Trigeminal Neuralgia
Table of Contents
What is Trigeminal neuralgia?
- Trigeminal neuralgia (TN ), also known as Tic Douloureux, Trifacial, or Fothergill Disease, is a long-term pain disorder that affects the Trigeminal nerve, the nerve responsible for sensation in the face and movement of the face such as biting and chewing.
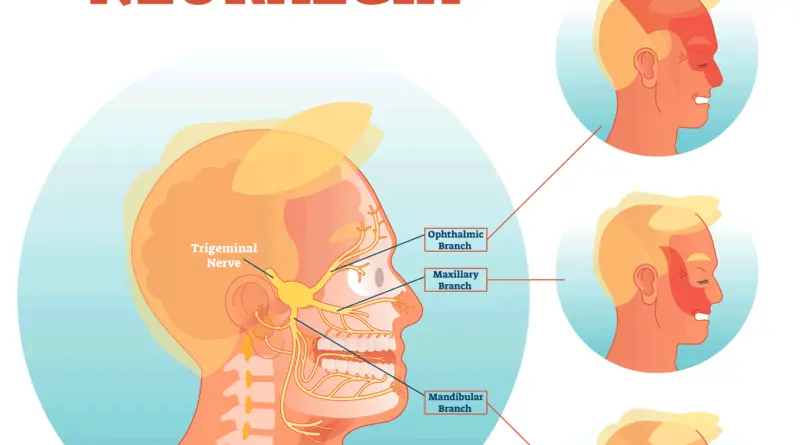
- Trigeminal neuralgia is a condition characterized by pain that arrives from the trigeminal nerve, which starts near the top of the ear and splits into three branches, toward the eye, cheek, and jaw. It is a form of neuropathic pain. We have two trigeminal nerves for each side of the face, but Trigeminal neuralgia pain most commonly affects only one side.
- The pain of Trigeminal neuralgia is not like other facial pain caused by other problems. Trigeminal neuralgia is a chronic condition that can cause sudden, intense painful episodes, typically on one particular side of the face, that can disrupt daily activities. People who have this condition say the pain might feel like an electric shock, lancinating or electrical in sensation & severe that the affected person cannot eat or drink. The pain travels through the face in a few seconds, but as the condition progresses, the pain can last minutes & even longer & it can sometimes be intense.
- This chronic pain affects the trigeminal nerve, which carries sensation from the face to the brain. If a patient has trigeminal neuralgia, even mild stimulation of the face — such as from brushing your teeth or putting on makeup, or wiping your face — may trigger a thrust of excruciating pain. Trigeminal neuralgia more affects women than men, and it’s more likely to occur in people who are older than 50 of age.
- Trigeminal neuralgia is a condition defined by intense facial pain that can disrupt your normal, daily activities. Activities as simple as smiling, talking, chewing, brushing teeth or shaving can trigger brief bouts of intense pain. Though these painful episodes are short-lived, the pain can return sporadically, Or the patient might also experience constant pain that isn’t as severe. The pain typically involves the jaw & lower face, however sometimes it affects the area around the nose and above the eye.
- A patient may initially experience mild & short attacks. But trigeminal neuralgia can progress and cause longer, more-frequent bouts of flaming pain. they are described as a ‘lightning bolt’ stuck on the face or a stabbing sensation on the face. Actually, such short-lasting attacks of pain occur multiple times throughout the day debilitating the patient. It usually happens in short & unpredictable attacks that can last from a few seconds to about 2 minutes.
- Typically, Trigeminal neuralgia is unilateral means that affects only one side of the face. If it is bilateral, both sides of the face will be affected, though not at the same time. Bilateral Trigeminal neuralgia is extremely rare. More interesting is the right side of the face is usually more affected by this condition than the left.
- Although Trigeminal neuralgia can’t always be cured, there are treatments available to alleviate the debilitating pain. Generally, the first treatment of choice is anticonvulsant medicines. Surgery can also be an effective option for those who become unresponsive to medications or for those who suffer serious side effects from the medications.
- Because of the variety of treatment options available, having trigeminal neuralgia doesn’t necessarily mean that patient is doomed to a life of pain. Doctors usually can manage trigeminal neuralgia with medications, injections, or surgery.
What are the symptoms of Trigeminal Neuralgia?
This disorder is distinguished by episodes of severe facial pain along the trigeminal nerve divisions.
A flare-up of trigeminal neuralgia may start with tingling or numbness in the face. Pain occurs in intermittent bursts that last from a few seconds to two minutes, becoming more and more frequent until the pain is almost continuous.
An individual attack generally lasts from a few seconds to several minutes or hours, but these can repeat for hours with very short intervals in attacks. In another case, only 4–10 attacks are experienced daily. The episodes of intense pain may occur in attacks.
To describe the pain sensation, people often have a trigger area on the face so sensitive that touching or even air can trigger an episode; nevertheless, in many people, the pain is developed spontaneously without any apparent stimulation. Which affects lifestyle as it can be triggered by everyday activities.
The attacks are said, by those affected, to feel like stabbing electric shocks, burning, sharp, pressing, crushing, exploding, jabbing, or shooting pain that becomes intractable. Pain occurs with facial spasms.
Most patients complain that their pain begins spontaneously and seemingly out of nowhere. Other patients complain that their pain follows a car accident, a blow to the face, or dental work.
The pain also tends to occur in cycles with suspension lasting months or even years. Pain attacks are known to getting worsen in frequency or severity over time, in some people. Pain might migrate to the other branches over time but in some people remains very stable. Pain is determined at one spot or spread in a wider pattern.
Pain rarely occurs at night while sleeping. Some patients suffer less than one attack a day, while others experience a number of or more every hour. The pain typically starts with a sensation of electrical shocks that peaks in an excruciating stabbing pain within less than 20 seconds. The pain often leads to patients with uncontrollable facial twitching.
Nevertheless, not all people will have the same symptoms as described above there are variants of Trigeminal neuralgia.
Bilateral trigeminal neuralgia which occurs on both sides is very rare except for trigeminal neuralgia caused by multiple sclerosis. This normally indicates problems with both trigeminal nerves, since one serves trigeminal neuralgia on the left side of the face and the other serves the right side. Occasional reports of bilateral trigeminal neuralgia show successive episodes of unilateral pain switching the side of the face rather than pain occurring simultaneously on both sides.
The rapid spreading of the pain, bilateral involvement, or simultaneous participation with other major nerve trunks may suggest a systemic cause. Systemic causes can include multiple sclerosis or cranial tumors.
The severity of the pain makes it difficult to wash the patient’s face, shave, and perform good oral hygiene. The pain has a remarkable impact on daily living activities especially as sufferers live in fear of when they are going to get their next attack of pain & how severe it will be. Which can cause severe anxiety & depression.
Trigeminal pain can also occur after herpes zoster. Postherpetic neuralgia has the same indication as in other parts of the body. Herpes zoster oticus typically presents with the inability to move many face movements, taste loss on the front of the tongue, dry eyes and mouth, pain in the ear, & a vesicular rash. Less commonly varicella-zoster infections involve the facial nerve and result in this occurring.
Trigeminal deafferentation pain also termed colloquially or anesthesia Dolorosa, as phantom face pain, is from intentional damage to a trigeminal nerve following attempts to surgically fix a nerve problem. normally this pain is constant with a burning sensation and numbness. It is very difficult to treat as further surgeries are usually ineffective and possibly detrimental to the person.
symptom triggers
Attacks of Trigeminal neuralgia can be triggered by certain things or movements, such as:
- Eating and drinking.
- Drinking hot or cold beverages
- talking
- smiling
- Blowing the nose
- chewing
- brushing your teeth
- washing your face
- a light touch
- shaving or putting on make-up
- swallowing
- a cool breeze or air conditioning
- head movements
- vibrations, such as traveling in a car
- However, pain can happen spontaneously even with no trigger whatsoever.
What is the prevalence of Trigeminal Neuralgia?
Trigeminal Neuralgia is more common in females than males and the right side of the face is more involved than the left side, it is more commonly found in rural populations than the urban populations.
What are the Risk factors for Trigeminal Neuralgia?
The following have been identified as important risk factors for Trigeminal neuralgia:
- Increased age
- Stroke
- Tumors in the trigeminal nerve region
- Hypertension in women
- Charcot-Marie-Tooth Disease
Which are the main types of Trigeminal Neuralgia?
There are two main types of trigeminal neuralgia:
- Typical trigeminal neuralgia. The patient will experience painful episodes that are sharp, sudden, intense, and sporadic. The patient may feel pain or a burning sensation all over the face that can last anywhere from a few seconds to two minutes. However there will be pain-free breaks in between episodes, this can continue for up to two hours.
- Atypical trigeminal neuralgia. This will be less painful and intense but it is more widespread. The patient will likely feel constant pain, notably stabbing or burning sensations, along with persistent aches and pains. With atypical trigeminal neuralgia, patients may have more difficulty controlling the symptoms.
What are the causes of Trigeminal Neuralgia?
The trigeminal nerve is a mixed cranial nerve responsible for sensation on the face and it is also responsible for the motor function of the muscles of mastication.
There are many conditions that may cause trigeminal neuralgia, but it is typically caused by a blood vessel exerting pressure on the nerve near the brain stem which causes irritation of the nerve.
An enlarged or lengthened blood vessel most commonly the superior cerebellar artery compressing against the microvasculature of the trigeminal nerve near its connection with the pons. Such compression can injure the nerve’s protective myelin sheath and cause unpredictable and hyperactive functioning of the nerve. This leads to attacks of pain at the slightest stimulation of any area served by the nerve as well as hinders the nerve’s ability to shut off the pain signals after the stimulation ends. This type of injury may rarely be caused by an aneurysm; a tumor; such as meningioma or trauma, such as a car accident.
Short-term peripheral compression is often painless—continuous compression results in local demyelination with no loss of potential axon continuity.
Chronic nerve entrapment results in demyelination primarily, with subsequently progressive axonal degeneration. It is, ” widely accepted that trigeminal neuralgia is associated with demyelination of axons in the Gasserian ganglion.” It has been suggested that this compression may be related to a branch of the superior cerebellar artery that lies on the trigeminal nerve.
Secondary trigeminal neuralgia is caused by pressure on the nerve from a tumor, Multiple Sclerosis due to damage to the spinal trigeminal complex, a cyst, cerebellopontine angle tumor, or another expanding lesion, facial injury, or another medical condition that damages the myelin sheaths.
When there is no apparent structural cause it is called idiopathic.
Postherpetic neuralgia, which occurs after shingles might cause similar symptoms if the trigeminal nerve is damaged. Some patients may experience trigeminal neuralgia due to lesions in the brain or other abnormalities. In other cases, stroke, surgical injuries, or facial trauma may be responsible for trigeminal neuralgia.
What is the Trigeminal nerve?
There are XII cranial nerves in the body, and all of them originate in the brain. They come in pairs for both sides and connect different body areas and organs to the brain.
The Trigeminal Nerve is also known as the fifth cranial nerve which is a cranial nerve responsible for sensation in the face and motor functions such as biting and chewing. Its name “trigeminal” means tri-, or three, and – geminus, or twin so each of the two nerves arrives from the pons.
The trigeminal nerve is a mixed nerve that has both sensory and motor function
Sensory information includes sensations about touch, taste, smells, sights, and sounds.
Motor information includes the signals that affect the movement or activity of muscles and glands.
Nerves that send sensory information have sensory functions. Those which send motor information have motor functions. Although some nerves have only sensory or motor functions, others can have both.
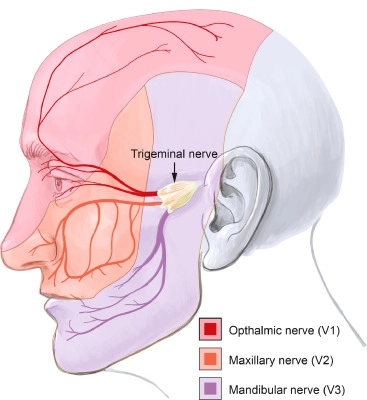
three major branches: the ophthalmic nerve, the maxillary nerve, and the mandibular nerve.
The ophthalmic and maxillary nerves are pure sensory nerves, whereas the mandibular nerve supplies motor as well as sensory or cutaneous functions.
More complex of this nerve is that autonomic nerve fibers, as well as special sensory fibers (taste), are contained within it.
The motor division of the trigeminal nerve arrives from the basal plate of the embryonic pons, and the sensory division originates in the cranial neural crest. Sensory information is processed by parallel pathways in the central nervous system which is coming from the face and body.
Anatomy of Trigeminal Nerve:
The three major branches of the trigeminal nerve—the ophthalmic nerve, the maxillary nerve, and the mandibular nerve —merge on the trigeminal ganglion. A ganglion is a collection of nerves outside the nervous system, which is located within Meckel’s cave and contains the cell bodies of incoming sensory-nerve fibers at the side of the head near the temple, in front of the ear. The trigeminal ganglion is similar to the dorsal root ganglia of the spinal cord, which contain the cell bodies of incoming sensory fibers from the rest of the body.
From the trigeminal ganglion, a single, large sensory root enters the brainstem at the level of the pons. Immediately adjoining to the sensory root, a smaller motor root enters from the pons at the same level. Motor fibers pass without synapsing through the trigeminal ganglion on their way to peripheral muscles, but their cell bodies are located in the nucleus of the fifth nerve, deep within the pons.
Trigeminal Nuclei
All sensations from the face, both touch, position and pain, and temperature, are sent to the trigeminal nucleus. except for parts of the mouth, ear and meninges are carried by VII cranial nerve.
The trigeminal nucleus extends through the brainstem, from the midbrain to the medulla, and continues into the cervical cord where it merges with the dorsal horn cells of the spinal cord. The nucleus is divided into three parts. From caudal to rostral ascending from the medulla to the midbrain they are the spinal trigeminal nuclei, the principal sensory and mesencephalic nuclei. These parts of the trigeminal nucleus receive different types of sensory information, the spinal trigeminal nucleus receives pain-temperature fibers, and the principal sensory nucleus receives touch-position fibers and proprioceptor and mechanoreceptor fibers from the jaws and teeth received by the mesencephalic nucleus.
Spinal trigeminal Nuclei
The spinal trigeminal nucleus consists of pain and temperature sensory maps of the face and mouth. From the spinal trigeminal nucleus, secondary fibers cross the midline and ascend in the trigeminothalamic tract contralaterally to the thalamus. Pain-temperature fibers are sent to multiple thalamic nuclei. The central processing of pain-temperature information is different from the processing of touch-position information.
Principal nucleus
The principal nucleus represents touch, pressure sensation from the face. It is situated in the pons, near the entry of the fifth nerve. Fibers carrying touch-position information of the face and mouth from cranial nerves V, VII, IX, and X are sent to this nucleus when they enter the brainstem. From the principal nucleus, secondary fibers cross the midline and ascend in the ventral trigeminothalamic tract to the contralateral thalamus. Some sensory information from the teeth and jaws is sent from the principal nucleus to the ipsilateral thalamus via the small dorsal trigeminal tract.
Mesencephalic nucleus
The mesencephalic nucleus is not a true nucleus, it is a sensory ganglion enclosed in the brainstem and the sole. Two types of sensory fibers are present in the mesencephalic nucleus: proprioceptor fibers from the jaw and mechanoreceptor fibers from the teeth.
Main branches of Trigeminal Nerve:
The Trigeminal nerve has three branches that perform distinct functions:
- Ophthalmic: This branch sends nerve impulses from the upper part of the face and scalp to the brain. Ophthalmic refers to the eye. The ophthalmic nerve is connected to the eyes, upper eyelids, and forehead.
- Maxillary: This nerve branch is responsible for sensations in the middle part of the face. Maxillary refers to the upper jaw. The maxillary nerves extend to cheeks, nose, lower eyelids and upper lip, and gums.
- Mandibular: The mandibular branch aids sensation in the lower part of your faces, such as the jaws, lower lip, and gum. These nerves also have a motor function. which helps to bite, chew and swallow.
What is the course of Trigeminal Nerve?
All 3- ophthalmic, maxillary, & mandibular branches leave the skull through three separate foramina: opthalmic from the superior orbital fissure, maxillary from the foramen rotundum, and mandibular from the foramen ovale.
The ophthalmic nerve conveys sensory information from the forehead, scalp, the upper eyelid, the conjunctiva and cornea of the eye, the nose, the nasal mucosa, the frontal sinuses, & parts of the meninges (the dura and blood vessels).
The maxillary nerve transfers sensory information from the cheek, lower eyelid, the nares, & upper lip, the teeth and gums, the nasal mucosa, the palate and roof of the pharynx, the maxillary, ethmoid and sphenoid sinuses, & parts of the meninges.
The mandibular nerve carries sensory information from the jaw, lower lip, lower teeth, and gums & the chin except for the angle of the jaw, which is supplied by cervical branches, parts of the external ear & parts of the meninges. The mandibular nerve carries touch-position and pain-temperature sensations from the mouth. Although it does not carry taste sensation which is carried by chorda tympani, one of its branches—the lingual nerve—carries sensation from the tongue.
The peripheral processes of the mesencephalic nucleus of Vth neurons run in the motor root of the trigeminal nerve & terminate in the muscle spindles in the muscles of mastication. They work as proprioceptive fibers which convey information regarding the location of the masticatory muscles.
The central processes of mesencephalic Vth neurons synapse in the motor nucleus.
What are the functions of the Trigeminal Nerve?
The main function of the trigeminal nerve is transmitting sensations to the skin, sinuses, and mucous membranes in the face. The nerve transmits pain, temperature & touch to the brain.
The sensory function of the trigeminal nerve is to supply proprioceptive, tactile & nociceptive sensations to the face and mouth.
Dermatome distribution of the trigeminal nerve is the area of skin supply of the three sensory branches of the trigeminal nerve that has keen borders with relatively little overlap.
The motor component of the mandibular division of the trigeminal nerve controls the movement of eight muscles, including the four muscles of mastication: the temporal muscle, the masseter, and the medial and lateral pterygoids. Another four muscles are the tensor tympani, the tensor veli palatini, the mylohyoid & the anterior belly of the digastric.
With the exception of the tensor tympani, all these muscles are involved in chewing, biting, and swallowing and all have bilateral cortical representation.
How to test Trigeminal Nerve?
The Trigeminal nerve is responsible for many sensations that are felt in different parts of the face. There are many ways to test the nerve
Common methods include:
Cotton swab test. One or both sides of the face are touched with a cotton swab. The patient will then be asked whether they felt anything, and if so, where they felt it.
A doctor may also check corneal reflex by lightly touching the cornea of the eye with a cotton swab to test the ophthalmic division. If the patient doesn’t blink, the ophthalmic division of their trigeminal nerve may be damaged.
Clenching test. A doctor will ask patients to clench their teeth or try to open their jaws against the resistance. They’ll check the tone of muscle and movement for any signs of trigeminal nerve damage.
How to protect the Trigeminal nerve?
Healthy lifestyle changes can lead to a healthy nervous system.
- Intake of a nutritious diet and plenty of water to prevent dehydration.
- Be physically active most days of the week with regular exercises.
- Find healthy ways to manage stress like meditation, mindfulness and relaxation technique, yoga, or gardening.
- Improve your sleep habits.
- Manage comorbid conditions like diabetes and high blood pressure that can affect nerve function.
- Quit smoking or any other addiction.
What is the diagnostic procedure for Trigeminal Neuralgia?
Trigeminal neuralgia can be very difficult to diagnose because there are no specific diagnostic tests and symptoms are very similar to other facial pain disorders. That’s why it is important to seek medical care when feeling unusual, sharp pain around the jaw, lips, nose, forehead, eyes, and scalp, especially if you have not had dental or other facial surgery recently.
Reflex tests also can help doctors determine if a patient’s symptoms are caused by a compressed nerve or another condition.
Trigeminal neuralgia is usually diagnosed based on the patient’s description of the symptoms, detailed patient history, and clinical evaluation. There are no specific diagnostic tests for Trigeminal neuralgia, so doctors must rely on symptoms and history.
Physicians base their diagnosis on the type of pain (sudden, intense, quick, and shock-like), the location of the pain, and the things that trigger the pain. Physical and neurological examinations may also be done so the doctor can better understand where the pain is located.
while also performing a physical exam of your head and neck area, including your ears, mouth, teeth, and temporomandibular joint.
They will likely make their diagnosis based on a few factors: The specific type of pain you’re feeling.
The exact point on your face where you feel pain.
The activities or actions which trigger a painful episode.
Neuroimaging studies like Magnetic Resonance Imaging (MRI)of the Brain or Head CT-scan can help in identifying causes like multiple sclerosis or cerebellopontine angle tumor, which can cause secondary Trigeminal Neuralgia.
MRI or high-resolution MRI can help in identifying vascular compression as the cause of classic Trigeminal Neuralgia. A high-resolution MRI can reveal if there is compression caused by a blood vessel. This can give a detailed picture of the brain and the blood vessels. These are called FIESTA sequences in some MR machines.
In these MRI machines, each section is taken in a coronal plane as thin as 1 mm, without any skips between the images. This is how the imaging of the entire course of the trigeminal nerve can be obtained, and the offending vessel causing compression is identified.
Differential Diagnosis of Trigeminal Neuralgia:
There are some conditions that can mimic trigeminal neuralgia are:
- Temporo-mandibular Joint syndrome
- Dental pain
- Post-herpetic neuralgia
- Temporal tendinitis
- Ernest syndrome (injury of the stylomandibular ligament
- Occipital neuralgia
- Cluster headaches or migraines
- Giant cell arteritis
- Glossopharyngeal neuralgia
- Sinus infection
- Ear infection
What is the treatment plan for Trigeminal Neuralgia?
The treatment options for patients with trigeminal neuralgia depend on a variety of factors, including general health, age, disease severity, and the underlying cause. The decision should be taken after a thorough discussion of the process with the patient and other doctors involved in the care of the patient.
As with many conditions without clear physical or laboratory tests, Trigeminal Neuralgia is sometimes misdiagnosed. Trigeminal Neuralgia patients will sometimes look for the help of numerous clinicians before a firm diagnosis is made.
There is evidence that the longer a patient suffers from Trigeminal neuralgia the harder it may be to reverse the neural pathways associated with the pain.
Trigeminal neuralgia treatment generally starts with medications, and some patients don’t need any additional treatment. nevertheless, over time, some patients with trigeminal neuralgia may stop responding to medications, or they may experience unpleasant side effects. For those patients, injections, or surgery provide other treatment options.
If your condition is due to a secondary cause, such as multiple sclerosis, the doctor will treat the underlying condition.
The painful attacks of trigeminal neuralgia can sometimes be brought on, or worsened by certain triggers, so it may help to avoid these triggers if possible.
Avoid hot, cold, or spicy food or drink if these seems to trigger your pain. Using a straw to drink warm or cold drinks may also help prevent the liquid from coming into contact with painful areas of the patient’s mouth. It is important to eat nourishing meals, so eating mushy foods or liquidizing your meals if you’re having difficulty chewing.
Medical treatment for Trigeminal Neuralgia:
To treat trigeminal neuralgia, doctors usually will prescribe medications to lessen or block the pain signals sent to your brain.
Anticonvulsant medications
Carbamazepine is the first-line treatment of anticonvulsant drugs; second-line medications include baclofen, phenytoin, lamotrigine, oxcarbazepine, and topiramate, gabapentin, and pregabalin. clonazepam and lidocaine are also may be effective.
carbamazepine controls pain for most people. When a patient has no relief from this medication, there is doubt whether TN is present. Nevertheless, the effectiveness of carbamazepine decreases over time. Possible side effects include dizziness, double vision, drowsiness, and nausea.
Gabapentin, an anticonvulsant drug most commonly used to treat epilepsy or migraines, can also treat TN. Side effects of these drugs are minor and include dizziness and/or drowsiness which go away on their own.
Oxcarbazepine is a new medication, which has been used more recently as the first line of treatment. It is structurally related to carbamazepine and may be preferred because it generally has fewer side effects. side effects include dizziness and double vision.
Antidepressant medications
Drugs such as amitriptyline or nortriptyline have shown good efficacy in treating trigeminal neuralgia, especially if combined with an anticonvulsant drug such as pregabalin. duloxetine can also be given in some cases of neuropathic pain, especially in patients with major depressive disorder as it is an antidepressant. However, by no means it should be considered first-line therapy and should only be tried by specialist advice.
opioids
There is controversy around opiate use such as morphine and oxycodone for the treatment of TN, with varying evidence on their effectiveness for neuropathic pain. Generally, opioids are ineffective against Trigeminal neuralgia and thus should not be prescribed.
Antispasmodic medications
Muscle-relaxing drugs such as baclofen, Gablofen, and Ozobax may be used alone or in combination with carbamazepine. Side effects can be confusion, nausea, and drowsiness.
Botox injections
Studies have shown that onabotulinumtoxinA injections may reduce pain from trigeminal neuralgia in patients who are ineffective with other medications. Nevertheless, more research should be done on its usage in this condition.
Trigeminal Nerve Blocks
Nerve blocks are injections ( steroid medication or another agent) made at various parts of the nerve to decrease pain. They may provide temporary pain relief for patients with trigeminal neuralgia. Multiple injections are needed to achieve the desired effects and relief which may have different durations for different people.
There are some drawbacks to these medications, other than side effects. Some patients might need relatively high doses to alleviate the pain and the side effects can become more noticeable at higher doses.
Anticonvulsant medications may lose their effectiveness over time. and some patients may need a higher dose to reduce the pain or a second anticonvulsant, which can lead to adverse drug reactions. Many of these drugs have a toxic effect on some patients, particularly patients with a history of bone marrow suppression and liver and kidney toxicity. These patients should have their blood monitored to ensure their safety.
surgical treatment for Trigeminal Neuralgia:
If medication does not help to control trigeminal neuralgia pain despite the increased dosage, or if the side effects are intolerable, there are several surgical procedures to consider. It helps to learn about these options before you are in urgent need of relief so the patient and doctor have time to evaluate them. The patient’s overall health, pain level, age, and availability of the procedure are all factors on which the decision of the type of surgery depends. Most people with trigeminal neuralgia are candidates for any of the surgical treatment options — a doctor can help to decide which ones and in what order you should consider them.
The surgery for trigeminal neuralgia is very precise and delicate since the involved area is very small. Experienced neurosurgeons who see and treat a large number of people with trigeminal neuralgia are good for this surgery.
Microvascular Decompression Surgery
Microvascular decompression surgery is regarded as the most long-lasting treatment for trigeminal neuralgia caused by blood vessel compression, and it helps about 80% of people with this diagnosis. This is suitable for patients in good health who can tolerate surgery and general anaesthesia, and who can accommodate a recovery period of four to six weeks.
Microvascular decompression surgery aims to separate the blood vessel from the trigeminal nerve by placing a cushion made of Teflon between them. The surgeon made an incision behind the ear and removes a small piece of the skull to gain access to the trigeminal nerve and surrounding blood vessels. Then, the surgeon places a cushion around the blood vessel so it does not compresses or rubs against the nerve. The surgery takes two to three hours, and patients can expect to spend a couple of days in the hospital for observation and recovery. The pain relief from Microvascular decompression is quick but not immediate.
The risks of microvascular decompression include cerebral spinal fluid leak, facial numbness, and hearing loss that may persist in some cases. In rare cases, infections, bleeding, seizures, and paralysis can occur.
In some patients treated with microvascular decompression surgeries, pain may return, possibly due to the blood vessels growing back. If this happens, the doctor will help you choose other options. But this procedure is rarely repeated.
Rhizotomy
There are many kinds of rhizotomies for trigeminal neuralgia, which are all performed under general anaesthesia in the operating room. The surgeon inserts a long needle through the cheek and uses an electrical current or chemical glycerin or glycerol to suppress the pain fibers of the trigeminal nerve. Generally first time the chemical approach is typically recommended. Those patients who have the procedure repeated often benefit from both the chemical and the heat treatment in the same session.
The procedure takes about 30 minutes and most patients go home with less to no pain. Out of the surgical options, rhizotomy offers the most immediate relief from trigeminal neuralgia pain. The patient may experience some swelling or bruising on the cheek. The doctor will prescribe pain medications and, if necessary, give a plan to discontinue medications gradually.
This surgery provides pain relief to most patients with trigeminal neuralgia, but it’s a temporary solution that usually lasts one to three years until the nerve regrows.
It is a recommended surgical treatment for patients with trigeminal neuralgia resulting from multiple sclerosis because it is minimally invasive and can be safely repeated since the pain is more likely to come back due to the progression of Multiple sclerosis.
Stereotactic Radiosurgery
Stereotactic radiosurgery is also known as Gamma Knife treatment, is another surgical procedure that can be used to treat trigeminal neuralgia. It includes a very precise and concentrated beam of radiation that is aimed at the trigeminal nerve to relieve the pain. For a detailed image of the head, surgeons use MRI and CT scans to locate the trigeminal nerve. Then, they work with radiation oncologists and physicists to deliver the radiation treatment, it takes about 45 minutes for this procedure.
It is painless and is performed without anaesthesia therefore around 70% of patients experience significant pain relief within weeks of undergoing stereotactic radiosurgery for trigeminal neuralgia. The relief may last for some years, but in some cases, the nerve may recover from radiation and resume transmitting pain.
Side effects are minimal but sometimes fatigue and facial numbness can occur, so the recovery time is brief. It is not recommended more than two times for trigeminal neuralgia treatment because of the high dose of radiation delivered near the brain.
Glycerol injection
In this procedure, the doctor inserts a needle through the face and into an opening in the base of the skull. the doctor guides the needle into the trigeminal cistern which is a small sac of spinal fluid that surrounds the trigeminal nerve ganglion where the trigeminal nerve divides into branches. Then, the doctor injects a small amount of sterile glycerol, which damages the trigeminal nerve and blocks pain signals.
This procedure often relieves pain. However, some patients have a later recurrence of pain, and many experiences facial numbness or tingling.
Balloon compression
In this surgery, the doctor inserts a hollow needle through the patient’s face and guides it to a part of the Trigeminal nerve that goes through the base of the skull. Then, the doctor threads a thin and flexible tube with a balloon on the end through the needle.
then the doctor inflates the balloon with pressure to damage the trigeminal nerve and block pain signals.
Balloon compression successfully controls pain in most people. Most patients undergoing this surgery experience at least some temporary facial numbness.
Percutaneous balloon compression uses a needle that is passed through the cheek to the trigeminal nerve. The neurosurgeon places a balloon through the catheter. The nerve fibers which produce pain balloon should inflate there so the balloon compresses the nerve and blocks pain.
Radiofrequency thermal lesioning
This procedure selectively breaks nerve fibers associated with pain. With anaesthesia surgeon inserts a hollow needle through the face and guides it to a part of the Trigeminal nerve that goes through an opening at the base of the skull.
Once the needle is positioned, the surgeon will briefly wake you from sedation. the surgeon inserts an electrode through the needle and sends a mild electrical current through the tip of the electrode. The patient will be asked to indicate when and where they feel tingling.
Neuromodulation
For patients with trigeminal neuralgia another surgical procedure can be done that includes the placement of one or more electrodes in the soft tissue near the nerves, under the skull on the covering of the brain, and sometimes deeper into the brain, to deliver electrical stimulation to the part of the brain responsible for the sensation of the face. In peripheral nerve stimulation, the electrodes are placed under the skin on branches of the trigeminal nerve. For motor cortex stimulation, the area which innervates the face is stimulated. In deep brain stimulation areas that affect sensation pathways to the face may be stimulated.
Peripheral Neurectomy
The Neurectomy can be performed on peripheral branches of the nerve like the supraorbital, infraorbital, lingual, and alveolar nerves. This can be accomplished by incision, alcohol injection, cryotherapy, or radiofrequency lesioning. Peripheral neurectomy can be safe in elderly patients in rural areas, where neurosurgical facilities are not readily available. Nevertheless, the evidence regarding these peripheral techniques for trigeminal neuralgia is inconclusive.
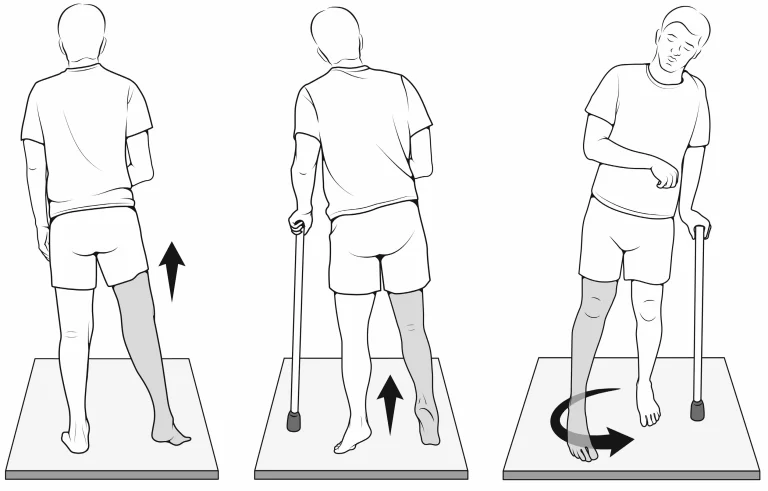
Physiotherapy treatment for Trigeminal Neuralgia:
Physiotherapy treatment promotes general well-being and helps to reduce pain by the use of different techniques. The physiotherapy treatment of trigeminal neuralgia focuses on the patient’s goals and needs.
Transcutaneous Electrical Nerve Stimulation (TENS) is the most effective and most often used technique over the path of affected nerve 5 days a week for 4 weeks.
LASER therapy
Interferential Therapy (IFT)
A hot moist pack was applied to the neck and trapezius muscle for 10 minutes, To reduce muscle spasms
Ultrasound
Physiotherapy Management will also aim at reducing pain and improving the ability to carry on with the activities of daily living
Acupuncture to relieve facial pain and pressure
Isometric neck exercises
Stress management
Relaxation techniques such as deep breathing exercises
Cardiovascular exercises to improve general health and fitness levels
self-massage education
use a scarf to avoid exposure to the cold environment on the affected side of the face
Functional Activities for problems associated with activities of daily living
Avoid the use of cold water for drinking and washing your face
Patient’s education on diet and pain management
Complementary Management for Trigeminal Neuralgia:
people with TN have been using some useful complementary approaches along with the medical treatment to medical management usually used to relieve pain and improve their health. These techniques include:
- Yoga.
- Meditation.
- Creative visualization.
- Acupuncture.
- Chiropractic.
- Aromatherapy.
- Low-impact exercise.
- Supportive counselling or therapy.
- Biofeedback.
- Vitamin therapy.
What is the prognosis of Trigeminal Neuralgia?
Patients should follow up with their primary care providers and specialist doctors regularly to maintain their treatment. Typically, surgical patients are asked to return to the clinic every few months in the year following the surgery. During these visits, they assess the patient’s recovery from surgery.
Routinely following up with a doctor ensures that the treatment is correct and effective. Patients who undergo any form of neurosurgery will also follow up with a device representative who will adjust the device settings and parameters as needed alongside their doctors.






5 Comments