Ulnar Artery
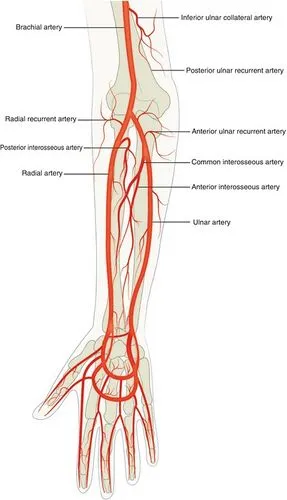
The ulnar artery is one of the major blood vessels in the forearm and hand. It originates from the brachial artery in the upper arm, coursing along the medial aspect of the forearm and running parallel to the ulnar bone.
Table of Contents
Introduction
The radial and ulnar arteries are in charge of providing the blood supply to the hand and forearm. The ulnar artery begins in the cubital fossa, travels through the forearm’s medial (ulnar) side, and terminates as the superficial palmar arch in the hand’s medial region.
The circulatory supply to the hand and upper extremities includes the ulnar artery. With the brachialis muscle at its deep surface, it emerges from the brachial artery as its bigger terminal branch at the level of the cubital fossa. It then travels obliquely and medially (ulnarly) past the flexor digitorum superficialis, palmaris longus, pronator teres, and flexor carpi radialis of the proximal forearm before passing deeply beneath the median nerve.
The flexor digitorum profundus muscle is located posterior to the ulnar artery at the same time. The ulnar artery passes via the flexor carpi ulnaris muscle in the forearm and then continues radially to the ulnar nerve. The ulnar artery is located in the distal forearm and wrist, between the flexor carpi ulnaris tendon (ulnar) and the flexor digitorum superficialis (radially) tendons.
The ulnar artery enters the hand through Guyon’s canal superficial to the flexor retinaculum. It ends with two branches: one deep branch that contributes to the deep palmar arch, and the other superficial, which produces the superficial palmar arch.
It delivers blood that is rich in oxygen to your hands, fingers, wrists, and forearms. Hammering and other repetitive wrist motions can increase the chance of developing ulnar artery thrombosis.
What is the ulnar artery?
A blood vessel in your arm is called the ulnar artery. It gives your hands, wrists, and forearms blood that is high in oxygen.
Relative to the brachial artery, the ulnar artery is one of them. The radial artery is the other branch. The ulnar artery is closest to your pinky on the outside of your forearm. The radial artery is nearest your thumb on the inside of your forearm.
Anatomy:
The larger brachial artery located in the upper arm divides into two branches, which travel down through the forearm. Both the radial and ulnar arteries have these two branches. The ulnar artery forms several structures in the hand, such as:
- The anterior and posterior ulnar recurrent arteries
- Common interosseous artery
- Palmar carpal arch
- Superficial palmar arch
- Dorsal carpal branch
These smaller branches form structures within the hand. Some structures within the hand that receive blood supply from the ulnar artery are the arches and grooves of the palm, along with muscles that flex and rotate the hand and fingers. The axial artery serves as the source of the ulnar and radial arteries during pregnancy instead of the undeveloped brachial artery.
The radial and ulnar arteries are located superficially on the forearm, which means that skin covers them. As a result, these structures are frequently seen in the unaided eye, particularly in those with thin skin or big arteries.
Course and origin
Arm
The subclavian artery is the third branch of the aortic arch on the left and a branch of the brachiocephalic trunk on the right. After going under the clavicle, the artery crosses the lateral boundary of the first rib and is referred to as the axillary artery. The medial, lateral, and posterior cords of the brachial plexus are connected to the axillary artery.
The axillary artery changes its name to the brachial artery as it crosses the inferior border of the teres major. The brachial artery descends the arm, passing deep to the bicipital aponeurosis before splitting to form the ulnar and radial arteries at the elbow (first medial to the medial nerve, then lateral at the elbow). Not often, the ulnar artery split off from the axillary artery.
The radial and ulnar arteries descend the forearm on opposite sides. Numerous muscles, such as the flexor digitorum superficialis, pronator teres, and flexor carpi radialis, surround the ulnar artery along its upper course. It rests above the flexor digitorum profundus and brachialis. The median nerve, which runs between the two pronator teres heads, and the ulnar artery are separated by the ulnar head of the pronator teres.
The ulnar artery provides perforating branches to the muscles on the ulnar side of the forearm and is situated mostly between the flexor digitorum superficialis and flexor carpi ulnaris. At the wrist, the radial artery arises lateral to the median nerve, situated beneath the brachioradialis.
Elbow
By passing anteriorly and posteriorly via the medial epicondyle, respectively, the superior and inferior ulnar collaterals, also known as the anterior and posterior ulnar recurrent arteries, create a network of collateral circulation surrounding the elbow joint from the brachial artery.
When the elbow is flexed or vascular disease restricts blood flow through the main arteries (brachial, ulnar, and radial), this network keeps the elbow perfused. Not every patient has this vast vascular network, and it might be an adaptation that develops after vascular illness in the leg.
Forearm
The common interosseus artery, which divides to form the anterior and posterior interosseous arteries, is derived from the ulnar artery next. These extend both sides of the interosseus membrane, which joins the two forearm bones, down the forearm. The deep muscles of the forearm’s flexor compartment are supplied by the anterior interosseus, whereas the posterior interosseous artery provides the extensor muscles.
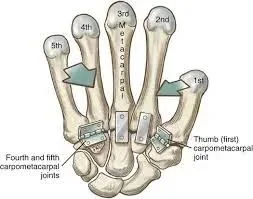
Hand
The ulnar artery then continues to descend the ulnar side of the forearm, close to the ulnar nerve. It is not a component of the carpal tunnel because it just goes briefly through to the transverse carpal ligament. The artery travels lateral to the nerve in its tunnel, also called Guyon’s canal.
Guyon’s canal has a floor formed by the flexor retinaculum and hypothenar muscles, and a roof formed by the superficial palmar carpal ligament. The tunnel is bound medially by the pisiform, laterally by the hamate, and to the floor by the pisohamate ligament. The distal end of the canal is normally restricted by the aponeurotic arch of the hypothenar muscles, measuring around 4 cm in length.
The superficial palmar arch is the primary blood supply to the fingers and is the direct continuation of the ulnar artery once it enters the hand. It is an arch of arteries, completed on the radial side by the little palmar branch of the radial artery. It is only slightly deeper than the thick palmar aponeurosis and lies superficially to all of the intrinsic hand muscles. The bases of the proximal phalanges are reached by three common digital arteries that emerge from this arch and go between the second and fourth metacarpals. At this point, they divide to create the appropriate digital arteries, which supply the fingers on either side.
The deep palmar arch is the source of the radial two common digital arteries, which are the radial artery’s direct continuation. The radial artery forms the deep palmar arch in the hand by running posteriorly between the two heads of the first dorsal interosseus. On the ulnar side, the arch is completed by a deep branch from the ulnar artery. This blood supply, which is especially sensitive because of the paucity of blood vessels in the fingers, can be severely compromised by trauma.
Supplied Structures:
The ulnar artery supplies blood to the ulna, radius, interosseous membrane, and elbow joint. It supplies the flexor digitorum superficialis, flexor carpi ulnaris, flexor digitorum profundus, and pronator teres muscles, which are located on the medial portion of the forearm. Additionally, it provides cutaneous supply to the area surrounding the hypothenar eminence, the medial aspect of the wrist, and the medial aspect of the forearm.
Branches:
The following are the ulnar artery’s principal branches, ordered from proximal to distal:
Anterior ulnar recurrent artery: The proximal branch of the ulnar artery that travels superiorly and anteriorly to the medial humeral epicondyle is known as the anterior ulnar recurrent artery.
Posterior ulnar recurrent artery: The posterior ulnar recurrent artery is a further proximal branch of the ulnar artery that arises from the anterior ulnar recurrent artery. It climbs behind and above the medial epicondyle. Together with the inferior and superior ulnar collateral arterial branches of the brachial artery, the anterior and posterior ulnar recurrent arteries form vascular anastomoses around the elbow.
Common interosseous artery: Anterior and posterior interosseous arteries split from the common interosseous artery, which is a small branch of the ulnar artery. The muscles of the deep, volar compartment of the forearm are supplied by the anterior interosseous artery, which descends along the anterior portion of the interosseous membrane. Many of the dorsal compartment’s extensor muscles are supplied by the posterior interosseous artery, which passes posteriorly to the interosseous membrane.
Palmar carpal branch: The palmar carpal branches of the radial and ulnar arteries combine to form the palmar carpal arch, which is situated on the palmar face of the carpals and supplies the carpal bones and joints with blood.
Dorsal carpal branch: Together with the dorsal carpal branch of the radial artery, the dorsal carpal branch of the ulnar artery supplies blood to the dorsal carpal arch.
Deep palmar branch: Through Guyon’s canal, which is located anterior to the flexor retinaculum, the ulnar artery enters the hand. The ulnar artery’s deep palmar branch contributes to the hand’s deep palmar arch, which is located deep within the flexor tendons, as well as the hypothenar muscles.
Superficial palmar arch: The superficial palmar arch, a crucial vascular structure in the hand, is formed by the ulnar artery as it enters the palm. The superficial palmar arch is radially curved, situated superficially to the flexor tendons and deep to the palmar aponeurosis. The superficial palmar arch gives rise to common digital arteries, which carry blood to the ulnar aspect of the index finger and the ulnar three digits.
Anatomical Variations
Certain individuals may occasionally have anatomical variations of the ulnar artery.
The ulnar artery’s second segment: Possession of a second segment of the brachial artery, which subsequently merges to produce a second segment of the ulnar artery, is one variation that is occasionally observed. Differentiation at the level of the brachial artery is less common in the general population, but these differences within the ulnar artery are rather widespread.
When the ulnar artery starts earlier than in other people, some medical professionals find it difficult to tell the difference between the ulnar artery and the superficial brachial artery. Due to the confusion between the ulnar artery and other vascular structures, these variations can cause difficulties in placing intravenous ports, administering medications intravenously, drawing blood from the ulnar artery, and other issues related to venipuncture.
These people may have anatomical differences due to residual embryological arteries or mild underdevelopment of the forearm’s vascular systems.
Superficial ulnar artery: In some individuals, both the radial and ulnar arteries appear more superficial than is typical. This results from the forearm’s components not developing fully, which usually causes the radial artery to enlarge. In these kinds of circumstances, the radial artery provides greater forearm and hand muscle supply than the normal-sized ulnar artery would.
Once more, a more superficial ulnar artery may be misdiagnosed as extraneous structures, venous inflammation, or other inflammatory disorders by certain diagnostic techniques. For diagnosis and proper treatment, it is crucial to recognize anatomical features and any potential alterations.
Ulnar artery connected to the radial artery: This is an extremely uncommon occurrence that occurs when both arteries are thinner than normal. As a result, the forearm develops an aberrant branching pattern, which makes it more challenging to interpret imaging data, finish diagnostic procedures, and locate damaged artery structures in the forearm.
Function
The ulnar artery’s primary purpose is to carry oxygen-rich blood to the hand and forearm muscles. The ulnar artery, ulnar vein, and ulnar nerve are not the same thing; they serve different purposes.
The ulnar artery supplies oxygenated blood to the smaller arteries in the hand and forearm in addition to supplying nutrition to the forearm muscles. The digital arteries, which provide blood to each finger and the thumb, are among these smaller arteries.
The index finger receives an extra blood supply. One side of the index finger is supplied with blood by the ulnar artery, and the other side is supplied with blood by the radial artery. The blood flow to the index finger is vital since it is one of the most important digits for stabilization and manipulation.
The source of a pulse recording is the ulnar artery. The ulnar pulse normally registers between 60 and 100 beats per minute (bpm).
This can serve as an easy method of taking vital signs, keeping an eye on the basic operation of the heart, and looking for any mild abnormalities in the cardiovascular system. Using the index and middle fingers, feel the artery and count the number of pulses to obtain the ulnar pulse.
Owing to its placement among other forearm structures, the ulnar pulse can occasionally be challenging to find and record. To avoid stiff muscles obscuring the existence of the pulse, it can be simpler to do this if the person relaxes their arm, especially at the wrist.
When abnormalities in the pulse are detected at the level of the ulnar artery, additional comprehensive diagnostic examinations should be performed.
Clinical Significance
The volar wrist is a particularly sensitive area for acute injuries due to the superficial position of the flexor tendons, ulnar and median nerves, and arteries. As previously mentioned, due to their close anatomical association, the ulnar artery frequently sustains damage in conjunction with the ulnar nerve and the flexor carpi ulnaris tendon.
Significant blood loss may result from ulnar artery transection, and pulsating bleeding may occur from the ulnar aspect of the wrist. When the patient is being evaluated and immediate surgical intervention is being planned, bleeding can frequently be controlled by direct pressure and elevation. It is essential to repair concurrent damage to the flexor tendon and nerve injuries. Using an operating microscope makes repairing the ulnar artery in the event of an acute transection very simple.
Trauma: The ulnar artery is especially vulnerable to damage when it is exposed to recurrent blunt trauma, such as when a manual labourer uses the hypothenar aspect of their hand as a hammer. This is because the ulnar artery passes through the Guyon canal at a somewhat exposed superficial site.
Aneurysm/Thrombosis: There is a chance that the ulnar artery will have intimal damage and thrombosis. A ruptured aneurysm could result from the damage extending into the media. Patients may exhibit digital discoloration of the ulnar-sided fingers, paresthesia, coldness, and discomfort. These signs could be associated with distal embolization or vasospasm.
Flaps: Plastic surgeons can plan various flaps to meet a patient’s reconstructive demands if they thoroughly understand the vascular anatomy of the ulnar artery and its perforating branches.
- The flexor carpi ulnaris muscle flap can be turned proximally to fill soft tissue abnormalities of the proximal forearm and elbow, based on the proximal muscular perforators of the ulnar artery. In recent times, the flexor carpi ulnaris muscle flap has been characterized as a distally based muscle flap for soft tissue coverage of the wrist and hand, based on a more distal ulnar artery muscular perforator. These methods preserve the ulnar artery.
- Soft tissue covering of abnormalities involving the dorsal-ulnar hand and palmar-ulnar wrist can be achieved with Ulnar artery perforator-based fasciocutaneous propeller flaps. The ulnar artery is spared with perforator-based pedicled flaps, which is a major benefit.
- The fasciocutaneous free flap, known as the ulnar forearm free flap, is derived from the ulnar artery and its perforating branches to the skin component that is overlaying. It is a thin, flexible, largely hairless flap that is frequently utilized for oncologic restoration of head and neck soft tissue abnormalities that range in size from small to medium. A sufficient length of the ulnar artery and venae comitantes are collected from the flap to facilitate microvascular anastomosis to the recipient site’s arteries. The division of the ulnar artery proximally in the forearm is involved in this flap.
Since the appropriate digital arteries are small end arteries that can suffer from vascular spasm and necrosis if left in a constricted state for an extended period, the use of adrenaline during hand surgeries is discouraged. Because the arteries supplying the fingers and toes are small and delicate, this is also the reason why frostbite affects them first.
Summary
The ulnar artery provides an essential circulatory supply to the hand and upper extremities. It originates at the level of the cubital fossa, where the brachialis muscle is located at the deep surface, as the bigger terminal branch of the brachial artery.
FAQs
The primary blood vessel supplying the medial aspects of the forearm with oxygenated blood is the ulnar artery. It starts from the brachial artery and ends at the superficial palmar arch, where it connects to the radial artery’s superficial branch. On the medial and anterior aspects of the wrist, it is palpable.
Ulnar flow is measured by Allen’s test. This is how the test is conducted: The patient’s fist is simultaneously blocked in the radial and ulnar arteries. The hand seems pale when it is opened. Hand colour should recover after 8–10 seconds after the ulnar artery is released.
It forms a short trunk (2-4 cm) that passes beneath the FCU and superficially to the ulnar nerve. It divides into the descending branch and the ascending branch of the cutaneous system after passing between the extensor carpi ulnaris (ECU) and the FCU.
One of the two major arteries in your forearms is the ulnar artery. It runs along the pinky side of your arm, beginning just below your elbow. It delivers blood that is rich in oxygen to your hands, fingers, wrists, and forearms.
Ischemia of the hand or fingers can infrequently result from injury to one of the major arteries (radial or ulnar) in the forearm. To prevent necrosis, repair should be done right away in cases of ischemia. Nonetheless, the hand and fingers typically show no symptoms of ischemia.
Reference:
- Ulnar artery. (2023, May 25). Kenhub. https://www.kenhub.com/en/library/anatomy/the-ulnar-artery
- Professional, C. C. M. (n.d.). Ulnar Artery. C, Cleveland Clinic. https://my.clevelandclinic.org/health/body/23436-ulnar-artery#overview
- Ferri, B. (2022, November 15). The Anatomy of the Ulnar Artery. Verywell Health. https://www.verywellhealth.com/ulnar-artery-anatomy-4687676#toc-anatomy
- Marques, E., & Bordoni, B. (2023, July 24). Anatomy, Shoulder and Upper Limb, Ulnar Artery. StatPearls: NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK546619/
- Ulnar artery. (2023, May 25). Kenhub. https://www.kenhub.com/en/library/anatomy/the-ulnar-artery



One Comment