Deep Brain Stimulation (DBS)
Table of Contents
Overview-
- Deep brain stimulation (DBS) is a surgery to place a device that dispatches electrical signals to brain areas accountable for body movement.
- Electrodes are set deep in the brain and are connected to a stimulator device.
- Alike to a heart pacemaker, a neurostimulator uses electric pulses to manage brain activity.
- DBS may help decrease the symptoms of tremors, slowness, stiffness, and walking problems caused by Parkinson’s disease, dystonia, or essential tremor.
- Successful DBS allows individuals to potentially decrease their medications and improve their quality of life.
What is deep brain stimulation?
- In this deep brain stimulation, electrodes are situated in a specific area of the brain to turn on the symptoms being treated.
- The electrodes are situated on both the left and right sides of the brain through small holes constructed at the top of the skull.
- The electrodes are attached by long wires that travel under the skin and down the neck to a battery-powered stimulator under the skin of the chest.
- When turned on, the stimulator sends electrical pulses to manage the faulty nerve signals causing tremors, rigidity, and other symptoms.
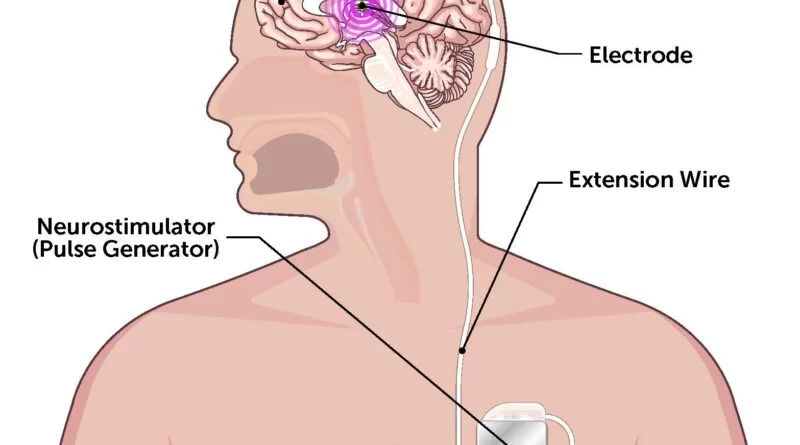
The parts of the DBS system-
- The electrode, or lead, is a thin, insulated wire placed through a small opening in the skull and inserted into a specific brain area.
- The extension wire is also insulated and passed under the skin of the head, neck, and shoulder, attaching the electrode to the internal pulse generator (IPG).
- The IPG is the third piece of the system and is generally implanted under the skin in the upper chest.
Description of Deep brain stimulation system-
A DBS system includes three parts that are implanted inside the body:
Neurostimulator –
- A programmable battery-powered pacemaker device that generates electric pulses.
- It is situated under the skin of the chest below the collarbone or in the abdomen.
Lead –
- A coated wire with a number of electrodes at the tip passes the electric pulses to the brain tissue.
- It is situated inside the brain and connects to an extension wire through a small hole in the skull.
Extension-
- An insulated wire joints lead to the neurostimulator. It is situated under the skin and runs from the scalp, behind the ear, down the neck, and to the chest.
Electrodes may be placed in the following brain areas ;
The subthalamic nucleus (STN) –
- Effectual for tremor, slowness, rigidity, dystonia, and dyskinesia.
- Most frequently used to treat Parkinson’s disease.
Thalamus (VIM) –
- Effectual for tremor.
- It is mostly used to treat essential tremors.
Globus pallidus (GPi) –
- Effectual for tremor, slowness, rigidity, dystonia, and dyskinesia.
- It is generally used to treat dystonia and Parkinson’s disease.
Uses of the DBS system-
Deep brain stimulation is generally used to treat a number of conditions, like;
- Parkinson’s disease
- Essential tremor
- Dystonia
- Epilepsy
- Obsessive-compulsive disorder
Deep brain stimulation is also being studied as an important treatment for:
- Tourette syndrome
- Huntington’s disease and chorea
- Chronic pain
- Cluster headache
Symptoms-
Each disease type has a diversity of symptoms that patients may feel. Frequent ones are:
Dystonia-
- Involuntary muscle contractions take place during specific actions (For example; writing)
- Muscle contractions get worse with stress, fatigue, or anxiety.
Epilepsy-
- Temporary confusion
- A staring spell
- Loss of consciousness
- Uncontrollable jerking movements of the arms or legs
- Emotional responses like; fear, and anxiety.
Essential Tremor-
- Tremors take place during daily activities such as; writing or drinking.
Obsessive-compulsive Disorder-
- Obsessive-compulsive Disorder-
- Fear of germs or contamination
- Aggressive thoughts toward other people or one’s self
- Having some things in symmetrical or in perfect order
- Excessive cleaning or handwashing
- Compulsive counting
- Checking things repeatedly (For example, the oven is off, the door is locked, etc.).
Parkinson’s Disease-
- Tremor
- Bradykinesia – slowing down of movement
- Stiffness
- Abnormal walking.
Testing & Diagnosis-
- There is a multifaceted team of executives including a neurologist, neurosurgeon, neuropsychologist, and psychiatrist that may care for patients.
- Frequently patients with Parkinson’s disease or tremors may undergo testing of motor symptoms on and off medications to know the severity of the disease.
- Epilepsy testing can include electroencephalography, which involves more advanced testing.
- Few patients may undergo neuropsychological evaluation during evaluation.
- Obsessive-compulsive disorder patients must complete Yale-Brown Obsessive Compulsive Scale (YBOC) testing.
Prior to surgery, patients undergo the following:
- Blood and urine tests.
- This helps identify toxins and abnormalities.
- MRI and CT scans.
- Imaging may help doctors target the right brain area for symptom relief.
- Medical Clearance.
Criteria for DBS system-
- Symptoms are substantially decreasing quality of life.
- Symptoms are not in control despite receiving a suitable dose of medications.
- Side effects stemming from current medications cannot be authorized.
Treatment-
Non-Surgical Treatments-
Before being chosen for surgical interventions like DBS, doctors may allow any of the following treatments.
- Medications.
- Physical Therapy.
Surgery;
How to work the DBS system-
- The DBS system consists of four parts:
- One or more, insulated wires called leads, or electrodes, are situated in the brain.
- Anchors to affix the leads to the skull The neurostimulator placed out the electric current.
- The simulator is such as a heart pacemaker.
- It is usually situated under the skin below the collarbone but may be placed elsewhere in the body.
- In some people, another thin, insulated wire called an extension is added on to connect the lead to the neurostimulator.
- Surgery is done to locate each part of the neurostimulator system. In young individuals, the whole system may be situated in 1 or 2 stages (two separate surgeries).
Stage 1-
This is generally done under local anesthesia, meaning the person is awake but pain-free. (In children, general
anesthesia is given.)
- A bit of hair on the head is likely shaved.
- The head is placed in a particular frame using small screws to hold on it still during the procedure.
- Numbing medicine is petitioned where the screws contact the scalp.
- Sometimes, the procedure is done in the MRI machine and a frame is on top of the head rather than around the head.
- Numbing medicine is put into the scalp at the site where the surgeon will open the skin, then drill a tiny opening in the skull and places the lead into a specific area of the brain.
- If both sides of the brain are being treated, the surgeon makes an opening on each side of the skull, and two leads are thrust.
- Electrical impulses may need to be sent through the lead to be sure that it is connected to the area of the brain responsible for the symptoms.
- A person can ask questions, read cards, or describe images.
- The person may also be asked to move their legs or arms.
- These are to be sure that the electrodes are in the right positions and that the expected effect is achieved.
Stage 2-
This is done under general anesthesia, meaning individuals are asleep and pain-free. The timing of this stage of surgery turns on where in the brain the stimulator will be placed.
- The surgeon constructs a small opening (incision), generally just below the collarbone, and implants the neurostimulator.
- (Sometimes it is situated under the skin in the lower chest or belly area.)
- The extension wire is tunneled under the skin of the head, neck, and shoulder and connected to the neurostimulator.
- The incision is closed.
- The device and wires are under the skin and may appear as a slight bump.
- Once connected, electric pulses proceed from the neurostimulator, along the extension wire, to the lead, and into the brain.
- These small pulses interfere with and block the electrical signals that cause symptoms of certain diseases.
Advantages of surgery-
- Advantages of surgery-
- May be performed on one or both sides of the brain, depending on symptoms.
- The effects are reversible and may be designated individually for each patient’s clinical status.
- Stimulation settings may be altered to diminish potential side effects and improve effectiveness over time.
- The device may come up with continuous symptom control 24 hours a day.
- Patients who have undergone DBS may participate in other treatments, like stem cell or gene therapy, when they become available.
Risk factors of surgery-
- Deep brain stimulation includes creating small holes in the skull to implant the electrodes into the brain tissue as well as performing surgery to implant the device that accommodates the batteries under the skin in the chest.
Complications of surgery-
- Misplacement of leads
- Bleeding in the brain
- Stroke
- Infection
- Breathing problems
- Nausea
- Heart problems
- Seizure
Side effects after surgery-
- Possible side effects after surgery
- Seizure
- Infection
- Headache
- Confusion
- Difficulty concentrating
- Stroke
- Hardware complications, like an eroded lead wire
- Nonpermanent pain and swelling at the implantation site
- A few weeks after the surgery, the device will be turned on and the process of finding the best settings for the person begins.
- Some settings can cause side effects, but these often improve with further adjustments of patients’ devices.
- Because there have been unusual reports that DBS therapy affects the movements needed for swimming, the Food and Drug Administration put forward consulting with the doctor and taking water safety precautions before swimming.
Possible side effects of stimulation-
- Numbness or tingling sensations
- Muscle tightness of the face or arm
- Speech problems
- Balance problems
- Lightheadedness
- Vision problems, like double vision
- Unwanted mood changes, like anger and depression
FAQ-
Patient satisfaction, although, remained high (92.5% were happy with DBS, 95% would recommend DBS, and 75% felt it provided symptom control).
The most individual feels little if any sensation at all during normal use. For the few that do, it is mentioned as a little tingling sensation down an arm or leg or mild facial pulling which subsides. This is more common in people using DBS for essential tremors as the device may be turned off at bedtime.
Difficulty concentrating. Stroke. Hardware complications, like an eroded lead wire. Temporary pain and swelling at the implantation site.
Deep brain stimulation benefits appear to last for not very many years but not enough research has been accessible to show that these outcomes are still present more than 15 years after surgery.”
Yes, a patient can travel with their DBS System. Metal detectors, X-ray machines, security scanners, and other security devices will not harm the implant but they can cause unintentional stimulation. The implant may also activate metal detector alarms.




One Comment