Headaches
Table of Contents
Description
Headache is a very common condition that most people will experience several times in their life. The primary sign of a headache is a pain in the head or face. There are too many types of headaches and tension headaches are the most common. Although most headaches are not dangerous, some headaches can be a sign of a serious illness. A headache is a pain in the head or face that is often felt as throbbing, constant, sharp, or dull. Headaches can vary greatly depending on the type, severity, location, and frequency of the pain.
What are the types of Headaches?
There are more than 150 types of headaches. They fall into 2 main categories: primary and secondary headaches.
1 Primary headaches
Dysfunction or overactivity of the pain-sensing properties of the head causes a primary headache. They are not symptoms or caused by an underlying disease. Some people may have genes that make them more likely to get primary headaches.
Types of primary headaches include:
- Tension-type headaches
- Migraine headaches.
- Cluster headaches.
- New daily persistent headaches (NDPH).
1 Tension-Type Headaches

Tension headaches are typical headaches that frequently cause mild to moderate pain that some define as a tight band around the head. This headache may be healed with over-the-counter ache relievers or antidepressants. Other treatments include lifestyle changes and learning how to respond to stress.
What are the types of tension-type headaches?
Tension headaches into two main types.
Episodic tension-
This type of headache happens less often (fewer than 15 days a month). Your doctor may describe them as “infrequent” if you have one or fewer headaches each month.
Chronic tension –
This type describes when you have more headache days than headache-free days. Chronic tension-type headache occurs at least 15 days per month for more than three consecutive months.
Cause of tension headache
Scientists have not identified a single cause of tension headaches. This type of headache is not hereditary (it runs in families). Some doctors believe that tight head or neck muscles can trigger (cause) a tension headache.
The trigger point of tension headache
A person may be more likely to have tension headaches if they have:
- Eye strain, such namely from staring at a computer screen for a long time.
- Pain in other parts of the head and neck caused by problems reasons temporomandibular disorders.
- Problems sleeping, mainly insomnia.
- Stress related to family, work, or life challenges, namely starting or losing a job or juggling too many commitments.
Symptoms of tension headache
People experience tension headache symptoms in different ways. Some individuals determine this type of headache as supposing that someone (or something) is squeezing both sides of their head completely or a band near their head. A person can have pain that’s:
- Constant (but not throbbing).
- Mild or moderate (not severe).
- On both sides of the head.
- Better after a person takes over-the-counter pain relievers.
Difference between tension headache and migraine
Migraines are another common headache type. Migraines and tension headaches tend to cause various symptoms. A migraine is more likely to cause:
- More severe pain.
- Throbbing or pounding pains.
- Symptoms mainly focused on one side of the head.
- Pain gets worse when a person is near bright lights or loud sounds.
- Nausea or vomiting.
Side effects of medication in tension headache
Headaches:
- Taking pain relievers too frequently may cause a headache (called rebound headaches) when a person stops taking the medicine.
- This effect is similar to withdrawal.
Other side effects:
- Every drug has side effects. Do not take aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs), namely ibuprofen, too frequently.
- Overuse can be the reason for stomach pain, bleeding, or ulcers.
- If a person takes any medication regularly, discuss the risks and benefits with the doctor.
Reduced benefits over time:
- A person’s body may build up a tolerance (get used to) to any medication.
- A person can notice that a medication a person used regularly does not work as well as it once did.
Dependence:
- Some medications may become addictive.
- They can pose more risks than benefits. For that reason, physicians generally suggest against prescribing benzodiazepines and narcotics (namely codeine and oxycodone) to treat tension headaches.
2 Migraine Headaches

A migraine is more than a bad headache. This neurological condition can cause debilitating throbbing pain that can leave you
in for how many days in bed! Movement, light, sound, and other triggers can cause symptoms such as pain, fatigue, nausea, visual disturbances, numbness and tingling, irritability, difficulty speaking, temporary vision loss, and more.
What is an aura?
- An aura is a group of sensory, motor, and speech symptoms that usually act as warning signals of a migraine headache.
- Often misinterpreted as a seizure or stroke, it usually occurs before the headache, but can sometimes occur during or even after it.
- A plow can last from 10 to 60 minutes.
- About 15 to 20 percent of people with migraines have an aura.
Symptoms of aura
Aura symptoms are reversible, meaning that they may be stopped/healed. An aura generates symptoms that can involve:
- Seeing bright flashing dots, sparkles, or lights.
- Blind spots in your vision.
- Numb or tingling skin.
- Speech changes.
- Ringing in your ears (tinnitus).
- Temporary vision loss.
- Seeing wavy or jagged lines.
- Changes in smell or taste.
- A “funny” feeling.
Types of migraine headaches
There are many different types of migraine, and the same type may be given different names.
Migraine with aura (complex migraine):
- Approximately 15-20% of migraine sufferers have aura.
Migraine without aura (common migraine):
- This type of migraine occurs without warning from the aura.
- The symptoms are the same, but this stage does not occur.
Migraine without headache:
Also identified as “silent migraine” or “painless migraine,” this form includes aura symptoms but not the headache that usually follows.
Hemiplegic migraine:
- Provisional paralysis (hemiplegia) or neurological or sensory changes on one side of the body.
- A headache can begin with temporary numbness, extreme weakness on one side of the body, and a tingling sensation.
- Numbness, sensory loss, dizziness, or visual disturbances. A headache can or cannot occur.
Retinal migraine (ocular migraine):
- There may be a temporary, partial, or complete loss of vision in one eye and a dull pain behind the eye that radiates to the rest of the head.
- This vision loss may last from a minute to several months. Retinal migraines should always be reported to your doctor as they can be a sign of a more serious problem.
Chronic Migraines:
- If a migraine occurs at least 15 days a month, it is said to be a chronic migraine.
- Symptoms change frequently, and so does the intensity of pain.
- A person who suffers from chronic migraines may be on headache medication for more than 10-15 days a month, and unfortunately, this can lead to more frequent headaches.
Migraine with brainstem aura
- This is a rare, severe migraine headache that can last more than 72 hours.
- Headache and nausea can be very severe. Certain medications and drug interruptions can trigger this type of migraine.
stage of migraine
In chronological order, there are four stages: prodromal (aura), aura, headache, and posterior curtain. about 30% of people Feel the symptoms before the headache occurs. The phases are:
Prodrome:
- The first stage lasts for hours but can last for days.
- It doesn’t happen every time, so you may or may not experience it. Some know this as the “frontal headache” or “aura” stage.
Aura:
- Aura stages can last up to 60 minutes and as short as 5 minutes.
- Most people do not feel an aura, but some people feel an aura and a headache at the same time.
Headache:
- Headache lasts about 4 to 72 hours.
- The word “pain” is not accurate because it can be mild, but it is commonly described as a constant, throbbing, or feeling like an ice pick is stuck in the head. It usually starts on one side of the head and spreads to the other side.
Postdromal symptoms:
- Inability to concentrate. Depressed. Fatigue. Lack of understanding. Euphoric atmosphere.
Risk factors
It’s challenging to indicate who will obtain migraines and who won’t, but there are risk factors that may make a person more helpless. These risk factors involve:
Genetics: Up to 80 percent of people with migraine headaches have a first-degree relative with the condition.
Gender – Migraine headaches are more common in women than men, especially women aged 15-55. It probably occurs more often in women due to the effects of hormones.
Stress level – If you are under a lot of stress, you may get migraines more often. Stress can trigger migraines. Smoking.
What are the symptoms of migraine?
- The primary sign of a migraine is a headache.
- The pain is sometimes described as throbbing or throbbing. It can start as a dull ache that progresses to a throbbing pain that is mild, moderate, or severe. If your headache is not treated, it will become moderate or severe.
- The pain may turn from one side of the head to the other, or it can affect the front of the head, the back of the head, or feel like it affects the whole head.
- Some people feel pain around the eyes or temples, and sometimes in the face, sinuses, jaw, or neck.
Other symptoms of a migraine headache include:
- Sensitivity to light, noise, and smells.
- Nausea and vomiting, stomach and abdominal pain.
- Loss of appetite.
- Feeling very hot (sweating) or cold (shaking).
- Light skin color (pale).
- Feeling tired.
- Dizziness and blurred vision.
- Sensitive scalp.
- Diarrhea (rare).
- Fever (rare).
- Most migraines last about four hours, although severe migraines can last much longer.
- Each stage of a migraine attack can include different symptoms:
Prodromal symptoms:
- Problems with concentration.
- Irritability and/or depression.
- Difficulty speaking and reading.
- Difficulty sleeping.
- Yawning Nausea.
- Fatigue.
- Sensitivity to light and sound.
- Appetite for food.
- Increased urination.
- Muscle stiffness.
Symptoms of aura:
- Numbness and tingling.
- Visual disturbances.
- You may see the world as if through a kaleidoscope, have blurry spots, or see sparks or lines.
- Temporary loss of vision.
- Weakness on one side of the body.
- Speech changes.
Headache symptoms:
- Neck pain, stiffness.
- Depression, dizziness, and/or anxiety.
- Sensitivity to light, smells, and sound.
- Nasal congestion. Insomnia.
- Nausea and vomiting.
Postdromal symptoms:
- Inability to concentrate.
- Depressed.
- Fatigue.
- Lack of understanding.
- Euphoric atmosphere.
Causes of migraine
- The cause of migraine headaches is complex and not fully understood.
- When you have a headache, it’s because certain nerves in your blood vessels are sending pain signals to your brain.
- In this way, inflammatory substances are released into the nerves and blood vessels of the head.
- It is unclear why your nerves do this.
Migraine trigger points
Migraine attacks may be triggered by too many factors. Typical triggers contain:
Emotional stress
- Emotional stress is one of the most ordinary migraine headaches.
- Certainly during stressful events chemicals in the brain are released to fight the situation (known as the “flight or fight” response).
- Publishing their chemicals can cause migraines.
- Some other feelings, namely anxiety, worry, and tension, can improve muscle tension and extend vessels It can make your migraines more threatening.
Missing meal
- Delaying a meal can also trigger a migraine headache.
- Sensitivity to certain food chemicals and preservatives.
- Specific foods and beverages namely aged cheese, beverages contain alcohol, chocolate, and food additives such as nitrates (found in pepperoni, hot dogs, and lunch meat) and fermented or pickled foods can cause up to 30% of migraines.
Caffeine
- Excessive caffeine consumption or caffeine withdrawal can cause headaches if caffeine levels drop sharply.
- Your blood vessels seem to become more sensitive to caffeine and if you don’t get it you can get a headache.
- Caffeine sometimes physicians suggest to treat acute migraine attacks, but it should not be used frequently.
Daily use of painkillers
- If you use headache medicine too often, it can cause a rebound headache.
- Hormonal changes in females Migraines are more common in ladies at the time of menstruation.
- The sudden drop in estrogen that triggers menstruation can also trigger migraines.
Hormonal differences
- This may also be caused by birth management pills and hormone replacement therapy.
- Migraines tend to be worse between puberty and menopause because teenagers and postmenopausal women don’t usually experience these fluctuations in estrogen.
- If your hormones are a powerful factor in migraines, you can feel more irregular headaches after menopause.
- Hormonal changes do not cause migraines in men.
Light
- Flashing lights, fluorescent lights, TV or computer lights, and sunlight can trigger you.
Other possible triggers include:
- Changing weather conditions, such as storm fronts, changes in air pressure, strong winds, or changes in altitude.
- Being too tired.
- Overload.
- Dieting or drinking enough water.
- Changes in your usual sleep patterns.
- Loud sounds.
- Exposure to smoke, perfumes, or other odors.
- Some medications cause blood vessels to swell.
3 Cluster headache

Cluster headaches cause severe, one-sided pain and occur up to eight times a day, in episodes lasting weeks to months before easing. People aged 20-40 suffer the most. Newer treatments include electrical stimulation.
Cluster headache difference
A cluster headache is a very painful headache, even more so than a migraine. Physicians consider both types of headaches to be primary rather than secondary.
- Primary headache: starting from a reaction of the part of the brain that transmits pain. A primary headache is its health problem, not part of a larger problem.
- Secondary headaches: Start from another disease. These headaches can be caused by several things, including ear infections, nasal congestion, and dehydration. Cluster headaches may disrupt life for weeks or even months at a time. They tend to follow a pattern, often appearing at the same time each day. They can also awaken a person an hour or two after a person goes to bed. These nighttime headaches can feel more severe than daytime ailments.
Why are they called cluster headaches?
- Cluster headaches obtain their name from how they affect a person. For most people, they occur in clusters or groups before temporarily going away.
- Each headache usually lasts 30-45 minutes, although some are shorter and others are longer.
- You can have up to eight of these headaches in 24 hours. And this may occur for weeks or months.
- Then the clusters usually stop for reasons that are not yet understood.
- Headaches go away for months or years before returning. However, some people never get much time.
- They experience chronic (constant) cluster headaches.
- This occurs in about 1 in five people who have cluster headaches.
Why do some people call them suicidal headaches?
- Some people call cluster headaches “suicide headaches.”
- The name came from people who take their own lives when they experience or expect a cluster headache.
- Unfortunately, some people feel that there is no hope for cluster headaches.
- But health care providers can help you with these headaches.
Causes of cluster headache
- Cluster headaches affect 1 in 1,000 people.
- This makes them less common than migraines, although some people have both headaches.
- Cluster headache symptoms usually begin to appear between the ages of 20 and 40.
- Scientists once thought that these headaches were more common in men.
- They now think they affect males and females equally.
- Cluster headaches are also more typical in individuals who smoke and drink alcohol often.
- Many people with cluster headaches also have sleep apnea.
- Experts still don’t know much about cluster headaches, including exactly what causes them.
- Cluster headache is a kind of trigeminal autonomic cephalgia that includes the hypothalamus, the brain structure of the autonomic nervous system, and implicates the 1st branch of the trigeminal nerve.
- Symptoms include severe flank pain, usually around and around the eyes, and tears.
Tiggers points of cluster headaches
If you have cluster headaches, you probably know their triggers. These are things that can cause or otherwise affect a headache.
There are two ways to view a trigger:
- Triggers that begin a new headache cycle (cycle): Most individuals go months or years between cluster headache episodes.
- When the headache starts again, the change often seems to be related to the changing of the seasons.
- (The relationship makes individuals consider they have allergies or a sinus infection.)
- This can occur because there is a suspected link between cluster pains and the hypothalamus.
- This part of the brain contains the “circadian clock”, a built-in schedule that responds to sunlight.
Triggers that affect the headache cycle:
- During headache episodes, the blood vessels in the brain change.
- These differences make a person more sensitive to alcohol and nicotine.
- Small amounts of alcohol can cause headaches.
- Smoking can also make headaches worse or cause headaches.
What are the signs of a cluster headache?
- Cluster headaches usually have very recognizable symptoms.
- Once symptoms start, it usually only takes 5-10 minutes for them to get worse. Common symptoms include a one-sided headache and other symptoms involving the eyes, nose, and skin on the same side of the pain.
Pain from cluster headache
- The pain caused by a cluster headache has some notable features:
- Often described as burning or piercing. Lasted from 15 minutes to 3 hours at a time.
- It usually feels on the same side of the head in the current cycle – rarely it can change in the future.
- Always centered behind one eye, but may spread to the forehead, temple, nose, and gums on the affected side.
- It can make you feel like you can’t sit still and need a boost, unlike the relief that comes with reclining migraines.
Other cluster headache symptoms
Congestion: Your nose may be runny or blocked just on the side of the headache
Eye problems: You may experience drooping eyelids, eye pain, or watery eyes. Your pupil (the black center of the eye) may also appear smaller. These symptoms appear on the same side of the head as the headache.
Facial changes: You may start sweating and your face may turn red from the headache.
4 New daily persistent headache (NDPH)

New daily persistent headache (NDPH) is a rare disorder that occurs unpredictably and for unknown reasons. Patients with NDPH have headaches that do not stop or improve with standard treatments. For some people, headaches can last for years or never go away. There are therapies available, but they are not constantly successful.
What is the new daily constant headache?
- A new daily persistent headache (NDPH) is a rare headache.
- Symptoms of NDPH begin very suddenly and are moderate to severe.
- It is not a dangerous condition, but the symptoms last for months and can seriously interfere with your life and routine activities.
- Most patients with this condition are also challenging to treat.
- NDPH has two main types, primary and secondary.
Primary NDPH: It is called “idiopathic” NDPH, which suggests that experts cannot diagnose properly why it happens.
Secondary NDPH: This is when NDPH occurs secondary to another illness or disease, most often a viral illness.
Who is affected by the new daily constant headache?
- Anyone can get NDPH, however, it is more frequent in women and those who were given the gender of a female at birth.
- It can also happen more often in children and teenagers, especially between the ages of 10 and 18, but it can still happen at any age.
How common is a new daily constant headache?
There are few studies on the prevalence of NDPH, but available data indicate that it is rare. The best available studies in Norway and Spain suggest that it occurs between 30 and 100 people out of 100,000.
Symptoms of a new daily constant headache
- The symptoms of NDPH are not unique, but some present in unusual ways.
- They are long-lasting.
- The requirement for a diagnosis of NDPH is that you have had headaches for at least three months.
- The pain is constant.
- Most experts define NDPH as constant pain at the onset.
Do you remember when it started?
- Official guidelines from the International Headache Society, the International Classification of Headache Disorders, require you to remember when the headache started.
- This means that a healthcare provider will only diagnose NDPH if you remember exactly when the headache started, including where you were and what you were doing.
- The pain is usually moderate to severe. Patients with NDPH usually have moderate or worse pain.
- Because the pain is also constant, it can seriously disrupt a person’s life and activities.
- Headaches associated with NDPH can appear as a typical tension headache, migraine, or both.
Symptoms of a tension headache may include:
Pain on both sides of the head. The pain feels like pressure or tension in or around the head. The pain doesn’t get worse depending on what you do. Symptoms of a migraine may include:
- Pain on one side of the head.
- Pain that feels like throbbing, throbbing, or throbbing.
- Photophobia (sensitivity to light or pain).
- Phonophobia (sensitivity or pain due to sounds).
- Nausea and vomiting.
- Dizziness Visual auras.
Causes of a new daily constant headache
Professionals do not know precisely why NDPH happens, but they inquire that specific events and conditions are likely triggers. Experiencing stressful events is common for people who develop NDPH. People are also likely to develop NDPH after certain medical events, but there is not enough information to confirm whether these events cause or contribute to NDPH. One of the main types of such triggers is infection. People often develop NDPH when they have a viral or bacterial infection, including:
- Epstein-Barr virus (the main cause of mononucleosis, or simply “mono”).
- Salmonella.
- E. coli.
- Dengue fever.
- COVID-19
- Meningitis or encephalitis.
You may also have secondary NDPH disease that directly affects the brain or central nervous system. Some examples of this are:
Subarachnoid hemorrhage- (bleeding in the subarachnoid space between the brain and the outer membrane; this often begins very suddenly with a “thunder headache”).
Low cerebrospinal fluid (CSF) pressure, is usually caused by a leak of cerebrospinal fluid in the skull or around the spinal cord.
High CSF pressure causes headaches.
Post-injury headache (for example from a concussion or traumatic brain injury).
Overuse of medications (especially those used to treat headaches or migraines) can cause “rebound headaches.”
Some primary headaches can be caused by lifestyle factors or situations, including:
- Alcohol, especially red wine.
- Some foods, such as processed meats, contain nitrates (headaches caused by food).
- Nicotine consumption (nicotine headache).
- Sleep disturbances or lack of sleep.
- Bad attitude.
- Physical activity, such as exercise (headache during exercise).
- Skipping meals (hunger headache).
- Coughing, sneezing, blowing the nose, straining (as with a bowel movement), or laughing or shouting (primary cough headache).
- Primary headaches are usually not dangerous, but they can be very painful and interfere with your daily life.
2 Secondary Headaches
The underlying disease causes the secondary headache. They are considered symptoms or signs of disease. Secondary headaches, which may not be dangerous and go away when the underlying condition is treated, include:
- Dehydration headache.
- Sinus headaches.
- Medication overuse headache.
1 Dehydration Headache
A dehydration headache occurs when your body is dehydrated (not getting the fluids it needs). Headaches often occur along with other symptoms of dehydration, such as dizziness, extreme thirst, and dry mouth. The pain usually goes away after drinking water, resting, and taking a pain reliever.
What is a dehydration Headaches?
- Dehydration headaches happen when your body doesn’t get enough fluids.
- Even mild dehydration can cause headaches. Other signs of dehydration (such as fatigue, dizziness, extreme thirst, and dry mouth) usually occur along with the headache.
- Headaches related to dehydration are often treated with home remedies such as drinking water, resting, and taking over-the-counter pain relievers.
- If you have signs of severe dehydration (such as confusion or dizziness), seek medical attention immediately.
How usual Are Dehydration Headaches?
- Nearly every individual has a headache from time to time.
- Headache is the most typical type of pain.
- They are caused by many different conditions, disorders, and diseases, including dehydration.
- Healthcare providers are not sure how many people suffer from dehydration-related headaches.
- In the United States, most people do not get enough fluids from food or drinking water. Insufficiency of fluids may lead to dehydration, which generates headaches.
- Babies, young children, and older adults are at greater risk of dehydration. Individuals with specific medical conditions (such as diabetes) are also at higher risk.
Symptoms and causes
- The pain caused by dehydration headaches can range from mild to severe.
- You may feel the pain all over your head or just in one place, such as the back, front, or side.
- The pain is generally like a dull ache, but it may also be sharp.
- You may have a throbbing (throbbing) headache or the pain may be constant.
- The pain may worsen when you bend over, shake your head, or move.
Other signs of dehydration generally arise along with a headache. They include:
- Dark urine (pee) and decreased need to urinate.
- Dizziness and confusion.
- Dry mouth. Fatigue.
- Hot cramps (muscle spasms).
- Loss of appetite.
- Fainting or fainting (fainting).
- This happens in severe cases of dehydration. Intense thirst (However you may not thirsty at all).
- If your child has a headache and signs of dehydration, call a healthcare provider right away.
- Symptoms of dehydration in infants and children form fewer trips to the bathroom (or fewer wet diapers), pale skin, and deficiency or lethargy. It is necessary to consult a doctor immediately.
What is dehydration?
- A person’s body is mainly made up of water.
- It is in your blood, your organs, your soft tissues, and your bones.
- When a person sweats and urinates, the body loses fluids and electrolytes.
- Electrolytes are minerals that help your body function as it should.
- Dehydration occurs when the amount of fluid leaving the body (including sweat and urine) is greater than the amount of fluid entering.
- Dehydration can be dangerous because it means your body isn’t getting the fluids it needs.
Dehydration can be caused by:
- Diarrhea and vomiting.
- Lack of adequate water supply.
- Excessive alcohol consumption, which can cause a hangover.
- Profuse sweating due to exercise, physical activity, or heat. Exercising at higher altitudes also increases the risk of dehydration.
- Some medications, such as diuretics (water pills), treat heart failure and other conditions.
- Water tablets help the body get rid of excess fluid and salt.
What causes dehydration headaches?
- When you are dehydrated, your brain and other body tissues shrink (get smaller).
- As your brain shrinks, it pulls away from your skull, compressing nerves and causing pain.
- Even mild dehydration can cause headaches.
- If you drink water and other liquids, the brain will fill up to its original size and the pain will disappear.
2-Sinus Headaches

A sinus headache is a symptom of sinus inflammation that causes pressure and pain in your face. A cold or allergy increases the risk of sinus infections and headaches. But the so-called sinus headache can be a migraine with a nasal symptom. In this case, your doctor can help you find long-term relief.
What are sinuses?
- The sinuses are a series of connected hollow spaces behind the cheekbones, forehead, and nose.
- The sinuses produce thin mucus.
- As air pushes via the sinuses into the lungs, mucus traps toxic particles such as dust, pollutants, and bacteria. The mucus discharges through the nose.
What is a sinus Headache?
- About 80% of what people call sinus headaches are migraines with nasal symptoms.
- A true sinus headache is caused by inflammation of the sinuses (sinusitis).
- The infection generates pain and tension in the sinuses.
How common is a sinus Headaches?
A sinus headache is very common with an infection. A sinus headache can also be felt if you have migraines, which occur in 12 percent of people.
What causes sinus Headaches?
- Sinus infections cause sinus headaches.
- Everything that generates mucus to build up in the sinuses may lead to a sinus infection, such as:
- The most common culprit is a cold.
- Seasonal allergies trigger mucus production.
- Nasal polyps can block mucus drainage.
- Deviated septum, where the line of cartilage and bone in the middle of the nose is not straight.
- A deviated septum can prevent mucus from draining properly.
- Too much mucus allows bacteria to grow.
- As bacteria build-up, they irritate the sinuses.
- In response, the sinus tissue swells and prevents mucus from passing through.
- Swollen, irritated sinuses filled with fluid make your face scarred and painful.
Can allergies cause sinus headaches (allergy headaches)?
- Allergies themselves do not cause headaches.
- But allergies can cause sinus congestion (nasal congestion), which can lead to sinus pressure, pain, and infections.
- If you have seasonal allergies (allergic rhinitis), you are also 10 times more likely to get migraines.
3 Drug overdose Headache
- A medication overuse headache is a vicious cycle of headaches with more and more pain relievers being used to relieve them, which actually leads to daily or almost daily headaches.
- Cracking the cycle impacts controlling an acute medication, taking preventative medication, and then using an acute medication with restrictions.
What is medication overuse Headache?
- overuse of medication Headache is precisely what its name implies: a headache brought on by using painkillers (pain) too frequently to treat a headache.
- Overuse of headache medications results in daily or near-daily headaches for which your current medications become less and less effective.
How does taking headache medication too often cause medication overuse headaches?
- When you get a headache, you probably take your acute (immediate relief) medicine.
- However, if your headaches do not get under control and more headaches develop, you will take more and more medications to control the headaches.
- So this vicious cycle of taking more and more painkillers to treat headaches actually leads to daily or almost daily headaches.
- Technically, medication overuse headache is defined as a headache that occurs at least 15 days per month in a person with a history of a headache disorder, who has used one or more acute medications for symptom relief for at least three months, and who has no other.
- known cause of the headache.
Who is most likely to get a headache from overuse of medications?
- At-risk groups include those with primary headaches such as migraines, cluster headaches, or tension headaches, whose headaches do not respond well to medication and require medication.
- Medication-induced migraine is more typical in middle age and 3 times more typical in females than males.
What are the symptoms of a medication overuse headache?
- Medication overuse headache symptoms vary in number, severity, and location.
- This is because headaches themselves are different and people with headaches use different types and different medications.
Common symptoms of a medication overuse headache include:
- Daily or almost daily headaches that usually start when you wake up.
- The headache gets better when you first take the pain reliever, but the headache comes back after you stop taking the medicine.
- The headache may feel like a dull, tension headache or be more severe than a migraine headache.
Other related symptoms include:
- Nausea. Irritability, restlessness.
- Bad sleep. neck pain
- Depression, anxiety.
- Runny nose, nasal congestion, watery eyes.
- Weakness
- Difficulty concentrating, memory problems.
What medications can cause medication overuse headaches?
Many common over-the-counter medications can cause headaches if taken too often. Drugs that were once considered “safe” are the most likely culprits. These drugs include:
- Aspirin.
- Sinus relief medications.
- Acetaminophen.
- NSAIDs, such as ibuprofen and naproxen.
- Sedatives for sleep.
- Codeine and prescription narcotics.
- OTC mixture headache medications containing caffeine (namely aspirin with caffeine; acetaminophen, aspirin, and caffeine, Bayer Select®, and others).
Other medications generally connected with medication overuse headaches are:
Ergotamine-containing preparations:
- Caffeine and ergotamine .
- Ergotamine (Ergomar®).
- Belladonna, phenobarbital, ergotamine (Bel-Phen-Ergot S®, Phenerbel-S®.
- Belladonna, caffeine, ergotamine (Cafatine PB®).
Butalbital combination analgesics:
- Aspirin, caffeine,
- Acetaminophen (Goody’s® Headache Powder, Excedrin®).
- Excedrin®.
Triptans:
- Sumatriptan (Imitrex®, Treximet®).
- Zolmitriptan (Zomig®).
- Rizatriptan (Maxalt®).
- Eletriptan (Relpax®).
- Almotriptan (Axert®).
- Frovatriptan (Frova®).
- Naratriptan (Amerge®).
Secondary headaches, which may be a symptom of a painful or potentially life-threatening condition, contain:
Spinal headache:
- A spinal headache is a severe headache that occurs when spinal fluid flows from the membrane that covers the spinal cord, usually after touching the spinal cord.
- Most spinal headaches can be treated at home, but long-term untreated back pain can lead to life-threatening complications such as subdural hematoma and seizures.
Thunderclap headache:
- A thunderclap headache is an exceptionally painful headache that arrives on unexpectedly, like a clap of thunder.
- This type of headache reaches its most intense pain within a minute and lasts at least five minutes.
- Although a headache caused by a thunderstorm can sometimes be harmless, it is important to seek medical attention immediately.
- They can be a sign of head injury or Cerebral hemorrhage.
- Reversible cerebral vasoconstriction syndrome.
- An impulsive, extreme upsurge in blood pressure.
What is the dissimilarity between a Headache and a migraine?
- Migraine is a kind of preliminary headache condition.
- Migraine is a common neurological condition that induces a type of sign, the most notable of which is a throbbing headache on one side of the head.
- Migraines are often aggravated by physical activity, light, sounds, or smells.
- They generally last at slight four hours or even a day.
Who is affected by Headaches?
- A person may have a headache, including kids, teenagers, and grown-ups.
- About 96% of people experience a headache at least once in their life.
- About 40 percent of people worldwide have tension headaches and about 10 percent have migraine headaches.
The main cause of Headache
- Interactions between impulses from the brain, blood vessels, and peripheral nerves result in headaches.
- During a headache, several mechanisms activate certain nerves that affect muscles and blood vessels.
- These nerves send pain signals to your brain, causing headaches.
Is Headache hereditary?
- Headaches grow to conduct in families, especially migraines.
- Children with migraines usually have at least one biological parent who also has migraines.
- In fact, children whose parents have migraines are up to four times more likely to develop migraines.
Headaches can also be triggered by environmental factors common in the family household, such as:
- Eating specific foods or components namely caffeine, alcohol, fermented foods, chocolate, and cheese.
- Exposure to allergens. Used smoking. Strong odors from chemicals or perfumes.
Which Headache symptoms require immediate medical attention?
If you or your child has any of these headache symptoms, see your doctor right away:
A sudden, new, and severe headache. Headache accompanied by fever, shortness of breath, stiff neck, or rash. A headache that occurs after a head injury or accident. A unique kind of headache behind the age of 55. Also, seek immediate medical attention if the headache is accompanied by neurological symptoms, such as:
- Weakness
- Dizziness
- Sudden loss of balance or fall.
- Numbness or tingling.
- Paralysis.
- Speech difficulties.
- Mental confusion.
- Scenes.
- Personality changes / inappropriate behavior.
- Vision changes (blurred vision, double vision, or blind spots).
Diagnosis and test
If you have frequent or severe headaches, contact your doctor.
Getting your headaches properly diagnosed is important so that your provider can prescribe the specific treatment that will best help you. Your physician will conduct a physical exam, discuss the medical history, and discuss the headache symptoms with you. This discussion is part of the headache assessment.
During a headache diagnosis, the physician will ask you about your headache history, including:
- What does a headache feel like?
- How often do you have headaches?
- How long does the headache last each time?
- How much does it give you a headache?
- What foods, drinks, or events trigger your headaches?
- How much caffeine do you drink per day?
- What is your stress level?
- What are your sleeping habits?
A headache can be more accurately diagnosed if you know:
- When the headache started.
- Whether it is one type of headache or several types of headaches.
- If physical activity makes the headache worse.
- Who else in your family has headaches?
- What symptoms occur between headaches?
- After completing the medical history portion of the evaluation, your provider may perform physical and neurological exams.
They look for signs and symptoms of a disease or condition that may be causing the headache, including:
- Fever.
- An infection and High blood pressure.
- Muscle weakness, numbness, or tingling.
- Excessive fatigue.
- Loss of consciousness. Balance problems and frequent falls.
- Vision problems (blurred vision, double vision, blind spots).
- Mental confusion or personality changes. Scenes.
- Dizziness Nausea and vomiting.
- Neurological tests focus on ruling out diseases that can also cause headaches.
- A disorder of the central nervous system can be suspected in the event of severe headaches.
- After evaluating your headache history, physical exam, and neurological exam results, your doctor should be able to determine
- what type of headache you have, whether it’s a serious problem, and whether further testing is needed.
- If they are doubtful of the cause, they can refer you to a headache specialist.
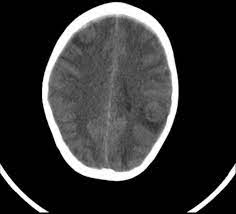
What tests are used to diagnose headaches?
- Although scans and different imaging examinations may be necessary for ruling out other conditions, they are not useful in analyzing migraines, cluster headaches, or tension headaches.
- But if your doctor thinks your headaches are due to another medical condition, he or she may order several imaging tests.
- A CT scan or MRI can help determine if your headaches are related to a problem with your central nervous system. Both tests provide cross-sectional images of your brain that can show abnormal areas or problems.
Treatment of Headache
- Therapy of a headache depends on the classification.
- One of the most important aspects of primary headache treatment is identifying a trigger.
- Understanding them – typically by maintaining a headache log – may decrease the number of headaches.
- Once you know your triggers, your healthcare provider can tailor treatment to suit you.
- For example, you may have a headache when you are stressed or anxious.
- Counseling and stress control methods can assist you in better dealing with this trigger.
- By reducing your stress levels, you can prevent tension headaches.
- Not all headaches require medication. Various treatments are available.
Depending on the type, frequency, and cause of the headache, treatment options include:
- Stress management.
- Biofeedback Medicines.
- Treatment of the underlying disease/cause.
- Managing stress to treat headaches
- Stress management teaches you ways to deal with stressful situations. Relaxation techniques help reduce stress.
- You use deep breathing, muscle relaxation, imagery, and music to relieve tension.
Biofeedback for Headache
Biofeedback guides you to remember when tension is building up in the body. You will know how your body responds to stressful conditions and how to calm down. During biofeedback, sensors are attached to your body. They regulate your involuntary physical responses to a headache, including:
- Respiratory rate.
- Pulse. Rhythm.
- Temperature.
- Muscle tension.
- Brain activity.
Medicines for Headache
- Periodic tension headaches generally respond well to over-the-counter pain relievers.
- But be aware that using these medications too often can cause long-term daily headaches (medication overuse headaches).
- For regular or unbearable headaches, your provider may suggest prescription headache medications.
- Triptans and other medications can stop a migraine attack.
- You take them at the first sign of an impending headache.
- Treatments for high blood pressure, seizures, and depression can sometimes prevent migraines.
- A healthcare provider may recommend trying some of these medications to reduce the frequency of headaches.
Treatment of the underlying disease causing the secondary headache
- Treatment of a secondary headache contains treatment of the underlying disease that caused it.
- For example, surgery is often required to treat the underlying cause of a secondary cough headache.
Home exercise program
You can fete the periodic mild headache at home with over-the-counter pain relievers. Other headache self-treatments include:
- Use hot or cold packs to the head.
- Doing strenuous exercises.
- Massage your head, neck, or back.
- Rest in a dark and quiet room.
- take a walk
Prevention
- The key to preventing headaches is to find out what triggers the headache.
- Exiles are very individual to each person – what gives you a headache may not be a problem for others.
- Once you identify your triggers, you can avoid or minimize them.
- For example, you may find that strong smells invigorate you.
- Avoiding perfumes and scented products can make a big difference in the number of headaches you have.
- The same goes for other common triggers such as boring food, lack of sleep, and bad attitude.
- Many people are unable to identify triggers.
- In this case, a more individualized multidisciplinary approach with a headache specialist is often needed.
FAQ
The headache is escorted by high fever, confusion, stiff neck, prolonged vomiting, slurred speech, or numbness or weakness, particularly on one side of the body. Headache medicine does not relieve chronic or excruciating pain.
Rare headaches are typical and generally do not require medical attention. Nevertheless, contact your doctor if: You usually have two or more headaches a week. Most days you take a pain reliever for a headache.


9 Comments