Disability With Fibromyalgia
Table of Contents
Definition/Description-
- Fibromyalgia Syndrome is a disease distinguished by chronic pain, stiffness, and tenderness of muscles, tendons, and joints, without noticeable inflammation.
- Fibromyalgia does not cause human body damage or diseases.
- Fatigue affects 90 percent of.
- Fatigue affects 90 percent of individuals and sleep disorders are general.
- Fibromyalgia may be related to other rheumatic conditions, and irritable bowel syndrome (IBS).
- There is no ultimate medical test for the diagnosis of fibromyalgia and fibromyalgia symptoms may come and go over time.
- Diagnosis is dissolved by eliminating other possible causes of the symptoms.
- It may take time to establish which symptom is caused by what problem.
- FMS is NOT just one condition; it’s a complex syndrome that includes many different factors that may severely impact and disrupt a patient’s daily life.
- Fibromyalgia Syndrome (FMS) is reviewed as a systemic difficulty including biochemical, neuroendocrine, and physiologic abnormalities, leading to a disorder of pain processing and perception(i.e. allodynia, hyperalgesia).
- The symptoms correlated with FMS may arise from primary or secondary/reactive causes.
Prevalence-
- FMS occurs in more than 6 million Americans, or 4% of the population, causing it to be the most general musculoskeletal disorder in the U.S.
- It affects mainly females (90%) more often than males.
- Symptoms typically present among the ages of 20-55 years, but a person has been diagnosed as young as 6 years and as old as 85 years of age.
Pathophysiology
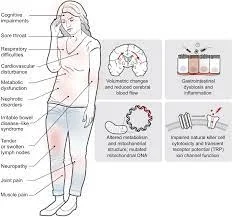
- The pathogenesis of FMS is theorized to be impairment of the central nervous system (CNS), distinguished by central
- sensitization, which is an intensified pain perception accompanied by ineffective pain inhibition and/or modulation.
- This elevated response to peripheral stimuli causes hyperalgesia, allodynia, and referred pain across multiple spinal segments, resulting in chronic widespread pain and reducing the tolerance to the sensory input of the musculoskeletal system.
FMS systemically causes dysregulation- in neurologic, immunologic, endocrinologic, and enteric organ systems,
Autonomic Nervous System-
- The Autonomic Nervous System (ANS) is accountable for regulating the Sympathetic (“fight or flight”) and the Parasympathetic (“rest and digest”) responses.
- With FMS, patients feel the systemically accountable sympathetic (SNS) response with a diminished parasympathetic (PNS) modulation.
- Uninterrupted over-activation of the SNS results in improved heart rate, excessive gastric secretions and contractions, abnormalities of smooth muscle contraction throughout the digestive tract, fast and shallow respiration, and vasoconstriction.
- This may lead to malnourishment due to absorption and digestion disruptions.
- Long-lasting inhibition of PNS make difference in the neuro immunoendocrine systems, directly affecting growth hormone secretion by the pituitary gland.
- This may outcome in nonrestorative sleep, pain, fatigue, and cognitive/mood symptoms.
Immune System-
- The immune response to infection, inflammation, and/or trauma is the liberation of cytokines for local healing, which activate the CNS to release glial cells within the brain and spinal cord for healing support and pain response.
- With FMS, this auto-immune response is accounted for, causing an excess of glia in the human body which produces an overemphasized state of pain (chronic).
Causes of fibromyalgia-
- There are numerous hypotheses of how multiple factors play their role in the development of FMS.
- The exact etiology of FMS is still being researched; although, there are too many potential causes and risk factors, listed below, that are currently associated with, or improved one’s risk for developing this condition.
- Diet.
- Food Pyramid.
- Viral.
- Occupation, seasonal, and environmental influence.s
- Adverse childhood experiences (i.e. PTSD).
- Psychological and cognitive/behavioral factors.
- Other diseases- RA, systemic lupus erythematosus, or AS.
- Present-day research leftovers inconclusive regarding the genetic or hereditary cause of SMS. A family history of FMS is a risk factor.
Characteristics/Clinical Presentation-
- Muscle pain is distinguished as the major symptom of FMS, generally mark out by patients as “aching or burning” regardless of physical activity.
- Other symptoms or associated problems happen, with various reports of frequencies, that may also affect function.
- FMS can cause residual pain sensations at a minor intensity due to repetitive exposure to peripheral stimuli or activity, also known as the “Wind-up Response.”
Symptoms-
Symptoms are often aggravated by:
- Stress.
- Overloading physical activity.
- Overstretching.
- Damp or chilly weather.
- Heat exposure to humidity.
- Sudden change in barometric pressure.
- Trauma.
- Another illness.
- Recent research carried out that functional capacity, upper limb muscular strength, postural maintenance, pain threshold, and anxiety is the most crucial predictive factor of Quality Of Life in women with FMS.
Can a person qualify for disability with fibromyalgia?
- Fibromyalgia (FM) is one of the worst conditions to get approved for as a disability in the United States.
- Because the symptoms are often self-reported, the patient will need medical documents and a doctor to support their case.
- Despite the fact that it’s possible to have a successful claim for FM
Keep in mind that the best chance of getting approved for disability is to have:
- Relevant medical records.
- Laboratory testing.
- doctors’ opinions.
- Statements from friends, family members, and co-workers.
What are the criteria for disability?
- The SSA is accountable for evaluating all disability applications.
- When reviewing the case, the SSA will determine if the patient has a medically determinable impairment (MDI) of FM.
- The criteria and provisions for claiming disability due to FM are adjunct.
- They consisted of symptoms of pain in joints, muscles, and surrounding tissues that must be severe and present for at least 3 months.
- Documented proof that rules out other conditions statements from the patient and others about any restrictions on, or inabilities to perform, the patient’s daily activities whether FM prevents patients from working six or more ongoing signs or symptoms of FM.
These signs or symptoms may include:
- Fatigue.
- Problems with memory or cognition, also known as fibro fog.
- Irritable bowel syndrome (IBS).
- Depression.
- Anxiety.
- Waking up exhausted
- In the past era, doctors would check 18 specific points (11 or more of the 18 tender points were essential to support the diagnosis) to look out how many of them were painful when pressed firmly.
How should a patient document a disability case?
- Documentation is the most important key to a successful disability case.
- This factor is more than supplying the SSA with patients’ medical records.
- If their symptoms result in missed workdays, the patient’s employer may need to provide a statement saying so.
Overall, the application should contain:
- A confirmed diagnosis from a rheumatologist
- Dates of the medical visits, as provided by the doctors, caseworkers, and hospitals contact information for the doctors, caseworkers, and hospitals.
- Patient’s current and relevant medical records, which can include information like the patient’s medications, lab test results, or psychologist visits Residual Functional Capacity (RFC) assessment about the patient’s impairments that the doctor fills out.
- A summary of the patient’s previous job Keeping track of the patient’s symptoms it’s also helpful to keep a fibromyalgia diary.
- This may help the patient to track all the days the patient experiences pain and how it interferes with their normal daily routine.
The patient may take into account:
- Migraine attacks.
- Painful menstrual periods.
- chronic exhaustion.
Assessment by patient’s rheumatologist-
- The patient’s rheumatologist may also give a professional opinion on their limitations.
- This encompasses an assessment of the patient’s ability to:
- Sit, stand, and walk in an 8-hour duties day.
- Lift and carry heavy loads.
- Control fluid movements like bending, balancing, or crawling.
- Maintain punctuality and attendance at work.
How is the patient’s disability application evaluated?
- The SSA takes all documentation into consideration prior to making a decision on the disability application.
- Once a patient relinquishes the application, a team of doctors that works with the SSA will evaluate all of its components.
The team of doctors will also involve the psychologist to see if FM has resulted in any mental impairment. These impairments are based on:
- Memory
- Speed of information processing
- Concentration
- Calculation
- Speech
- Word-finding
- The team interprets the medical information and attempts to predict the impact of the patient’s condition on overall function and well-being.
Fibromyalgia: Work and Disability-
- So many people with fibromyalgia continue to work full or part-time.
- But the chronic pain and fatigue connected with fibromyalgia often make working too difficult.
- If the patient is employed, it’s important to know about managing fibromyalgia symptoms and dealing with pain and fatigue.
- Furthermore, if the patient has tried different jobs and is unable to work, the patient might consider applying for disability.
- Disability can be difficult to get, although, because of rules about work capacity.
Can People With Fibromyalgia Work?
- By self-managing fibromyalgia pain and controlling daily stress, most individuals with fibromyalgia may do almost anything they choose.
- Unless the patient has physical pain that’s directly work-related, the patient should be able to make simple modifications to their workplace that allow the patient to continue working.
Workplace refinement for people with fibromyalgia disability-
- Individuals with fibromyalgia can use the following lists when talking with their employer about making modifications.
- They contain put forwardness for accommodations employers should be willing to think about for employees with fibromyalgia.
To communicate concentration issues, employers should consider:
- Providing written job instructions when possible.
- Prioritizing job assignments and providing more structure.
- Allowing preferable work hours and allowing a self-paced workload.
- Allowing periodic rest periods to reorient.
- Providing memory aids, like schedulers or organizers.
- Minimizing distractions.
- Reducing job stress.
To communicate depression and anxiety, employers should consider:
- Forshorten distractions in the work environment.
- Providing to-do lists and written instructions.
- Prompted the employee of crucial deadlines and meetings.
- Allowing time off for counseling.
- Give them clear expectations of responsibilities and consequences.
- Giving sensitivity training to coworkers.
- Giving short breaks to use stress management techniques.
- Developing strategies to deal with work difficulties before they arise.
- Permitted telephone calls during work hours to doctors and others for support.
- Giving information on counseling and employee assistance programs.
To monologue fatigue and weakness, employers should consider:
- Decreasing or eliminating physical exertion and workplace stress.
- Scheduling periodic rest recesses away from the workstation.
- By giving a preferably flexible work schedule and flexible use of leave time.
- Allowing the employee to work from home.
- Carry through the ergonomic workstation design.
To monologue migraine headaches, employers should consider:
- Giving the task lighting.
- Reducing the fluorescent lighting.
- Providing air purification devices.
- By giving preferably flexible work hours and working from home.
- Allowing periodic rest breaks.
To address issues connected with sleep problems, employers should consider:
- Give them flexible work hours and frequent breaks.
- Allowing the employee to work from home.
FAQ
Fibromyalgia, a chronic pain disorder, as well as known as fibromyositis, fibrositis, muscular rheumatism, and FM, is a disabling
the condition that causes the uttermost suffering for millions of people in the United States.
If a person believes that they will not be able to work for a year or more, think about applying for Social Security Disability
Insurance (SSDI) benefits. Most long-term disability insurance policies require the person to apply for SSDI benefits. Furthermore,
the Social Security Administration (SSA) recognizes fibromyalgia as a disability.
Fibromyalgia can receive a disability rating of 40%, 20%, or 10%. Some old timers have more than one service-related sickness or
injury. When that is the case, the old ones consider all conditions to calculate a mutual disability rating. This rating cannot exceed
100%.
Unusual Symptoms of Fibromyalgia include-
Paresthesia.
Brain Fog. Also called “fibro fog,” this symptom is one of the most infuriating ones and it leads to many people in distress.
Allodynia.
Smell and Sound Sensitivity.
Extreme Sweating.
Lipomas.
Dystonia.
The short answer is yes, a person can, but the Social Security Administration (SSA) has orthodox rules that make it more difficult
to receive financial assistance for a medical disorder.