Botox for Trigeminal Neuralgia
Table of Contents
Introduction of botox for trigeminal neuralgia
Botox is the name for Botulinum toxin type A, which is derived from a strain of bacteria called Clostridium Botulinum.
Botox injections block certain chemical signals from nerves, most of the signals that cause muscles to contract. The most common use of these injections is to temporarily relax the facial muscles that cause contractions in the forehead and around the eyes. Injections of botox are also used to treat some other conditions.
Patients with Trigeminal neuralgia that have easily identifiable trigger points, permanently contracted muscles, or pain that are associated with muscle spasms are very good candidates for Botulinum Toxin A injections. When Botox is injected into a muscle, it blocks the signals sent from the brain which gives a signal of muscle contraction. Botox targets the muscles which are involved. The body feels that there is no pain being experienced. Botox can help to keep the muscles relax for anywhere from three to six months, after that it is hoped that muscle works normally.
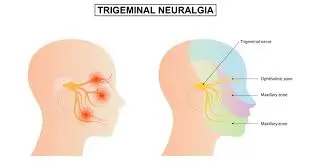
Trigeminal neuralgia is a long-term pain disorder that affects the Trigeminal nerve, the nerve responsible for sensation in the face and movement of the face such as biting and chewing. It is a chronic condition that can cause sudden, intense painful episodes, typically on one particular side of the face, that can disrupt daily activities. People who have this condition say the pain might feel like an electric shock, lancinating or electrical in sensation & severe that the affected person cannot eat or drink. The pain travels through the face in a few seconds, but as the condition progresses, the pain can last minutes & even longer & it can sometimes be intense.
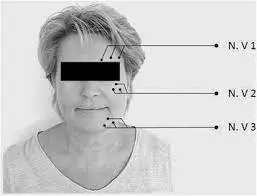
It is a condition characterized by pain that arrives from the trigeminal nerve, which starts near the top of the ear and splits into three branches, toward the eye, cheek, and jaw. It is a form of neuropathic pain. We have two trigeminal nerves for each side of the face, but Trigeminal neuralgia pain most commonly affects only one side.
The pain attacks are said, by those affected, to feel like stabbing electric shocks, burning, sharp, pressing, crushing, exploding, jabbing, or shooting pain that becomes intractable. Pain occurs with facial spasms. There are many conditions that may cause trigeminal neuralgia, but it is typically caused by a blood vessel exerting pressure on the nerve near the brain stem which causes irritation of the nerve.
Botox treatment for Trigeminal Neuralgia:
Onabotulinum toxin A is the serotype(A, B, C1, C2, D, E, F, and G) of botulinum neurotoxin. It was reported to be effective for cases of TN BTX-A was mostly administered intradermally and subcutaneously.
Botulinum neurotoxin has been the most popular artistic procedure performed by plastic surgeons. Botulinum neurotoxin type A was approved for facial aesthetics as the first botulinum toxin type A (BT-A).
Botulinum drugs are complex mixtures of compounds, non-toxic proteins, and excipients (stabilizers like human serum albumins, sugars included and buffers may be found as well to caliber the PH value). Whether and how Botox can have anti-depressive and anti-inflammatory effects are still a matter of debate.
Botox is injected into the muscle, which blocks the signals sent from the brain and tells the muscle to contract. Botox targets the muscles involved by effectively disarming them & ensures that they do not send panic signals throughout the body.
The body accepts that there is no pain being experienced. Botox can help to keep the muscle relaxed for anywhere from 3 to 6 months, after which it is hoped that the muscle will be able to contract normally without pain or spasms.
Is botox FDA approved for trigeminal neuralgia?
Let patients know that Botox is not FDA (food and drug administration) approved for the treatment of severe facial pain associated with trigeminal neuralgia.
What is the mechanism of action of Botulinum toxin?
The main outcome of botulinum toxin type-A is muscle contraction because of its binding to the presynaptic nerve endings, thus inhibiting the release of acetylcholine. It produces its antinociceptive effect in trigeminal neuralgia by several mechanisms.
A direct analgesic action has been recognized, suggesting that botulinum toxin might act through an alternative mode of action.
Most hypotheses assume that Botulinum toxin type A inhibits the release of Ach as well as other neurotransmitters. Inhibition of the release of these neurotransmitters from nociceptive nerve
endings can lead to pain relief.
The second site for botulinum toxin type-A action to produce an analgesic effect could be postganglionic
sympathetic nerve endings utilizing norepinephrine and adenosine triphosphate as neurotransmitters.
Norepinephrine is elevated in chronic pain, & ATP is involved in the stimulation of muscle nociceptors. It has been postulated that Botulinum toxin type-A may inhibit the release of these neurotransmitters and produce an analgesic effect in cases of sympathetically maintained pain involved in the complex regional pain syndrome.
Site of injection for Trigeminal Neuralgia:
Some doctors inject botox into the corresponding dermatome.
In medical terms, the action of Botox is selective muscle denervation. Usually, for muscle contraction, a nerve sends a signal to the muscle. The point where the nerve & the muscle meet is known as the neuromuscular junction. When the signal gets to the neuromuscular junction a chemical called acetylcholine is released from the nerve & binds to the muscle side of the junction causing more chemical reactions that make the muscle contract.
What is the procedure of Botulinum toxin application?
Botox injections are performed as an outpatient procedure with patients free to leave as soon as the treatment has been administered.
Initially, the doctor spends time identifying the individual trigger points, sometimes with the help of a physiotherapist and they will mark the areas with a pen. The marked areas will then be sterilized with a chlorhexidine antiseptic spray and a fast-acting local anesthetic will be injected through a small cosmetic needle.
Botox can then be administered in one of three different ways, depending on the case. Tiny cosmetic needles are preferred, but a Stimuplex nerve stimulator or ultrasound guidance is sometimes necessary if the trigger points are more difficult to access.
Normally 100 units of Botox are administered but it can increase up to 200 units depending on the affected area.
BTX-A crystals were diluted with 2 ml 0.9% saline to 50 U/ml prior to use. These injections of BTX-A were administered intradermally or submucosally at the trigger sites using a 1-ml syringe with a 0.45×16-mm needle by experienced clinicians, and the injection depth was −0.1 cm.
For patients who required injection at multiple sites, 15–25 injection sites in total were located at a distance of 15–20 mm between them. Each area received one injection with 1.25–5.0 units (0.025–0.1 ml) of BTX-A during the first course of the treatment and the patient’s response to the treatment was monitored.
For injection to the maxillary root, the patient was in a sitting position, and their head was supported by a headrest. At the upper edge of the zygomatic arch, midway between the external ear & the orbital rim, the needle was pointed toward the zygomatic bone on the other side of the skull, forming an angle at a depth of 50 mm around the pterygopalatine ganglion.
For injection to the mandibular root, the position was the same. Their mouths were slightly open. The needle was pointed transversely along the base of the skull towards the middle & inserted below the middle through the lower edge of the zygomatic arch. After reaching the pterygoid process, the needle was withdrawn a bit and rotated craniodorsally about 5 to 10 mm and the solution was administered throughout the trigeminal ganglion.
If pain involves the oral mucosa, injections were given submucosally in the oral mucosa with 2.5 U at each site in the way described above. During the procedure, injections in deep parts such as muscles were avoided to prevent unwanted effects on underlying muscles.
In addition, patients who required rescue analgesic medication were allowed to use their current opioid or non-opioid analgesics as clinically indicated. These include NSAIDs, COX-2 inhibitors, acetaminophen as well as topical analgesics.
For certain patients who did not show any symptom improvement within 2 weeks following the initial injection, additional injections were administered in the same areas (each area received one injection with 1.25–5.0 units BTX-A during the second course of the treatment).
Classification based on dosage
- Patients who received a total dose of <40 units were assigned to the low-dose group,
- Patients who received a total dose from 40–70 units were stratified into the medium-dose group and
- Patients who received a total dose of >70 units were classified into the high-dose group.
What are the side effects of Botulinum toxin?
- The patient can have swelling, Pain, or bruising at the injection site
- Headache or flu-like symptoms
- Eye dryness or excessive tearing
- Droopy eyelid or cockeyed eyebrows
- Crooked smile or drooling
Due to the diffusion of toxins into the systemic circulation, there is a possibility of antibody production and the potential for immune-mediated and other long-term complications. The development of antibodies to toxins may be related to exposure to high doses.
What is the outcome of botox treatment?
The beneficial effect of BTX-A on Trigeminal Neuralgia is indicated by a decrease in the degree of pain which was observed as early as 1 week following the first injection. For patients whose symptoms were not improved within two weeks following the first injection, additional doses were administered at the same site as the first injection.80% of pain alleviates with additional injections.
Neurotoxin relaxes striated muscle by way of inhibiting acetylcholine’s release from presynaptic nerve terminals blocking the neuromuscular junction. Although it is widely accepted that its therapeutic effects are confined to the peripheral nervous system, its actions at distant and central sites are also presumed. These central effects may be the result of haematogenic spread, and retrograde neural transport of BT to the central nervous system. However, inhibition is only temporary.
One proposed theory for BT-A relieving pain is by settling muscle trigger points. And it has been reported that around 72% of patients have myofascial trigger points. From this, it is possible to conclude that BT might be useful in 70% of patients with Trigeminal Neuralgia.
In dentistry, controlled clinical trials have demonstrated great efficiency in pathologies such as bruxism, temporomandibular joint disorders, neuropathic pain, and more.
The effect of BTX-A remains throughout the initial 6 months of the follow-up.
One of the main advantages of Botox is that there is little or no recovery time, and most patients feel fine and can return to their normal life immediately. The outcome of treatment should last around three to six months and the procedure can be repeated after this time.
What are the complications of botulinum toxin?
Although with less probability it is possible for the toxin of injection to spread in the patient’s body. Call the doctor right away if you notice any of these effects hours to weeks after receiving Botox:
- Muscle weakness
- Vision problems
- Trouble speaking or swallowing
- Breathing problems
- Loss of bladder control
- Doctors generally recommend against using Botox when the patient is pregnant or breastfeeding. And Botox should not be administered to patients who are allergic to cow’s milk protein.
What are the contraindications of Botulinum toxin?
Botulinum toxin is not given in patients with known hypersensitivity reaction or allergy to botulinum toxin human albumin.
Botulinum toxin is not suggested in patients with neurological diseases such as myasthenia
gravis, multiple sclerosis, and Eaton-Lambert syndrome. Botulinum toxin injections must be avoided in patients taking aminoglycosides as they interfere with neuromuscular transmission.
The use of botulinum toxin during pregnancy and lactation remains questionable. The majority of clinicians recommended avoiding its use until the end of pregnancy.
The treatment of nursing mothers is also controversial. Although botulinum toxin effects seem to
be localized, its concentration in human milk and its impact on nursing babies are unknown. Until safe recommendations are available for its utilization, it should be better avoided in pregnant and lactating mothers.
If patients are in poor general health, their skin is very thick or they have existing muscle weakness at the proposed injection site, the patient may not be a good candidate for Botox. Patients with sensitive skin might experience an allergic reaction at the injection site.
Physiotherapy treatment for Trigeminal Neuralgia after Botulinum toxin:
Physiotherapy treatment promotes general well-being and helps to reduce pain by the use of different techniques. The physiotherapy treatment of trigeminal neuralgia focuses on the patient’s goals and needs.
- Transcutaneous Electrical Nerve Stimulation (TENS)
- LASER therapy
- Interferential Therapy (IFT)
- A hot moist pack was applied to the neck and trapezius muscle for 10 minutes, To reduce muscle spasms
- Ultrasound
- Physiotherapy Management will also aim at reducing pain and improving the ability to carry on with the activities of daily living
- Acupuncture to relieve facial pain and pressure
- Isometric neck exercises
- Stress management
- Relaxation techniques such as deep breathing exercises
- Cardiovascular exercises to improve general health and fitness levels
- self-massage education
- use a scarf to avoid exposure to the cold environment on the affected side of the face
- Functional Activities for problems associated with activities of daily living
- Avoid the use of cold water for drinking and washing your face
Complementary management
- Yoga.
- Meditation.
- Creative visualization.
- Acupuncture.
- Chiropractic.
- Aromatherapy.
- Low-impact exercise.
- Supportive counseling or therapy.
- Biofeedback.
- Vitamin therapy.
FAQ(Frequently asked question)
How successful is Botox for trigeminal neuralgia?
Botulinum toxin type A injection therapy is a safe and effective method for the management of trigeminal neuralgia. No contrast between dosages of botulinum toxin type A was found. Maximum efficacy was observed between 6 weeks and 3 months after the procedure.
Can Botox cause trigeminal nerve damage?
There is no relation between Botox and Trigeminal neuralgia. There have been no reported complications such as trigeminal neuralgia after Botox injections, or complications to the nerve.
Do and don’ts after Botox?
The patient should not lie down for at least 3 hours after receiving Botox. They should not go into any saunas, hot tubs, or tanning booths for at least 4 hours. This will helps to prevent bruising because heat can raise blood pressure. Otherwise, the patient can resume their regular activities right after getting Botox.
What happens after years of Botox?
After some time repeated injections of Botox to a particular region in the body can also cause permanent paralysis of the muscle. This is by far one of the very important and dangerous side effects of using Botox injections. The toxins can spread to the surrounding tissues and this can prove to be fatal.
How long does it take for Botox to set in?
Botox is injected with a fine needle into the specific muscles with minor discomfort. It usually takes three to seven days to take full outcome, and it is best to keep away from alcohol starting at least one week before the procedure.
Do any medications interfere with Botox?
Some things that might interact with this drug include certain antibiotics like aminoglycosides such as gentamicin, polymyxin, Anticoagulants such as warfarin, Alzheimer’s disease drugs such as galantamine, rivastigmine, tacrine, Myasthenia Gravis drugs such as ambenonium, pyridostigmine, quinidine.
what is the cost of Botox?
Most people require more than one injection to achieve the desired results. On the other hand, botox is measured in units and typically costs around $10 to $15 per unit. For example, An average dosage of 30-40 units might be required to treat the forehead and eye area, making the total cost around $300 to $600.