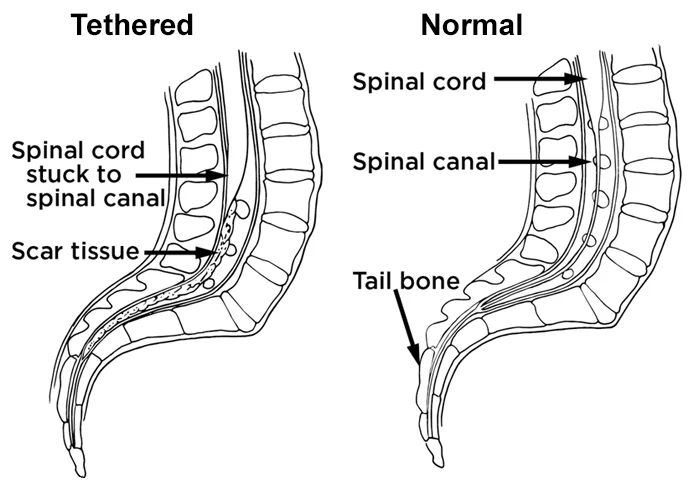
Tethered spinal cord syndrome
Table of Contents
What is a Tethered spinal cord syndrome?
- Tethered spinal cord syndrome is a neurologic disorder caused by tissue attachments that restrict the movement of the spinal cord within the spinal column. Tethered Cord Syndrome (TCS) is an extensive term that embraces both inherited (primary) and acquired (secondary) pathologies that anchor, elongate, and tension the spinal cord.
- The spinal cord fixation produces mechanical stretch, deformity, and ischemia with daily activities, growth, and development. This prevents the spinal cord from actively moving, which then increases stress with flexion and extension movements of the spine.
- Abnormalities are due to problems with secondary neurulation and are jointly related to spina bifida occults, tumors, lipomas, and infections. Ischemic injury from the traction of the conule directly correlates with the degree of degeneration metabolism and degree of neurological settlement.
- In addition to ischemic injury, traction of the conule by the filament may also mechanically alter the neuronal membranes, resulting in altered electrical activity.
- Depending on the age and intrinsic cause of the tethered cord, various signs and symptoms can manifest, including lower extremity and saddle pain, motor and sensory loss, urinary disorder, orthopedic abnormality, and cutaneous movement.
Etiology
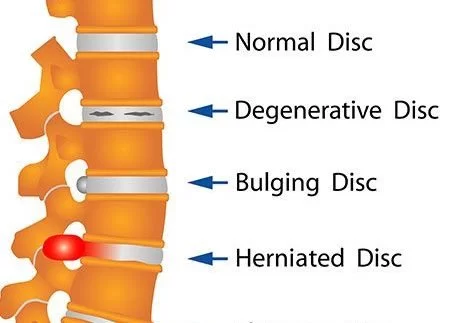
- tethered spinal cord syndrome can be subdivided into congenital and acquired groups. myelomeningocele is the most common congenital etiologies, including dermal sinus tract, lipo-myelomeningocele, fibrous or fibro-adipose filum termination, and diastematomyelia. acquired etiologies for tethered cord syndrome involve spinal cord tumors and scar formation.
Primary Tethered Cord Syndrome
When focusing on primary TCS, the simplest mechanism by which the caudal spinal cord capitulates to tethering is due to a thickened filum terminal. Normally, the filum terminal is a viscoelastic structure that facilitates the increase of the conus medullaris during neural development. During secondary neurulation, improper canalization of the neural tube allows for precursor cells (most commonly preadipose cells) to generate and differentiate, leading to a thickened ‘fatty’ filum terminal. This dedication prevents the ascent of the medullary, resulting in an abnormally broad spinal cord. An unusually thickened filum terminal was classified by Hoffman and colleagues in the 1970s as being greater than 2 millimeters in diameter Lipomas, or adipose cell aggregation, around the rear aspect of the spinal cord, have also been linked to TCS. Lipomas associated with TCS are ordinarily subpial in location, whereas subdural lipomas are a lot less associated with this determine. The presence of a lipoma can affect both the filum terminal as well as the conus medullaris, essentially leading to an elongated spinal cord and if large evoke, may elicit spinal compression as well. Spinal Dysraphism, which is any disorder that results in impairment of the spinal cord, has also been linked to TCS. Spina bifida occult as splatter cord malformations such as diastematomy
Secondary Tethered Cord Syndrome
Secondary or acquired tethered cord syndrome can be due to a multiplicity of sources that elicit the fibrotic thickening of the filum terminal such as infection fibrotic damage and the presence of a tumor. the further potential root of secondary TCS could be due to muscular thickening following spinal surgery. however, it is said that these creatures most likely possessed abnormal tethering prior to the surgery.
Pathophysiology
The preceding mechanisms apply their effect on the spinal cord in a few different appearances. demonstrated that after sustained or intermittent traction to the spinal cord, oxidative metabolism was decreased overall. It was suggested that this was likely due to the overall ischemic effect of spinal traction, which leads to afterward neural cells becoming hypoxic. Other preferred mechanisms suggest that the convulsion of ion channels is also associated with neuronal membrane traction, ultimately contributing to the decreased capacity for oxidative metabolism. Collectively, these mechanisms directly obtain neuronal dysfunction through progressive damage on the caudal spinal cord and can worsen over time.
Epidemiology
Tethered cord syndrome is normally recognized only after the onset of signs and symptoms found incidentally when looking for unrelated problems. Due to this, the true incidence and currency in the general population are not known. However, the onset of symptoms suggests appearing more commonly in childhood than in adulthood.
Primary Causes and Symptoms
In enlargement to myelomeningocele and lipo -myelomeningocele consider the following other causes of tethered cord that vary in severity of symptoms and treatment:
Dermal sinus tract (a rare congenital deformity)
Diastematomyelia (split spinal cord)
Lipoma (a benign, fatty growth)
Tumor
Thickened/tight filum terminal (a delicate filament near the tailbone)
A history of spine trauma
A history of spine surgery
Symptoms in Children
The indication listed below are some of the approaches in which tethered spinal cord syndrome may be exhibited in children:
Lesion on the lower back
Skin discoloration on the lower back
Hairy patch on the lower back
Back pain aggravates under activity and is relieved by rest
Leg pain mostly in the back of the legs
Leg numbness or tingling
Changes in leg strength
Deterioration in gait
Progressive or repeated muscle contractions
Leg deformities
Spine tenderness
Scoliosis (curvature of the spine)
Bowel and bladder problems
while it is rare, a patient with tethered spinal cord can continue under treatment into adulthood. In similar cases the stress on the spinal cord increases leading to increasing sensory and motor problems as well as loss of bladder and bowel control.
Diagnosis
If a tethered spinal cord is suspected one or more tests may be required to confirm the diagnosis.
MRI: A diagnostic test that uses powerful magnets and computer mechanics produces three structural images of body structures that can show the spinal cord, nerve roots, and surrounding areas as well as enlargement, degeneration, and displacement.
Myelogram: An x-ray of the spinal canal following injection of contrast material into the thecal sac can show pressure on the spinal cord or nerves caused by tethered spinal cord
CT or CAT scan: A symptomatic image created after a computer reads x-rays may be used after a myelogram to show how the dye flows around the spinal cord and nerves.
Ultrasound: A water-soluble gel is placed on the skin site the transducer (a handheld device that directs the high-frequency sound waves to the spine) is to be placed. The gel assists to transmit the sound to the skin surface. The ultrasound is rotated and images of the spinal cord moving in the thecal cavity are obtained.
Treatment of Tethered spinal cord syndrome
Treating tethered cord syndrome usually involves surgery to release the spinal cord from the tissue. This surgery is called a laminectomy and usually involves dislodging a few parts of the bones (called bone spurs) or tissues from the lower part of the spinal cord. This process enables the surgeons to approach the area around the spinal cord and enlarges the spinal canal, which relieves pressure on the cord and the nerves around it. If the patient has mostly back pain and mild weakness, a course of physical therapy may provide tethered cord treatment. This approach requires the patient to be old and suitable to reliably convey whether the symptoms are worsening or improving. In most cases, surgical treatment of tethered cords is needed to prevent neurologic degeneration. A laminectomy is performed, the dura is opened, and using the operating microscope, the spinal cord is released from the tethering structure. If practicable, the tethering part is removed.
Physical Therapy
Currently, there is a lack of evidence on physical therapy related to this disorder seeing as the primary mode of treatment is surgical intervention. That being said below is a list of important ideas that need to be advised as previously mentioned one of the causes of TCS is spinal lipomas. In this case, symptoms may be exaggerated in patients who experience rapid weight gain as the lipoma may increase in size. Therefore if neurological defaults in patients are not severe weight loss may be a beneficial treatment to be considered before any surgical intervention. This could be achieved between proper dieting and exercise that does not require excessive tension and bending in the spinal cord. It has been noted that individuals with less severe cases of tethered cord syndrome may endure symptom-free in childhood, but neurological deficiency may occur later in life due to repeated spine flexion, extension, or trauma that may aggravate signs. Therefore, it is imperative that patients receive proper education on posture, gait, and functional movements when participating in refreshments and daily activities in order to limit progressive tension in the spinal cord. Patients with a walking disorder can be treated with an exercise program to make walking comfortable and effortless.
Prevention
In children with TSCS, early surgery is usually suggested to prevent further neurological degeneration. If surgery is not suitable spinal cord nerve roots may be cut to relieve pain. In adults surgery to separate (dee tether) the spinal cord can reduce the size and further development of injury in the cord.
FAQs
A tethered spinal cord is a spinal cord that is drawn down and stuck or fixed, to the spinal canal. The spinal cord normally flows freely surrounding the spinal canal.
As a child develop, the spinal cord must be able to move freely surrounding the spinal canal. If the spinal cord is attached, it will stretch like a rubber band as a child develop. This container cause lasting damage to the spinal nerves.
Diastematomyelia (split spinal cord)
Lipoma (a benign, fatty growth)
Thickened/tight filum terminal (a delicate filament near the tailbone)
Tumor
A history of spine trauma
A history of spine surgery
Tethered spinal cord main treatment for surgery. In this method, the spinal cord is released from the circumambient spine so that it can transfer freely. If treated immediately, any damage resulting due to the tethered spinal cord can often be prevented.
In adults, symptoms of tethered cord normally develop slowly. However, if left untreated, these symptoms may become quite present. Common symptoms include back pain that separates the legs, hips, and rectal or genital areas. Many also describe feelings of weakness or numbness in the legs, as well as muscle loss.
Tethered Cord Syndrome is usually caused by a mistake in normal fetal development, resulting in conditions like dermal sinus tract, diastematomyelia (split spinal cord), lipoma, tumor, spina bifida, or a tight filum terminal.
After surgery, patients require to remain flat for 24 to 36 hours to minimize the risk of a spinal fluid leak. Physical activity is limited for the next many weeks to allow the surgical site to heal, but most surgical patients have excellent outcomes and container quickly resume normal activities.