Meningitis
Table of Contents
DEFINATION :
- Meningitis is an infectious disease of the central nervous system that causes inflammation of the meningeal membranes, involving all three layers surorunding the brain and spinal cord: dura mater, arachnoid, and pia mater.The arachnoid and pia mater become inflamed and opaque along with the first two layers of the cortex and the spinal cord. Many complications can result from this inflammation such as the increased risk of infarctions leading to blockage of cerebral spinal fluid flow, thromboses in the cortical veins and additional clinical symptoms. Meningitis can present as acute, subacute, or chronic.
- Viral (aseptic) and Bacterial meningitis are the most common forms of acute meningitis. Meningitis is usually a result of fungi, viruses, parasites, bacteria, or a noninfectious inflammation. Viral meningitis is less severe and symptoms can resolve without treatment. However, bacterial meningitis is a more severe form leading to numerous complications and early treatment is key. If diagnosis is delayed, this infectious inflammation can be fatal.
- Meningitis can be difficult to diagnose due to its similar presentations to other infectious disease such as influenza or encephalitis. The risk of developing the disease is highest in the first seven days following onset, and can persist for at least four weeks. Progression is very rapid and is distinguished by purulent CSF. Below is a picture of the meninges which are affected by meningitis.
CHARACTERISTICS OF MENINGITIS:
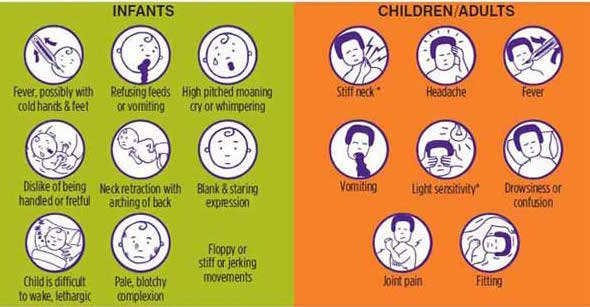
- Headache, fever, vomiting, and rigidity of the neck are the most common symptoms that present with the onset of meningitis.Early symptoms include nausea, drowsiness and confusion. Pain in the posterior thigh or lumbar region may also be noted.Later symptoms can include seizures, photophobia and rapid breathing rate. In addition, a rash on the skin, scanty petechial (red or purple non-blanching macules smaller than 2mm in diameter) or a purpuric (larger than 2mm) appears on approximately 80-90% of individuals with bacterial meningitis.
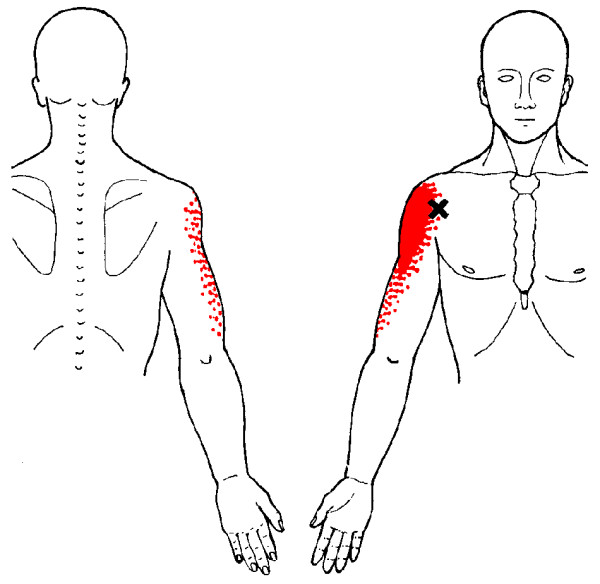
- Meningitis causes inflammation of the meningeal membranes; as a result nerve roots may endure tension as they pass through these inflamed membranes. Passive ROM of the neck into flexion will gradually become painful and limited. Also, neck extension and rotation may be painful as well, however not to the extent of flexion. In severe cases Brudzinki’s sign or Kernig’s may be presented. Brudzinki’s sign is caused by passive neck flexion producing flexion of the hips or knees. Kernig’s sign presents, as restrictive passive extension of the knee while the hip is flexed.In cases when meningitis is not treated immediately (especially bacterial meningitis), the parenchyma within the brain may be involved. As a result individuals may present with lethargy, vomiting, seizures, papilledema, confusion, coma, focal deficits, and cranial nerve palsies.
CAUSES OF MENINGITIS :
- Neonates receive antibodies via placenta for bacteria such as Listeria monocytogenes, Escherichia coli, and group B streptococcus. With age, these antibodies decline resulting in increased susceptibility especially in ages 1 to 2 for meningococcus, pneumococcus, and Haemophilus influenzae type b (Hib). Geriatric and the adult population are more affected by Neisseria meningitis and Streptococcus pneumoniae. Pneumococci infections are especially common in adults who suffer from alcoholism, CSF leaks, chronic otitis, mastoiditis, sinusitis, sickle cell anemia, pneumococcal pneumonia, and asplenia. These organisms are most commonly found in the upper respiratory tract in the mucosal layers.
- Aseptic meningitis is most commonly a result of a viral infection. Enteroviruses (echovirus and coxsackievirus) and herpes simplex virus are the most common viruses representing 40% of the cases of meningitis in individuals 30-60 years old and 20% of all individuals with meningitis, respectively. Individuals in late adolescence and early adulthood who develop meningitis usually came in contact with the Epstein-Barr virus (EBV). Other causes of viral meningitis include intracranial tumor rupture, mumps, systemic lupus erythematosus, radiopaque agents, lead poisoning, itrathecal drug use, and NSAIDs especially as a result of exposure during surgery.
- Bacterial meningitis is transmitted person to person through droplets of respiratory such as coughing or sneezing or throat secretions from carriers. Usually transmitted through close or prolonged contact. Average incubation is 4 days but can range between 2-10 days.Below are two tables that list causes of bacterial meningitis by age and associated risk factors.
Symptoms of Meningitis :
DIFFERENTIAL DIAGNOSIS :
- Confusion/dementia
- Cervical arthritis (stiff neck)
- Subarachnoid hemorrhage
- Pneumonia
- Otitis media
- Pharyngitis
- Gastroenteritis
- Upper Respiratory Infection
- Retrophyaryngeal Abscess
- Brain/Subdural/Epidural Abscess
- Encephalitis
SYSTEMIC INVOLVEMENT :
NERVOUS:
- Inflammation of subarachnoid space
- Spread of inflammation to parenchyma
- Focal ischemic lesions
- Hydrocephaly
- Impaired consciousness
- Stages include irritability, confusion, drowsiness, stupor, and coma
- Hemiparesis
- Seizures
- Cranial nerve palsy
- Hypothalamic dysfunction in children
VASCULAR:
- Inflammation of small subarachnoid vessels (especially veins)
- Thrombotic obstruction of vessels
- Musculoskeletal
- Opisthotonic posture
- Infectious spread to joints
SENSORY:
- Impaired hearing
- Loss of vision
METABOLIC:
- Dehydration
- Hyponatremia
GASTROINTESTINIAL:
- Vomiting
INTEGUMENTARY:
- Petechial rash of skin (usually associated with bacterial meningitis)
PHYSIOTHERAPY MANAGEMENT :

- According to the American Physical Therapy Association’s Guide to Physical Therapist Practice infectious disorders of the central nervous system fall under the following preferred practice patterns; 5D: Impaired Motor Function and Sensory Integrity Associated with Nonprogressive Disorders of the Central Nervous System- Acquired in Adulthood or Adolescence and 5I: Impaired Arousal, Range of Motion, and Motor Control Associated with Coma, Near Coma, or Vegetative State.
- Typically physical therapy treatment is initiated in the intensive care unit. While initiating a plan of care, it is crucial to keep in mind a patient’s chart information or contraindications to therapy such as intracranial pressure, cerebral perfusion pressure, and other lab values that determine rehabilitation guidelines. Meningitis may present with similar symptoms to brain injuries, neurological complications, immunological deficiency, vascular compromise, and additional secondary impairments.
- Additionally understanding the various stages of consciousness or behavioral changes a patient with secondary complications may go through can guide the approach to treatment. The therapist should create an environment that would ease the patient’s hypersensitivity to sensory input such as light or sound thus creating a structured environment to eliminate behavioral outbursts. Close monitoring of the vital signs will allow the therapist to gage the patient’s receptiveness to therapy. The therapist should be familiar with the Glasgow Coma Scale and monitor the patient’s progression through the levels of consciousness.
- Proper positioning and range of motion exercise should be intiated as soon as safely possible in the acute phase. Proper positioning with pillows and towels will protect the skin integrity and prevention of contractures. Maintaining mobility of the trunk and neck are important to sustain functional mobility. The earlier therapy is initiated with a patient, the chances of secondary impairments are decreased allowing for a better prognosis.
- A primary key component to treating a patient recovering from bacterial meningitis is proper education not only to the patient, but to the family and caregivers as well. Providing the patient and family with education on the disease, stages of the disease, secondary complications, warning signs and resources can encourage the patient and family to become more involved in the treatment. It is very important to educate on the effects from different systemic involvement and how the time line of recovery may vary.







4 Comments