Epilepsy
Table of Contents
What is epilepsy?

- Epilepsy is a condition that causes unprovoked, recurrent seizures.
- A seizure is an unexpected rush of abnormal electrical activity in your brain.
- Doctors diagnose epilepsy when you have 2 or more seizures with no other identifiable cause.
- Epilepsy affects fifty million trusted Source people around the world, according to the World Health Organization (WHO), and nearly 3.5 million trusted Source people in the United States, per the Centers for Disease Control and Prevention (CDC).
- Anyone can develop epilepsy, yet it most commonly trusted Source of onsets in young children & older adults.
- According to research published in 2021, men develop epilepsy more frequently than women, possibly because of higher exposure to risk factors like alcohol use & head trauma.
What are the types of epilepsy?
- Generalized seizures
- Focal seizures.
- Generalized seizures affect your whole brain.
- Focal, or partial seizures, can affect only one part of your brain.
- A mild seizure may be hard to recognize.
- It may only last a few seconds, and you may remain awake while it occurs.
- Stronger seizures can cause spasms & uncontrollable muscle twitches.
- They can last from a few seconds to several minutes & may cause confusion or loss of consciousness.
- Afterward, you may have no memory of a seizure occurring.
- There is currently no cure for epilepsy, yet it can be managed with medications and other strategies.
Focal seizures
- Focal seizures result from unusual electrical activity in one area of your brain.
Focal seizures can happen with or without loss of consciousness:
- Focal seizures with impaired awareness.
- These seizures include a change or loss of consciousness or awareness that feels like being in a dream.
- You may seem awake, yet you stare into space & do not respond normally to your environment or you perform repetitive movements.
- These may involve hand rubbing, mouth movements, repeating some words, or walking in circles.
- You may not remember the seizure or even know that it happened.
- Focal seizures without loss of consciousness.
- These seizures may alter emotions or change the way things look, smell, feel, taste or sound, yet you do not lose consciousness.
- You may instantly feel angry, joyful, or sad.
- Some people have nausea or uncommon feelings that are difficult to describe.
- These seizures may also result in difficulty speaking, involuntary jerking of a body part, such as an arm or a leg, & spontaneous sensory symptoms such as tingling, dizziness, and seeing flashing lights.
- Symptoms of focal seizures may be confused with other neurological disorders, like migraine, narcolepsy, or mental illness.
Generalized seizures
- Seizures that seem to involve all areas of the brain are called generalized seizures.
Different types of generalized seizures involve:
Absence seizures:
- Absence seizures, previously known as petit mal seizures, often happen in children and are characterized by staring into space or by subtle body movements, such as eye blinking or lip smacking. They commonly last for five to 10 seconds but may happen up to hundreds of times per day. These seizures may happen in clusters and cause a brief loss of awareness.
- Absence seizures include brief, instant lapses of consciousness.
- They are more usual in children than in adults.
- Someone having an absence seizure may look like he or she is staring blankly into space for some seconds.
- Then, there is a fast return to a normal level of alertness.
- This type of seizure commonly does not lead to physical injury.
- Absence seizures commonly can be controlled with anti-seizure medications.
- Certain children who have them also develop other seizures.
- Many children grow beyond the absence of seizures in their teens.
What are the symptoms of the seizure?
- An indication of a simple absence seizure is an empty stare, which may be mistaken for a lapse in attention that lasts about ten seconds, though it may last as long as twenty seconds, without any confusion, headache, or drowsiness afterward.
Signs and symptoms of absence seizures involve:
- Sudden stop in motion without falling,
- Lip smacking,
- Eyelid flutters,
- Chewing motions,
- Finger rubbing,
- Small movements of both hands.
- Later, there is no memory of the incident.
- Certain people have many episodes daily, which interfere with school or daily activities.
- A child may have absent seizures for a certain time before an adult notices the seizures because they are so brief.
- A decline in a child’s learning ability may be the first sign of this disorder.
- Teachers may comment about a child’s inability to pay attention or that a child is frequently daydreaming.
What are the causes of the seizures?
- Many children appear to have a genetic predisposition to the absence of seizures.
- In common, seizures are caused by abnormal electrical impulses from nerve cells (neurons) in the brain.
- The brain’s nerve cells commonly send electrical and chemical signals across the synapses that connect them.
- In people who have seizures, the brain’s common electrical activity is altered.
- During an absence seizure, these electrical signals repeat themselves over & over in a three-second pattern.
- People who have seizures may also have altered levels of the chemical messengers that assist the nerve cells to communicate with one another (neurotransmitters).
What are the risk factors for seizures?
Certain factors are common to children who have absent seizures, involving:
- Age: Absence seizures are more usual in children between the ages of 4 and 14.
- Sex: Absence seizures are more usual in girls.
- Family members who have seizures: Nearly half of the children with absence seizures have a close relative who has seizures.
What are the complications of seizures?
While most children outgrow absence seizures, certain:
- Must take anti-seizure medications throughout life to cure seizures,
- Eventually have full convulsions, like a generalized tonic-clonic seizure.
Other complications can involve:
- Learning difficulties,
- Behavior problems,
- Social isolation.
When to see a doctor
Contact your doctor:
- The first time you see a seizure,
- If this is a new type of seizure,
- If the seizures continue to happen despite taking anti-seizure medication.
Tonic seizures:
- Tonic seizures cause stiffening of your muscles. These seizures commonly affect muscles in your back, arms, and legs and may cause you to lose consciousness and fall to the ground.
What is a tonic seizure?
- Muscle “tone” is the muscle’s usual tension at rest.
- In a tonic seizure, the tone is greatly increased: the body, arms, or legs become instantly stiff or tense.
- A person may be aware or have only less change in awareness during a tonic seizure.
- They usually happen during sleep and commonly involve all or most of the brain, affecting both sides of the body.
- They are short, commonly less than 20 seconds.
- A person may fall down if standing when a tonic seizure starts.
Where does a tonic seizure begin in the brain?
When it starts in one part of the brain:
- Stiffening of a part of the body may begin in one area & stay local.
- These are called focal tonic seizures.
When it starts on both sides of the brain:
- The full body or both sides of the body may become stiff or tense from the beginning.
- These are called generalized tonic seizures.
Who is at risk for tonic seizures?
- Tonic seizures can occur in anyone.
- They are more typical in people who have Lennox-Gastaut syndrome or other syndromes with mixed seizure types.
How can I ask if someone is having one?
- Stiffening or other movements can be seen in other neurological problems, especially in children.
- A written description or video of what occurs during the seizure is very important.
- For example, tonic seizures start instantly with forceful movements.
- Events that start more slowly may be due to another condition.
What happens after a tonic seizure?
- When a tonic seizure ends, the person may or may not be sleepy or confused.
- Commonly, no first aid is needed unless a person is not fully aware during or after the seizure.
- Preventing harm is a key part of first aid for tonic seizures.
- Certain people may need to wear protective equipment like a helmet to prevent head injuries from falls.
If someone has tonic seizures, how often will they occur?
- It depends & varies between people.
- Some people may have just one seizure and others may have tonic seizures that happen often or in clusters of many a day.
How are tonic seizures diagnosed?
- Imaging tests like MRI (magnetic resonance imaging) scans to look for lesions or parts of the brain causing tonic & other types of generalized seizures.
- EEG (electroencephalogram) tests can assist tell the difference between tonic seizures & other symptoms.
How are tonic seizures treated?
- Seizure medicines are an important way of treating & preventing tonic seizures.
- If seizures are not controlled with medications, other options may be possible, like dietary therapies, devices, or even surgery.
- Knowing where a seizure starts and what part of the brain is involved assists you learn what options may be possible.
- If seizures are not controlled, seek out the assistance of an epilepsy specialist or visit an epilepsy center to explore treatment options.
What should I do if I believe my loved one or myself may have tonic seizures?
- If you think that you or your loved one may be having tonic seizures, ask your doctor as soon as possible.
- Getting the correct diagnosis early can assist lead to better treatment.
Atonic seizures:
- Atonic seizures, also known as drop seizures, cause a loss of muscle control, which may cause you to instantly collapse, fall down, or drop your head.

What are the atonic seizures?
- A seizure occurs when electrical activity in the brain surges suddenly.
- Atonic seizures are a type of seizure that causes instant loss of muscle strength.
- These seizures are also called akinetic seizures, drop attacks or drop seizures.
- The instant lack of muscle strength, or tone, can cause the person to fall to the ground.
- The person commonly remains conscious, and may not always fall down.
- Their head may drop, their eyelids may droop, & they may drop anything they were holding.
- These types of seizures frequently begin in childhood and may last into adulthood.
- Sometimes they are linked to other conditions, such as Lennox-Gastaut syndrome.
What are the symptoms of the seizures?
- Atonic seizures result in an instant loss of muscle strength while the seizure is occurring.
Other symptoms may involve:
- Going limp and falling to the ground
- Remaining conscious
- Experiencing a brief loss of consciousness
- Drooping eyelids
- Head nods
- Jerking.
- Because these seizures often result in a fall, the patient may require first aid once the seizure is over.
- Certain people who have these seizures often may choose to wear protective gear, like a helmet.
What are the causes and risk factors of seizures?
- The cause of atonic seizures is frequently unknown.
- Certain patients may be more likely to have seizures because of changes in their genes.
- Atonic seizures most often affect children yet can occur in patients of any age.
- Rapid breathing (hyperventilation) & flickering lights can trigger seizures.
What is the diagnosis of the seizures?
- The most practical test in diagnosing seizures is an electroencephalogram (EEG).
- This records the electrical activity in the brain.
- EEG can show uncommon electrical activity patterns.
- Various types of seizures can be identified with these patterns.
- Magnetic resonance imaging (MRI) & computed tomography (CT) scans may be used to study the condition.
- These images can also show where the seizure is occurring in the brain.
- The scans can also rule out other possible causes like as a stroke.
What is the treatment for seizures?
- Patients may need to wear helmets to cure head injuries during seizures if falling is common.
- Medication is the most usual treatment.
- Anti-seizure (or anti-epileptic) medications can very assist.
- It may take a few tries to find the right drug & the right dose.
- The doctor will monitor for side effects to notice the best option.
These medications involve:
- Ethosuximide (Zarontin) is most frequently used as the first drug treatment.
- Valproic acid (Depakene) is another option.
- It is not recommended for women who are pregnant or want to become pregnant as it can grow the risk of birth defects.
- Lamotrigine (Lamictal) has fewer side effects than the other two medications yet may also be less helpful.
- Clobazam (Onfi).
- Some types of seizures may be controlled with a ketogenic diet.
- This is a high-fat, low-carbohydrate diet used most frequently for children who have not responded to medications.
- A vagus nerve stimulator is sometimes implanted & used along with anti-epileptic medication to reduce seizures.
- The vagus nerve stimulator is a device placed under the skin of the chest that sends electrical energy through the vagus nerve in the neck to the brain.
Clonic seizures:
- Clonic seizures are associated with repeated, rhythmic, jerking muscle movements. These seizures commonly affect the neck, face, and arms on both sides of the body.
What is a clonic seizure?
- “Clonus” (KLOH-us) means fast stiffening and relaxing of a muscle that occurs repeatedly.
- In another word, it is repeated jerking.
- The movements can not be stopped by restraining or repositioning the arms or legs.
- Clonic (KLON-ik) seizures are rare & most commonly happen in babies.
- Most often, clonic movements are shown as part of a tonic-clonic seizure.
- Jerking movements alone, as with a clonic seizure, may last some seconds to a minute.
- Jerking or clonic movements that follow stiffening of muscles, as in a tonic-clonic seizure, can last seconds to one or two minutes.
- A clonic seizure may occasionally be hard to distinguish from a myoclonic seizure.
- The jerking is more consistent & sustained during a clonic seizure.
Where does a clonic seizure start in the brain?
When it starts in one part of the brain:
- Clonic seizures can start in the motor part on one side of the brain.
- These are called focal clonic seizures.
- The jerking movements would affect just one side or area of the body or face.
When it starts on both parts of the brain:
- Clonic seizures can also affect both parts of the brain at once.
- These would be called generalized clonic seizures.
- The jerking movements would affect both parts of the body or the whole body at once.
Who is at risk for clonic seizures?
- Clonic seizures can affect people of all ages, involving newborns.
- In infants, the clonic seizures are very brief and do not happen very often.
- They may also go away on their own for a less period of time.
- Clonic seizures that do not go away on their own will need long-term treatment.
What is it like to have a clonic seizure?
- Clonic seizures consist of repeated jerking movements of the arms & legs, occasionally on both sides of the body.
- If the clonic seizure has a focal onset (starts in one part of the brain), the person may be conscious during it.
- If the clonic seizure has a generalized onset (affects the whole brain), commonly the person is not aware during it.
- If a person is standing when a clonic seizure happens, they may fall.
- Sometimes a focal clonic seizure affects both the motor & sensory parts of the brain.
- It may also involve tingling or numbness of the body part with the jerking.
What happens after a clonic seizure?
- After a clonic seizure, the person may simply continue what they are doing, especially if they were aware when it occurred.
- If a person was not fully aware, they may need to rest for a few minutes before returning to common activity.
- The most important first aid step is to cure the person from injury when the jerking happens or if they fall.
- Do not try to prevent the person’s movements.
- If a clonic seizure goes into a tonic-clonic one, the person will most likely be tired & confused after the seizure.
- Let them rest as needed & follow care & comfort first aid.
If someone has clonic seizures, how often will they occur?
- The frequency of seizures depends a lot on the cause & the person.
- Certain people may have rare seizures, & others may have them more frequently.
How can I ask if someone is having a clonic seizure?
- Clonic seizures consist of rhythmic jerking movements of the arms and legs, occasionally on both sides of the body, that can be seen by the person observing.
- Occasionally “jitteriness” in a young infant can be mistaken for a clonic seizure, especially if it is serious (during crying, for instance).
- Changing the position of the baby’s arms or legs should decrease or stop jitteriness.
- A jittery infant also will be more aware than an infant who is having a clonic seizure.
- Children with other neurological problems can have repeated jerking that could be mistaken for clonic seizures.
- EEG (electroencephalogram) testing may be needed to see what occurs in the brain when the symptoms occur.
How are clonic seizures diagnosed?
- The best description of the symptoms is the first step.
- Written reports of what occurs from the person having the seizure & from observers can be very helpful.
- Bring the video recordings of events to the doctor’s visit if you have them.
- An electroencephalogram is done to show the electrical activity of the brain.
- Video electroencephalogram telemetry that can record the electrical activity and what it looks like during an event is helpful if seizures don’t respond to treatment.
- This test may also be done to sort out the clonic seizures from other causes.
How are clonic seizures treated?
- Some seizure medicines help prevent clonic seizures.
- Knowing where seizures begin – in one part (focal onset) or both sides (generalized onset) of the brain – will help decide which medicine may be best to use.
What should I do if I think my loved ones or myself may have clonic seizures?
- If you think you or your loved one may be having clonic seizures, ask your doctor as soon as possible.
- Getting these diagnosed early can assist lead to better treatment.
Myoclonic seizures:
- Myoclonic seizures commonly appear as sudden brief jerks or twitches of your arms and legs. There is frequently no loss of consciousness.
What is a myoclonic seizure?
- Myoclonic (MY-o-KLON-ik) seizures are short, shock-like jerks of a muscle or a group of muscles.
- “Myo” means muscle and “clonus” (KLOH-us) means quickly alternating contraction and relaxation—jerking or twitching—of a muscle.
- commonly they do not last more than a second or two.
- There can be just one, yet sometimes many will occur within a short time.
- Even people without epilepsy can experience myoclonus in hiccups or in an unexpected jerk that may wake you up as you are just falling asleep.
- These things are usual.
- In epilepsy, myoclonic seizures commonly cause abnormal movements on both sides of the body at the same time.
They happen in a variety of epilepsy syndromes that have different characteristics:
Juvenile myoclonic epilepsy: The seizures usually include the neck, shoulders, and upper arms. In many patients, the seizures most often happen soon after waking up. They commonly begin around puberty or sometimes in early adulthood in people with a normal range of intelligence. In most cases, these seizures can be well controlled with medication yet they must be continued throughout life.
Lennox-Gastaut syndrome: This is an uncommon syndrome that usually involves other types of seizures as well. It begins in early childhood. Myoclonic seizures usually include the neck, shoulders, upper arms, & often the face. They may be quite strong & are difficult to control.
Progressive myoclonic epilepsy: The rare syndromes in this category feature a combination of myoclonic seizures & tonic-clonic seizures. Treatment is commonly not successful for very long, as the patient deteriorates over time.
Who is at risk for myoclonic seizures?
- The epileptic syndromes that most commonly involve myoclonic seizures usually begin in childhood, but the seizures can occur at any age.
- Other characteristics depend on the particular syndrome.
What happens after a myoclonic seizure?
- When a myoclonic seizure ends, the person commonly continues doing whatever they were doing before and during the seizure.
- They are awake & able to think clearly.
- No first aid is required because of this seizure.
If someone is having a myoclonic seizure, how often will it happen?
- There can be just one, yet sometimes many will occur within a short time.
How can I ask if someone is having a myoclonic seizure?
- These seizures can be easily overlooked because they are so brief & appear as extra normal movements.
- These seizures can be mistaken for tics, tremors, or clumsiness.
How are myoclonic seizures diagnosed?
- The seizures themselves are easy to identify.
- The syndromes commonly can be diagnosed on the basis of medical history and often an EEG test.
How are myoclonic seizures treated?
- There are several medicines that can assist prevent myoclonic seizures.
- Myoclonic seizures frequently respond well to the appropriate medicine.
What should I do if I believe my child, loved one, or myself may have myoclonic seizures?
- If you think that you or your loved one are having myoclonic seizures, talk to your child’s doctor or your own & share your concerns right away.
- Because myoclonic seizures are often associated with some syndromes, seeing a doctor quickly to make a diagnosis & begin treatment is essential.
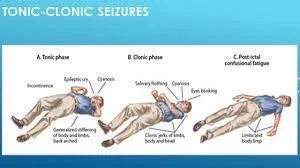
Tonic-clonic seizures:
- Tonic-clonic seizures, before known as grand mal seizures, are the most dramatic type of epileptic seizure and can cause an abrupt loss of consciousness, body stiffening & shaking, & sometimes loss of bladder control or biting your tongue. They may last for some minutes.
- Tonic & clonic seizures affect the muscles.
- Tonic seizures cause a stiffening of muscles periods of clonic seizures are characterized by jerking or twitching.
- Tonic & clonic seizures can start on one part of the brain (partial or focal seizures), or on both sides of the brain simultaneously (generalized).
- Tonic and clonic seizure activity can occur in the same seizure.
- A tonic-clonic seizure is a modern period for a grand mal seizure.
If a character near you has a seizure:
- Do not put anything in the person’s mouth.
- Do not restrain them.
- Make sure the area around the person is clear of objects that could harm them.
- Treatment for tonic & clonic seizures may include medication, nerve stimulation, dietary therapy, surgery, or a combination of these approaches.
- Tonic & Clonic Seizures: Partial or Generalized
- A seizure that originates in both halves (hemispheres) of the brain simultaneously, causing stiffness or twitching over the body, is known as a generalized tonic or clonic seizure.
- A tonic or clonic seizure can also begin in one area of the brain (called a partial or focal seizure), affecting only one portion of the body such as an arm or a leg.
Tonic or clonic seizures can start as partial & become generalized.
Tonic Seizures
- A tonic seizure causes an instant stiffness or tension in the muscles of the arms, legs, or trunk.
- The stiffness lasts about twenty seconds and is most likely to happen during sleep.
- Tonic seizures that happen while the person is standing may cause them to fall.
- After the seizure, the person may feel tired or confused.
- People with Lennox-Gastaut syndrome or other types of epilepsy with mixed seizures are most likely to have tonic seizures, yet they can happen to anyone.
Clonic Seizures
- Clonic seizures are characterized by repeated jerking movements of the arms and legs on one or both sides of the body, occasionally with numbness or tingling.
- If it is a focal (partial) seizure, the person may be aware of what’s occurring.
- During the generalized seizure, the person may be unconscious.
- Clonic seizures can happen in people of all ages, including newborns and infants.
What to Do When Someone Has a Seizure?
- First aid for a person having a tonic or clonic seizure includes protecting the person from injury, such as moving furniture or other items out of the way.
- It is important not to attempt to restrain the person or put anything in their mouth — “swallowing the tongue” is impossible.
- Later, the person is likely to be tired, embarrassed, or confused.
- Offer supportive care & reassurance.
- 1st-time seizures should be evaluated by a doctor.
Diagnosis & Treatment of Tonic & Clonic Seizures
- Creating a written report by describing the details of the seizure can be assisted when the patient or parent sees the doctor.
- A video of the seizure taking place, if available, can assist the doctor make a diagnosis.
- To diagnose tonic & clonic seizures, the physician is likely to use imaging tests like magnetic resonance imaging (MRI) to look for scarred areas in the brain, as well as electroencephalography (EEG) to assist differentiate seizures from other problems.
- Tonic & clonic seizures, like other seizures and seizure disorders, need an individualized approach.
- The doctor may commend treatment with anti-seizure medication, nerve stimulation, dietary therapy, or surgery.
What are the symptoms of epilepsy?

- Seizures are an important symptom of epilepsy.
- Symptoms dissimilar from person to person & according to the type of seizure.
Focal (partial) seizures
- A focal aware seizure (previously called simple partial seizure) does not include loss of consciousness.
Symptoms include:
- alterations to the sense of taste, smell, sight, hearing, or touch,
- dizziness,
- tingling and twitching of limbs,
- Focal unaware seizures (previously called complex partial seizures) include loss of awareness or consciousness.
Other symptoms involve:
- staring blankly,
- unresponsiveness,
- performing repetitive movements,
- Generalized seizures,
- Generalized seizures involve the whole brain.
Subtypes involve:
- Absence seizures: Absence seizures used to be called “petit mal seizures.” They tend to cause a short loss of awareness, and a blank stare, & may cause repetitive movements like lip smacking or blinking.
- Tonic seizures: Tonic seizures cause unexpected stiffness in the muscles in your legs, arms, or trunk.
- Atonic seizures: Atonic seizures conduct in loss of muscle control. They are also called “drop seizures” because an unexpected loss of muscle strength can make you fall suddenly.
- Clonic seizures: Clonic seizures are characterized by repeated, jerky muscle movements of the face, neck, & arms.
- Myoclonic seizures: Myoclonic seizures cause spontaneous fast twitching of the arms & legs. Sometimes these seizures cluster together.
- Tonic-clonic seizures: Tonic-clonic seizures are used to be called “grand mal seizures.”
Symptoms involve:
- stiffening of the body
- shaking
- loss of bladder or bowel control
- biting of the tongue
- loss of consciousness.
First aid for seizures
- It is important to note that most seizures do not require emergency medical attention, and you can not stop a seizure once it is in progress.
When you are with somebody having a mild seizure:
- Stay with the person until their seizure ends & they are awake.
- Once they are awake, guide them to a safe place and tell them what happen.
- Stay calm & try to keep other people calm.
- Speak calmly.
- Check for a medical bracelet.
- Offer to assist the person get home safely.
If the person is having a tonic-clonic seizure, which causes the uncontrolled shaking or jerking:
- Ease the person to the ground.
- Turn them gently onto their side to assist them to breathe.
- Clear any dangerous objects away from them.
- Put something soft under their head.
- If they wear glasses, remove them.
- Loosen any clothing, like a tie, that may affect breathing.
- Time the seizure and call 911 if it lasts longer than five minutes trusted Source.
When someone is having a seizure, it is critical to never:
- Grasp the person down or try to stop their movements,
- put anything in their mouth,
- give them mouth to mouth,
- offer the person food or water up till they are fully alert.
What are the causes of epilepsy?

In about half of the people with epilepsy trusted sources, the cause cannot be determined, per the WHO.
Different factors can contribute to the development of seizures, such as:
- traumatic brain injury or other head trauma,
- brain scanning after a brain injury (post-traumatic epilepsy),
- serious illness or very high fever,
- stroke, which causes about half rusted Source of epilepsy cases in older adults when there is no identifiable cause, according to the CDC,
- lack of oxygen to the brain,
- brain tumor or cyst,
- dementia, involving Alzheimer’s disease,
- maternal use of certain drugs, prenatal injury, brain malformation, or lack of oxygen at birth,
- infectious conditions like HIV & AIDS and meningitis,
- genetic or developmental disorders or neurological diseases,
- Epilepsy can develop at any age, yet diagnosis usually occurs in early childhood or after 60 years old trusted Source.
Is epilepsy hereditary?
- Researchers 1st identified genes linked to epilepsy in the late 1990s, according to the Epilepsy Foundation.
- Since then, they have discovered more than 500 genes from trusted sources thought to contribute to its development.
- Certain genes are associated with some types of epilepsy.
- For example, people with Dravet syndrome sometimes have abnormal changes in their SCN1A gene.
- Not all genes linked to epilepsy are passed down through the families.
- Some gene mutations develop in children even if they are not present in either parent.
- These are called “de novo mutations.”
- Certain types of epilepsy are more common in people with a family history, but most children of people with epilepsy do not develop epilepsy themselves.
- According to the Epilepsy Foundation, even if a child has a parent or sibling with epilepsy, the chances that they will develop the condition by age 40 is still less than 5 percent.
- The chances of developing epilepsy are higher if a close relative has generalized epilepsy rather than focal epilepsy.
- If your parent has epilepsy due to another cause like as stroke or brain injury, it does not affect your chances of developing seizures.
- Certain rare conditions, like tuberous sclerosis & neurofibromatosis, can cause seizures. These conditions can run in families.
- Genetics may also make certain people more susceptible to seizures from environmental triggers.
- If you have epilepsy & are concerned about starting a family, consider arranging a consultation with a genetic counselor.
Epilepsy in children

- Epilepsy is a brain condition that causes reoccurring seizures.
- It affects about 470,000 children & 3 million adultsTrusted Source in the United States.
- Seizures are incidences of neurological symptoms caused by changes in your brain’s electrical activity.
- Tonic-colonic seizures, previously known as grand mal seizures, cause a switch of consciousness and full-body convulsions.
- Certain other types of seizures cause symptoms that are not as noticeable.
- According to the Epilepsy Foundation, children with some types of epilepsy are at a heightened risk of developing learning problems and underachieving academically.
- A proper diagnosis and treatment plan are important for assisting your child to navigate potential difficulties caused by epilepsy.
- Remain reading to learn what causes epilepsy in children.
- We will also cover its symptoms and your treatment options.
What causes epilepsy in children?
- About 40 % of trusted sources of epilepsies have no known cause and are attributed to genetic factors.
- Epilepsy is thought to be more usual in people with close family members who also had epilepsy.
- Twin studies suggest that the heritability of epilepsy is somewhere between 25 & 70 percent trusted sources.
The other 60% of epilepsies are often attributed to brain damage caused by one of the following factors:
Head trauma: A traumatic harm to your head can potentially lead to brain damage and epilepsy. Car crashes, sports injuries, and physical abuse are certain potential causes.
Stroke: A stroke happens when impaired blood flow in a blood vessel leads to brain damage.
Brain conditions: Brain tumors, meningitis, and other conditions that conduct to brain damage can potentially cause epilepsy.
Prenatal injury: Factors like developmental brain abnormalities or an oxygen deficit previous birth can potentially lead to brain damage.
Types and symptoms of epilepsy in children
- Epilepsy can cause numerous types of seizures.
- Here are some of the usual types of seizures children who have epilepsy can experience.
Focal seizures
- Focal seizures are too known as partial seizures.
- They only harm one side of your child’s brain and are often preceded by an aura.
- An aura is a sudden uncommon feeling, such as déjà vu or changes in hearing, sight, or smell.
- Focal seizures can be more categorized depending on the specific symptoms.
Focal aware seizures
- Focal-aware seizures typically only harm a specific part of your child’s body, like a leg, and don’t cause a loss of consciousness.
- A person often becomes unable to respond yet can hear and understand their surroundings. These seizures generally last less than two minutes.
Focal impaired awareness seizures
- Focal impaired awareness seizures cause changes in consciousness. They commonly last for less than 2 minutes, and your child will likely seem awake to other people during the seizure. They will have involuntary movement or stiffening of part of the body and may make noises, yet they will not interact or respond normally. They will sometimes appear to fall asleep or faint for a period of several minutes to a few hours after the episode.
Focal to bilateral tonic-clonic seizures
- Focal to bilateral tonic-clonic seizures begin on one side of your child’s brain and spread to both sides.
- During the 1st phase, your child will have impaired consciousness and their muscles will stiffen.
- If standing, they might fall to the floor & their muscles may spasm or jerk.
- These seizures commonly last between 30 seconds and 3 minutes.
Gelastic and dacrystic seizures
- These 2 types of seizures start in your child’s hypothalamus.
- Gelastic seizures cause unmanageable laughter.
- Dacrystic seizures cause unmanageable crying.
- Your child would not lose consciousness during either type.
Generalized seizures
- Generalized seizures harm both sides of your child’s brain.
- They can be subdivided into so many categories.
Generalized tonic-clonic seizures
- Generalized tonic-clonic seizures cause similar symptoms as the focal to a bilateral tonic-clonic seizure.
- The difference is that this seizure begins with both sides of your child’s brain, whereas the bilateral tonic-clonic starts on one side and spreads.
Tonic seizures
- Tonic seizures cause muscle stiffing but do not cause muscle spasms.
- They typically harm your child’s back, legs, or arms.
- They can also occur due to certain medical conditions in people who do not have epilepsy.
Clonic seizures
- Clonic seizures cause muscle jerking motions.
- This type of seizure is relatively rare.
- According to the Epilepsy Foundation, they happen most often in babies.
Absence seizures
- Absence seizures can be mistaken for daydreaming and cause symptoms like blank staring and eyelid fluttering with impairment of consciousness.
- Most of the kids who have absence seizures do not have other types of seizures.
Myoclonic seizures
- Myoclonic seizures cause muscle jerking but do not affect your child’s consciousness.
- They usually last less than two seconds.
- They are often one of several types of seizures that happen as part of childhood epilepsy syndrome.
Atonic seizures
- An atonic seizure causes an unexpected loss of muscle tone.
- This can cause your child to fall if they are standing.
- You may too notice their head drop.
- Atonic seizures can happen as part of childhood epilepsy syndrome.
Epileptic spasms
- Epileptic spasms are brief muscle spasms that last for one to three seconds.
- They often happen several times throughout the day.
- They are referred to as infantile spasms when they happen in children under the age of 2 years, and they can be an indication of severe brain damage in infants.
Childhood epilepsy syndromes
- If your child has a particular group of symptoms, they may be diagnosed with a particular epilepsy syndrome.
- Each syndrome causes a particular pattern of brain activity when measured on an electroencephalogram (EEG).
- These syndromes also usually happen within certain age ranges.
Benign rolandic epilepsy of childhood
- Benign rolandic epilepsy is the most unusual Trusted Source epilepsy syndrome in children.
- It happens in about 15 percent of children with epilepsy and arises between the ages of 3 and 10.
With benign rolandic epilepsy:
- Your child may be seizure-free by the age of sixteen.
- They may have focal aware seizures, commonly at night.
- Focal-aware seizures can grow into generalized tonic-clonic seizures.
Childhood absence epilepsy
- Childhood absence epilepsy affects about 2 to eight percent of people with epilepsy.
- It typically starts between the ages of 4 and 8 years.
With childhood absence epilepsy:
- Most children grow out of it by the time they turn twelve.
- It causes absence seizures that only last many seconds.
- Seizures answer well to medication.
Infantile spasms (West syndrome)
- Infantile spasms begin in your child’s first year.
- They appear as brief muscle spasms that happen in clusters.
- They can happen in children with brain injuries.
- Many children have learning & behavior difficulties.
- It may be a starting symptom of Lennox-Gastaut syndrome.
Lennox-Gastaut syndrome
- Lennox-Gastaut syndrome typically starts between the ages of 3 and 5 years, but it can develop as late as adolescence.
- It may cause tonic, atonic, myoclonic, tonic-clonic, & absence seizures.
- Many children have learning & behavioral problems.
- It is difficult to treat with antiepileptic drugs.
Juvenile myoclonic epilepsy
- Juvenile myoclonic epilepsy begins between the ages of 12 and 18.
- Children sometimes experience myoclonic, tonic-clonic, & absence seizures.
- Your child may experience seizures shortly later waking.
- Seizures sometimes persist into adulthood but can be treated well with medication.
- Tiredness, stress, & alcohol can trigger seizures.
Landau-Kleffner syndrome
- Landau-Kleffner syndrome is a rare condition that typically starts between the ages of 3 and 7.
- This syndrome conducts to problems with verbal expression and understanding of language.
- It commonly causes focal seizures.
Temporal lobe epilepsy
- About sixty percent of people with focal epilepsy have temporal lobe epilepsy.
- Symptoms typically start between the ages of 10 and 20 yet can also develop earlier or later.
- It conducts focal awareness and focal impaired awareness seizures.
- Seizures commonly last less than 2 minutes.
Is there a link joining autism & epilepsy in children?
- Autism spectrum disorder & epilepsy are one and other caused by changes in brain activity.
- Epilepsy is more common in children with autism, but the link still is not fully understood.
- About 20 to 30 percent of trusted sources of children with autism spectrum disorder develop epilepsy previous they turn 18.
What to execute if your child is having a seizure?
- It can be terrifying watching your child have a seizure.
- Yet often, the best thing you can do is wait it out.
- According to the Epilepsy Foundation, the following are the dos & don’ts of assisting a child who’s having a generalized seizure.
Do
- Move anything that could harm your child.
- Put something soft under their head.
- Turn them gently to the side to stop them from choking on their tongue.
- Remain track of how long the seizure lasts.
- Loosen anything around their neck.
- Comfort your child when the seizure is finished.
Don’t
- Try to hold your child.
- Try to end their movements or tongue biting.
- Open or put something in their mouth.
When to seek medical help?
- if it is your child’s first seizure.
- if their seizure lasts more than 5 minutes.
- if it occurs while swimming or in water.
- if your child has a high fever or diabetes.
- if they may have harmed their head.
- if they are having trouble breathing after their seizure.
How is epilepsy diagnosed in children?
- If your child has reoccurrence seizures, their doctor may diagnose them with epilepsy.
- A doctor will likely use different tests to make the diagnosis.
These may involve:
Medical history: They will gather all information about relatives with epilepsy & make a detailed list of your child’s symptoms.
Neurological exam: A doctor will test your child’s mental function & behavior to determine what variety of epilepsy your child has.
Blood test: They may arrange a blood test to rule out infections or other conditions that may cause seizures.
EEG: Electrodes are placed on your child’s scalp, and your child may be asked to perform specific tasks while the electroencephalography measures brain activity.
Imaging tests: The doctor may order many imaging tests to examine your child’s brain for abnormalities.
These tests involve:
- computerized tomography scan (CT or CAT scan),
- magnetic resonance imaging (MRI),
- functional MRI (fMRI),
- positron emission tomography (PET),
- single-photon emission computerized tomography.
Is there a cure for epilepsy in children?
- At this time, there is no known prevention for epilepsy.
- However, getting proper treatment can assist keep seizures under control and lessen potential complications.
How are seizures treated in children?
- The most usual treatment for epilepsy is medication, yet a number of other treatments may also be used.
Medication
- Epilepsy is commonly treated with antiepileptic drugs that assist control symptoms.
- There are dozens of types of antiepileptic drugs available, and your child’s doctor can assist you to determine which one is best for them.
- If your child has been seizure free for several years, the doctor may recommend reducing the amount of medication they are taking.
Ketogenic diet
- A ketogenic diet is a diet that drastically keeps away from carbs.
- This type of diet causes your body to produce a substance called decanoic acid that may reduce convulsive activity in certain people.
Surgery
- For children with frequent & severe seizures, a doctor may recommend surgery to the incision or remove part of the brain.
- Brain surgery can be effective for certain types of epilepsy, but it is usually not performed unless noninvasive treatments have failed.
Neurostimulation
- It may be an option if your child does not respond to medications.
- During neurostimulation, an implanted device delivers less amount of electricity to your child’s nervous system.
Currently, the 3 types of neurostimulation available include:
- vagal nerve stimulation,
- responsive neurostimulation,
- deep brain stimulation.
How do help children live with seizures?
Here are some ways that you can assist support a child with epilepsy:
- knowledge as much as you can about epilepsy, especially the specific type your child has.
- Stay away from making your child feel like a burden.
- Assist your child to understand the dosage of all their medications as well as potential side effects.
- Discuss with your child’s doctor before giving them medications that may interact with their epilepsy medications.
- Encourage your child to get enough sleep and build healthy habits.
- Take your child to look a doctor for regular checkups.
- Make sure your child wears a helmet when playing sports with an increased risk of head injury.
Takeaway
- Genetic factors or brain injury can lead to epilepsy in children.
- Epilepsy can cause a broad range of symptoms that can vary in severity from barely noticeable to severe.
- If you think your child may have epilepsy, it is critical to see a doctor as soon as possible for a proper diagnosis.
- Epilepsy can sometimes be well managed with medication or other treatments.
What triggers an epileptic seizure?
- Certain people identify things or situations that trigger their seizures.
A few of the most usual known triggers are:
- lack of sleep
- illness or fever
- stress
- bright lights, flashing lights, or patterns
- caffeine or alcohol or alcohol withdrawal or medications, or illegal drugs
- skipping meals, overeating, or specific food ingredients
- very low blood sugar
- head injury.
- Identifying triggers is not always easy.
- One incident does not always mean something is a trigger.
- Sometimes, a combination of factors triggers a seizure.
- A good way to find your triggers is to remain in a seizure journal.
After each seizure, note the following:
- day and time,
- what activity you were involved in,
- what was happening around you,
- unusual sights, smells, or sounds,
- unusual stressors,
- what you were eating or how long it had been since you had eaten,
- your level of fatigue & how well you sleep the night before.
- You can use your seizure journal to determine if your medications are working.
- Note how you felt just before and just after your seizure, & any side effects.
- Bring the journal with you when you visit the doctor.
- It may be useful for your doctors if adjusting your medications or exploring other treatments is, or becomes, necessary.
What are the complications of epilepsy?
- Epileptic seizures disturb the electrical activity of your brain, which can directly or indirectly affect many parts of your body.
Potential complications of epilepsy involve:
- learning difficulty (about 20 percent of trusted sources of people with epilepsy have an intellectual disability, according to a 2018 research article,),
- injury from falling during a seizure,
- injury while operating an automobile or machinery,
- depression,
- brain damage from prolonged and uncontrolled seizures,
- choking on food or saliva,
- medication side effects.
- Each year, about 1.16 out of every 1,000 people trusted Source with epilepsy experience unexpected death in epilepsy (SUDEP), according to the CDC.
- SUDEP (sudden unexpected death in epilepsy ) is an epilepsy-related death not caused by drowning, injury, or another known cause. Pauses in breathing, airway obstruction, & abnormal heart rhythm are thought to contribute.
- SUDEP (sudden unexpected death in epilepsy ) is more common in people with epilepsy that is not well managed.
- Taking all your medication as prescribed & visiting your doctor regularly can assist you to minimize your risk.
How is epilepsy diagnosed?

- If you suspect you have had a seizure, see a doctor as soon as possible.
- A seizure can be a symptom of an important medical issue.
- Your medical history & symptoms will assist your doctor to decide which tests will be helpful.
- They will likely give you a neurological examination to test your motor abilities and mental functioning.
- To diagnose epilepsy, more conditions that cause seizures should be ruled out.
- A doctor will probably order a complete blood count (CBC) & the chemistry of your blood.
Blood tests may be used to see for:
- signs of infectious diseases,
- liver and kidney function,
- blood glucose levels,
- Electroencephalogram (EEG) is the most usual test used to diagnose epilepsy. It is a noninvasive and painless test that involves placing electrodes on your scalp to search for abnormal patterns in your brain’s electrical activity. You may be asked to perform a particular task during the test. In certain cases, the test is performed while you sleep.
- Imaging tests can reveal tumors & other abnormalities that can cause seizures.
These tests might involve:
- CT scan,
- MRI,
- positron emission tomography (PET),
- single-photon emission computerized tomography,
- Epilepsy is commonly diagnosed if you have seizures, but there is no apparent or reversible cause.
How is epilepsy treated?
- Treatment for epilepsy may assist you to have fewer seizures or stopping seizures completely.
Your treatment plan will be based on:
- The severity of your symptoms,
- Your health,
- how well do you respond to therapy,
Certain treatment options include:
- Anti-epileptic (anticonvulsant, antiseizure) drugs: Anti-epileptic medications can assist reduce the number of seizures you have. In certain people, they may eliminate seizures. To be majorly effective, the medication must be taken exactly as your doctor prescribed.
- vagal nerve stimulator: This device is surgically placed under the skin on your chest & electrically stimulates the nerve that runs through your neck to prevent seizures.
- Ketogenic diet: According to the Epilepsy Foundation, more than 1/2 of children who do not respond to medications benefit from the ketogenic diet, which is high fat and low carbohydrate diet.
- Brain surgery: The area of the brain that causes seizure activity can be removed or altered if you & your healthcare team determine it is the right treatment for your condition.
- Research into new treatments is ongoing. 1 treatment that may be more widely available in the future is deep brain stimulation. It involves implanting electrodes into your brain & a generator into your chest. The generator sends electrical impulses to your brain to assist decrease seizures.
- The FDA approved the use of deep brain stimulation in 2018 in people over eighteen years old with focal onset seizures who have not responded to at least three anti-epileptic medications.
- Minimally invasive surgeries & radiosurgery are to be investigated.
Medications for epilepsy
- The first-line treatment for epilepsy is an anti-seizure medication.
- These drugs are designed to assist reduce the frequency and severity of seizures.
- They cannot stop a seizure that is already in progress, and they are not a cure for epilepsy.
- These medications are absorbed by your stomach.
- They then carry through your bloodstream to your brain.
- They affect neurotransmitters in a way that decreases the electrical activity that shows seizures.
- There are lots of antiseizure drugs on the market.
- Your doctor can prescribe one drug or a combination of drugs, depending on your type of seizure.
Common epilepsy medications involve:
- levetiracetam (Keppra),
- lamotrigine (Lamictal),
- topiramate (Topamax),
- valproic acid (Depakote),
- carbamazepine (Tegretol),
- ethosuximide (Zarontin).
- These medications are commonly available in tablet, liquid, or injectable forms and are taken once or twice a day.
- Your doctor will initially prescribe the lowest possible dose, which can be adjusted until it begins to work.
- These medications must be taken consistently & as prescribed.
Some potential side effects may involve:
- fatigue,
- dizziness,
- skin rash,
- poor coordination,
- memory problems,
- Rare, yet serious side effects include depression & inflammation of the liver or other organs.
- Epilepsy is different for everybody, yet in most cases, people see improvement with antiseizure medication.
- Certain children with epilepsy may stop having seizures and can stop taking medication.
Is surgery an option for epilepsy management?
- If medication can not decrease your number of seizures, another option is brain surgery.
Resection
- The most usual surgery is resection.
- This includes removing the part of your brain where the seizures start.
- Most sometimes, the temporal lobe is removed in a procedure known as temporal lobectomy.
- In certain cases, this can stop seizure activity.
- In some cases, you will be kept awake during this surgery so doctors can talk with you and avoid removing part of the brain that controls important functions such as vision, hearing, speech, or movement.
Multiple subpial transections
- If the part of the brain is too big or important to remove, surgeons may perform another procedure called a multiple subpial transection, or disconnection.
- During this procedure, the surgeon makes slits in your brain to interrupt the nerve pathway. This slit keeps seizures from spreading to other areas of your brain.
- After surgery, certain people are able to cut down on antiseizure medications or even stop taking them, under their doctor’s oversight.
- There are risks to any surgery, involving a negative reaction to anesthesia, bleeding, and infection.
- Surgery of the brain can sometimes consequence in cognitive changes.
- It can be a good idea to discuss the pros and cons of the various procedures with your surgeon and other healthcare team members.
- You may also want to seek a second opinion previous making a final decision.
Living with epilepsy: What to expect?
- Epilepsy is a chronic disorder that can harm many parts of your life.
- Laws differ from state to state, but if your seizures are not well managed, you may not be allowed to drive.
- Because you never know when a seizure will happen, many everyday activities like crossing a busy street can become dangerous.
- These problems can conduct to loss of independence.
In addition to regular doctor visits and following your treatment plan, here are certain things you can do to cope:
- Keep a seizure diary to assist identify possible triggers so you can avoid them.
- Wear a medical alert bracelet to let people know that you have epilepsy so you get the right medical help if you have a seizure and can not speak.
- Instruct the people closest to you about seizures & what to do in an emergency.
- Seek professional assistance if you have — or think you have — symptoms of depression or anxiety.
- Join an assist group for people with seizure disorders.
- Engage in health-promoting activities like eating a nutrient-rich, balanced diet & getting regular exercise.
Is there a cure for epilepsy?
- Early treatment with medication can assist reduce seizure frequency and the chances of serious complications.
- Epilepsy surgery, meanwhile, is considered curative in most cases.
- Approximately 30 percent of trusted sources of people with partial epilepsy and twenty-five percent of people with generalized epilepsy have seizures that do not respond well to medication.
- If medication fails, your doctor may suggest surgery or vagus nerve stimulation.
- Two types of brain surgery can break down or eliminate seizures.
- One type, called resection, includes removing the part of the brain where seizures originate.
- When the part of the brain responsible for seizures is too vital or large to remove, the surgeon can perform a disconnection.
- This includes interrupting the nerve pathway by making cuts in the brain.
- This remains seizures from spreading to other areas of the brain.
- Dozens of other avenues of research into the causes, treatment, and potential heals of epilepsy are ongoing.
- Although there is no cure at this time, the right treatment can result in a dramatic improvement in your condition and your quality of life.
What are the warning signs of epilepsy?
Temporary confusion—sometimes described as a “fuzzy” feeling.
Staring at the spell.
Unbounded jerking movements of the arms and legs.
Loss of consciousness or awareness.
Psychic symptoms—out-of-body feelings or not feeling “at the moment”
Memory lapses.Can epilepsy go away?
While many forms of epilepsy require lifelong treatment to control the seizures, for certain people the seizures eventually go away.
The odds of becoming seizure-free are not as good for adults or for children with severe epilepsy syndromes, yet it is possible that seizures may decrease or even pause over time.Can you live a normal life with epilepsy?
Most people with epilepsy live their whole life.
However, the risk of early death is higher certain.
We know that the best possible seizure control and living safely can decrease the risk of epilepsy-related death.What triggers epilepsy?
Some factors may increase your risk of epilepsy:
Age.
Family history.
Head injuries.
Stroke and other vascular diseases.
Dementia.
Brain infections.
Seizures in childhood.What is silent epilepsy?
Overview, Absence seizures include brief, sudden lapses of consciousness.
They are more usual in children than in adults.
Someone having an absence seizure may look like he or she is staring blankly into space for some seconds.





16 Comments