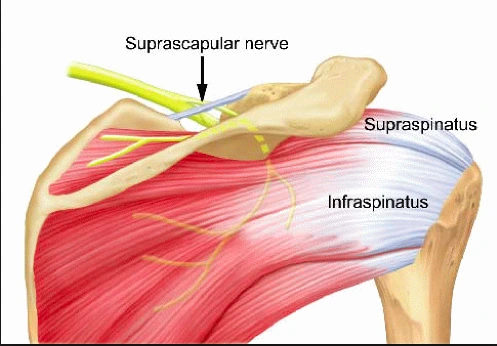
Suprascapular nerve palsy:
Suprascapular nerve palsy is a condition in which injury or compression of suprascapular nerve leads to the supraspinatus and/or infraspinatus muscles.
The suprascapular nerve is a mixed nerve (Motor and sensory) of the upper limb. Suprascapular nerve injury gives clinical significance to shoulder pain and upper limb weakness due to its own role. The suprascapular nerve gives both the motor and sensory branches to the muscle. Suprascapular nerve palsy happens when the suprascapular nerve is damaged. That can cause pain and weakness in the supraspinatus and infraspinatus muscles supplied by the suprascapular nerve.
Table of Contents
Anatomy of suprascapular nerve:
The suprascapular nerve starts from the upper trunk of the brachial plexus. The nerve roots of the suprascapular nerve are C5 and C6. It may have roots in C4 also. From the posterior triangle of the neck, the nerve runs over the upper part of the scapula, then downward and laterally, parallel to the omohyoid muscle belly.
Then it passes below the suprascapular ligament, through the suprascapular notch, and into the supraspinous fossa where it supplies the supraspinatus muscle and articular branches to the glenohumeral and acromioclavicular joints. Through it curves around the spinous process of the scapula and continues along the lateral scapula to the spinoglenoid notch and then passes under the inferior transverse ligament and enters into the infraspinous fossa where it supplies the infraspinatus muscle. The suprascapular nerve also provides sensory supply to the glenohumeral and acromioclavicular joint.
- Origin – Superior trunk of brachial plexus.
- Branches – Motor muscular branches, articular sensory branches.
- Supply – Motor supply: supraspinatus muscle, infraspinatus muscle.
- Sensory supply: glenohumeral and acromioclavicular joints.
What is suprascapular nerve palsy:
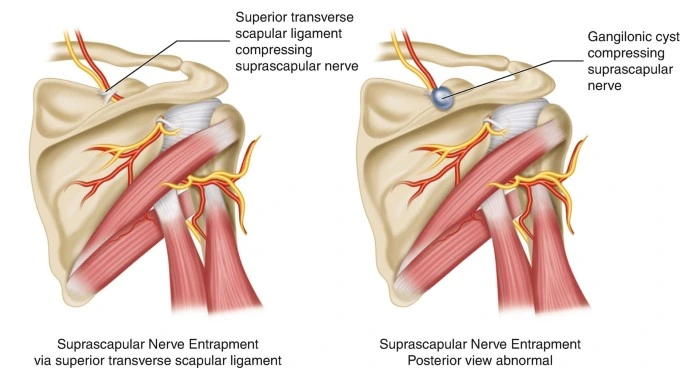
Suprascapular nerve palsy is an uncommon condition of shoulder pain and dysfunction, but it can lead to significant disability. Injury to the suprascapular nerve generally occurs by either a traction injury or a compressive mechanism. Suprascapular nerve injury most commonly occurs at the suprascapular and spinoglenoid notches. The suprascapular nerve gives motor branches to the supraspinatus muscle distal to the suprascapular notch and proximal to the spinoglenoid notch. So nerve entrapment at the suprascapular notch will affect the both supraspinatus and infraspinatus muscles.
“Suprascapular nerve entrapment syndrome (SNES) is one type of neuropathy in which the nerve is impinged along its course, most commonly at the suprascapular notch (SSN)”. Kopell and Thomas first described it in 1959. In this condition, weakness in the abduction and external rotation movement and dull aching pain is also present. PARESIS is the primary, therefore, upper limb neurological examination will reveal normal deep tendon reflexes and sensations.
Causes of suprascapular nerve palsy:
Causes of SSN injury include primary etiologies that can be given the anatomical entrapment of the suprascapular nerve along with the nerve’s course or functional impingement of this nerve with repetitive use, as in overhead athletes such as baseball players, tennis players, weight lifters, swimmers, and volleyball players.
Other etiology of SSN are the following:
- Compression neuropathy is the most common cause of suprascapular nerve palsy and it results from nerve entrapment. The common area of nerve entrapment is the suprascapular notch and the spinoglenoid notch.
- Shoulder trauma resulting from scapular fracture, clavicle, and proximal humerus can significantly damage the suprascapular nerve.
- Post-surgical complications after open or arthroscopic shoulder surgery can lead to suprascapular nerve damage.
- Less scapular movement can lead to suprascapular nerve palsy.
- Tumors, cysts, and other lesions around the shoulder joint may compress the suprascapular nerve.
- Systemic conditions like lupus erythematosus and rheumatoid arthritis.
- Glenohumeral dislocations.
- Acromioclavicular (AC) joint injuries.
- Unknown injuries during arthroscopic or open shoulder surgeries.
Space-occupying lesions:
- Ganglion cysts
- Paralabral cysts
- Bone cysts
- Osteosarcoma, soft tissue sarcoma, metastatic lesions.
Systemic conditions:
- Systemic lupus erythematosus (SLE).
- Rheumatoid arthritis (RA).
Moreover, while isolated SSN injuries are uncommon, it is the most frequently injured peripheral branch of the brachial plexus in athletes.
The former includes throwing athletes and those athletes exposed to repetitive overhead trauma and repetitive motions, such as baseball players, tennis players, weight lifters, swimmers, and volleyball players.
Signs and symptoms of suprascapular nerve:
If the supraspinatus muscle is affected so abduction movement of the shoulder joint may be decreased. Like the movement of bringing your arms up from your sides and clapping above your head.
If the infraspinatus muscle is affected external rotation movement may be affected. Like when we seat in the car and reach backward to keep a seat belt.
Muscle wasting: Wasting of these two muscles is visible when at the shoulder.
Pain: Pain is different, Sometimes it may be impingement-type pain and sometimes there is a general aching pain around the shoulder or over the superior or posterolateral aspect of the shoulder. Pain is present during the activity. In neuralgic conditions, severe pain may be present in the starting stages.
Pain is radiate to the neck, upper part of the chest, or back. Cross-body adduction and internal rotation may increase pain. Mostly 40% of cases present with any type of trauma of the shoulder.
The most common clinical presentation of suprascapular nerve palsy is atrophy of the supraspinatus and/or infraspinatus muscles.
Evaluation of the suprascapular nerve palsy:
- Nerve conduction studies and electromyography: They are used for the diagnosis of suprascapular nerve palsy. Prolonged latency, reduced amplitude, fibrillation potentials, and positive sharp waves in the nerve conduction study indicate suprascapular nerve compression and nerve denervation.
- X-ray: It can help rule out trauma to the surrounding bones.
- CT scan, MRI, and diagnostic ultrasound: These can help localize the site of injury. MRI tests are helpful in diagnosing a ganglion cyst and confirming the pattern of muscle wasting.
- By the MRI to diagnose neuropathy, this sign is the most significant. “Muscular edema may be the hydration modifications of the muscular mass, in the case of the denervated muscles”.
- EMG test: It is important to check the neuropathy condition for any nerves.
The diagnosis depends on the clinical examination, like depends on patient history and physical examination.
Differential diagnosis of the suprascapular nerve:
The diagnosis of SSN injury can be difficult because the symptoms overlap with other pathologies of the shoulder and cervical spine region. The differential diagnoses are the following:
- Cervical radiculopathy (C5-6).
- Parsonage-Turner syndrome.
- Brachial plexopathy (upper trunk).
- Rotator cuff injury (e.g., tendinitis, bursitis, partial or complete strain/tear)
- Subacromial impingement syndrome.
- Scapular dyskinesia.
- Superior labral tear from anterior to posterior (SLAP tear)
- Adhesive capsulitis
- Glenohumeral arthritis
- Facet mediated pain
Treatment of suprascapular nerve palsy:
Medical Treatment:
Non-steroidal anti-inflammatory drugs and anesthetic injections are used to reduce pain.
Surgical management:
Surgery is advised when the n any improvement is seen in 6 to 12 months by the conservative treatment. Surgical decompression of the suprascapular nerve is done.
General guidelines:
Pain:
Ice packs or a Cold pack apply on the pain area for up to 15 mins to help reduce pain. In order to maintain a dry wound cover the dressing before
applying the ice pack.
The wound:
This operation is done with usually three or four 5mm puncture wounds. There will be no stitches only small sticking plaster strips cover the wounds.
Wearing a sling:
When you return from home after removing the cast wear a sling to avoid the jerky movement. Apply the cold pack over the affected area to reduce the pain. People wear the sling at night for a little longer if the patient has tenderness over the shoulder.
Physiotherapy treatment of suprascapular nerve palsy:
Physiotherapy helps to improve functional movement and muscle strength.
It is also required after the surgery, to encourage good movement, help to decrease pain, and rehabilitate the muscles back to normal function. the patient will start exercise within 2 weeks of the surgery. This surgery is needed, 100% of athletes who had decompression at the suprascapular notch and 91% of athletes who had decompression at the spinoglenoid notch were able to return to sport.
Sports-specific activity is advised for overhead athletes to prevent repetitive trauma at the shoulder. a whole range of motion should be maintained at the shoulder to avoid adhesive capsulitis. Posterior capsule stretching of the shoulder and strengthening of the rotator cuff and shoulder muscles are advised.
The role of physical therapy.
The goal is to strengthen muscles and regain the muscular strength of the shoulder. Using proper posture, scapular retraction exercises, and proprioceptive exercises may be effective.
Mostly two main focuses of our physiotherapy program; 1) to Regain external rotation strength and muscle hypertrophy, and 2) to Protect the shoulder joint from repetitive and jerky movements.
Strengthening exercise for the external rotation movement:
The following sequence is found to be clinically helpful. The exercise duration and protocol depend on the patient’s condition and the cause of the neuropathy.
Alternating isometrics in sitting using a towel.
Isometric external rotation on the affected arm which is moving to the unaffected arm by the theraband. This provides a fluctuating resistance on an isometric hold.
A progressive external rotation strengthening exercise is done once an active range of movement has been regained.
Optimizing periscapular muscle control and posture:
Advise the patient about the exercises to promote postural awareness and control of the glenohumeral joint and scapula. The Main complaint of the patient having a lack of awareness of positioning of the humeral head at rest or during activity and pain with shoulder elevation, abduction, or flexion movement. Most patient does the forward position and anteriorly rotated humeral head.
Do the shoulder exercise with the theraband to provide proprioceptive feedback to the patient.
The first of to teach the patient how to plank in quadruped or a forward kneeling position. Once the patient is able to do the scapular movement (pressing away from the floor and bringing ribs to meet the scapula), that patient was able to actively move through a kneeling push-up. Once their strength progresses the patient may be able to do a full plank and full push-up progressively without aggravating their shoulder.
After the rehabilitation, as the patient strengthens their abduction and external rotation above 90 degrees, that may be advised to use this prone abduction exercise.
Stretching of posterior capsule:
Stretching the posterior capsule is important in athletes, as it is released by stretching to reduce tension on the spinoglenoid ligament, which can reduce repetitive microtrauma during any sports activity.
Home advises:
- Teach the patient to apply the hot pack and cold pack regularly.
- Do a normal scapular movement exercise at home but not a jerky movement.
- Advice to the patient to can’t lift a heavy weight for some period of time.
Post-surgical rehabilitation:
After the surgery, the patient’s arm is immobilized in a sling for 2-3 days, for the patient’s comfort. Patients are encouraged to progress their passive and active range of motion as able to do. A strengthening program is started when the full range of motion is achieved. the first patient does the scapular movement passively by the therapist and then assisted movement and then the patient does the whole movement actively without any support or assistance. After that therapist plans the strengthening program according to the patient’s condition.
FAQ:
What causes suprascapular nerve palsy?
Suprascapular nerve palsy mainly happens due to suprascapular nerve compression. It can be caused by: Trauma to the shoulder or damaging
structures surrounding the nerve. The other cause of functional impingement of this nerve with repetitive use, like in overhead athletes such as
baseball players, tennis players, weight lifters, swimmers, and volleyball players.What are the signs and symptoms of suprascapular nerve palsy?
In this condition, patients will present with dull, aching pain over the superior or posterolateral aspect of the shoulder. Pain radiates down to the neck,
upper limb, or chest. Cross-body adduction and internal rotation may increase pain.
The most common symptom of this condition is atrophy of the supraspinatus or infraspinatus muscles. Abduction or external rotation movement
affected due to these two muscles’ atrophy.What muscles are affected by the suprascapular nerve?
The suprascapular nerve supplies two muscles of the posterior shoulder girdle. These are the infraspinatus or the supraspinatus muscles.
The Infraspinatus muscle is the primary external rotator of the arm at the shoulder, and the supraspinatus muscle is help to initial phase of abduction
movement.What happens when the suprascapular nerve is damaged?
A suprascapular nerve injury presents as a vague shoulder pain with associated weakness in shoulder abduction and external rotation movement. The
shoulder girdle muscle is supplied by the suprascapular nerve and this may atrophy.What is the treatment for suprascapular nerve palsy?
Firstly Conservative treatment includes rehabilitation programs, nonsteroidal anti-inflammatory drugs, and lifestyle modification. Physical
therapy treatment aims to strengthen the rotator cuff muscles, trapezius, levator scapulae, rhomboids, serratus anterior, and deltoid muscle(s).
If the condition is not cured surgery may require and post-surgical rehabilitation is also necessary.How long does it take for a suprascapular nerve to heal?
If any surgical repairs are needed, the patient can expect to be immobilized with a sling for six weeks followed by four to six months of formal
physical therapy. After the release of the nerve, it may require six months to a year, or longer, for the nerve to recover, which is followed by the recovery
of muscle.