A physical therapist (PT) may be asked to estimate your strength, balance, and mobility, and give you suggestions for exercises to do both in the hospital and at home.
- You will probably have sequential compression devices (SCDs) fixed on your legs while you are in bed to help with blood clot formation. SCDs (sequential compression devices) have an air compressor that slowly pumps air into and out of fitted sleeves that are fixed on the legs. They help blood clots from forming by passively compressing the leg veins to keep the blood moving.
- Depending on your status, you may be given liquids to drink some hours after surgery. Your diet may be gradationally changed to include further solid foods as you can handle them.
- You may have a catheter in your bladder to drain your urine for a day or therefore until you are suitable to get out of bed and move around. Be sure to describe any painful urination or other urinary symptoms that do after the catheter is removed, as these may be signs of an infection that can exist treated.
- Depending on your situation, you may be transferred to a rehabilitation facility for a period of time to recapture your strength.
- Before you are discharged from the hospital, conformations will be made for a follow-up visit with your doctor. Your doctor will suggest home care.
At Home
- Once you are home, it’s important to observe the incision is clean and dry. Your doctor will give you special bathing instructions. still, they will be removed during a follow-up office visit. If stitches or surgical masses are used. still, keep them dry and they will fall off within many days. If sticky strips are used
- You may take to wear a loose turban or cap over the incision. You should not wear a wig until the incision is fully healed (about 3 to 4 weeks after surgery).
- The incision and head may pain, specifically with deep breathing, coughing, and exertion. Take a pain reliever for soreness as committed by your doctor. Aspirin or other blood-thinning drugs may increase the chance of bleeding. Be confident to take only recommended drugs and ask if you are doubtful.
- Continue the breathing training used in the hospital to prevent lung infection. You will be advised to avoid exposure to upper respiratory infections (colds and flu) and annoyances, similar to tobacco smoke, fumes, and environmental pollution.
- You should gradationally increase your physical exercise as you can handle them. It may take several weeks to return to your previous position of energy and strength.
- You may be instructed to avoid lifting heavy particulars for several weeks to prevent strain on your surgical incision.
- Don’t drive until your doctor gives you permission.
- Call your doctor to describe any of the following:
- Fever or chills
- Redness, swelling, drainage, bleeding, or other drainages from the incision point or face
- Increased pain around the incision point
- Vision changes
- Confusion or excessive sleepiness
- Your arms or legs Weakness
- Trouble with speech
- Chest pain, anxiety, Trouble breathing, or change in the internal status
- Green, yellow, or blood-tinged spit(numbness)
- Seizure activity
- Following a craniotomy, your doctor may present you with other instructions, depending on your particular status.
Post-Operative Physiotherapy
- The position of physiotherapy intervention and rehabilitation post craniotomy varies extensively and is impressed by a number of factors including the actual surgery, the condition which is being treated, the patient’s pre-morbid condition, and also the general effects of being in the hospital.
- Normally, the goals of physiotherapy post craniotomy are to maintain or increase range of motion and muscle strength, reduce and prevent spasticity and contractures, functional transfer or gait training, and to better balance and coordination.
- In neurological Intensive Care Units, physiotherapy intervention is both safe and beneficial. The benefits include the decreased length of hospital stay, decreased time on ventilation, improved muscle strength, and increased independence in activities of daily living.
- It has been found patients undergoing intracranial pressure monitoring received less frequent and intensive physiotherapy, despite the evidence standard physiotherapy practice is safe for these patients. At present, there are no set protocols for physiotherapy post-craniotomy, and instead, care is directed by the physiotherapists’ assessment findings.
- There can be long-term impairments to a patient’s function and quality of life, for which they might require ongoing physiotherapy intervention.
- Rehabilitation programs should be tailored to the individual patient’s abilities, prognosis, and goals.
Recovery
- Recovery depends on the type of surgery. Then’s what it usually looks like:
Immediately After Surgery
- You’ll exist taken to the recovery unit or intensive care unit when the Surgery is complete. Nurses will watch your vitals as you wake up.
- You’ll exist taken to your hospital room once your vitals are stable. You can anticipate staying at the hospital for around 1 week.
- During your stay, your healthcare providers will probably:
- elevate your head to manage to swell
- give you oxygen for several days
- teach you deep-breathing exercises to prevent pneumonia
- place contraction devices on your legs to prevent blood clots
- The urinary catheter will stay in your bladder for a few days.
- Your healthcare team will constantly do neurological checkups to insure your brain and body are performing properly.
- Before you go home, your surgeon will give home care instructions.
At Home
- After a craniotomy, follow your doctor’s arrangements for bathing and incision care. Take your prescription medication as directed.
- You can anticipate being out of work for at least 6 to 8 weeks.
- During this Surgery, you might have issues with:
- walking
- talking
- strength
- balance
- To recapture these functions, you may need physical therapy, occupational therapy, or speech therapy. You’ll also take to get lots of rest.
- Attend your follow-up so your doctor can see how you’re recovering. They’ll allow you know when you can resume certain conditioning.
What Are The Results?
- The results of your craniotomy depend on the underpinning condition being treated.
Life After Craniotomy Surgery
- After you’ve completely recovered, it’s still important to take care of yourself. This will help manage future difficulties and improve your long-term outlook.
- Continue seeing your doctor for follow-up appointments. It’s also wise to:
- exercise regularly
- eat a healthy diet
- limit or avoid alcohol
- quit smoking
- get enough sleep
FAQ
Exercise. Avoid risky activities, similar to climbing a ladder, for 3 months after surgery. Avoid forceful activities, similar to bike riding, jogging, weight lifting, or aerobic exercise, for 3 months or until your doctor says it is fine.
Post-Operative Physiotherapy aims to help people to restore optimal mobility and general functions in the body. It also helps in. 1) Improving posture Building muscle strength and balance of the body. 2) Reducing pain with various primer therapy that is crucial for strengthening weakened and disused muscles.
Patients are positioned 30° to 60° head-up. This technique has lately been associated with hypotensive episodes and consequent severe neurologic dysfunction, involving brain stem infarction from cerebral hypoperfusion and visual loss.
Positive exercise like spending time with family and friends, planning a pleasure event, light exercise, gardening, and attending therapy are good options. A healthy diet can also fuel the brain and help in recovery. The brain requires energy to function, indeed more so when recovering from brain surgery.
Permanent brain damage. pooling of infected fluid in the brain inflammation bleeding between your brain and scalp.
The usual length of stay for patients undergoing craniotomy for a brain tumor is 4 to 5 hospital days. Patients who have postoperative difficulties may be required to stay longer.
You will probably feel very tired for a few weeks after surgery. You may have headaches or problems concentrating. It can take 5 to 8 weeks to recover from surgery. Your incisions may be sore for about 4 to 5 days after surgery.