Duchenne Muscular Dystrophy (DMD)
Table of Contents
What is Duchenne muscular dystrophy(DMD)?
Duchenne muscular dystrophy(DMD) is the most common hereditary neuromuscular disorder that affects all races and ethnically. While some affecting newborn babies may have some mild decreased muscle tone or “floppiness”(hypotonicity ), other symptoms are rarely present at birth or in early infancy. Early gross motor evolutionary milestones, including rolling over, sitting, and standing, are usually met at the normal ages, or slightly later than normal.
Those affected usually maintain the ability to be able to use their hands to hold and use eating and writing implements. All children with DMD will have some degree of intellectual impairment, with most having only learning incapacities.
It is a genetic problem that causes muscles to damage and waste (become smaller and waste away).
Muscle weakness may affect the skeletal muscle and the heart muscle. It is caused by the inadequacy of muscles to react to nerve impulses from the brain.

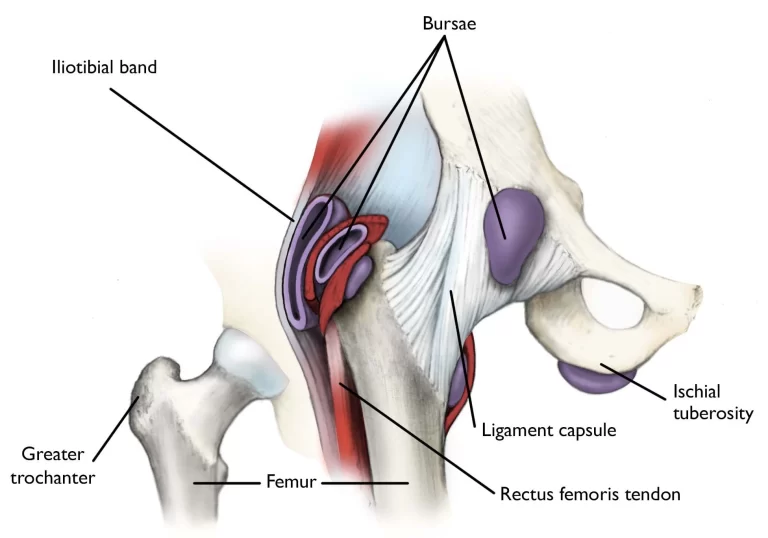
Clinically relevant anatomy:
All types of muscular dystrophy are caused by dystrophy defects in genes (the element of inheritance that parents transfer onto their children) which result in gradual muscle weakening due to muscle cells rupturing down and progressively becoming lost. This type of dystrophy is an X-linked genetic disorder influenced firstly boys (with extremely rare immunities) and difficulty in this gene results in a deficiency in a single significant protein in muscle fibers called dystrophin.
Causes of Duchenne muscular dystrophy(DMD):
DMD is a genetic disease. Those who receive it have a defective gene related to a muscular protein called dystrophin. This protein keeps muscle cells undamaged. Its absence causes rapid muscular degradation as a child with DMD grows.
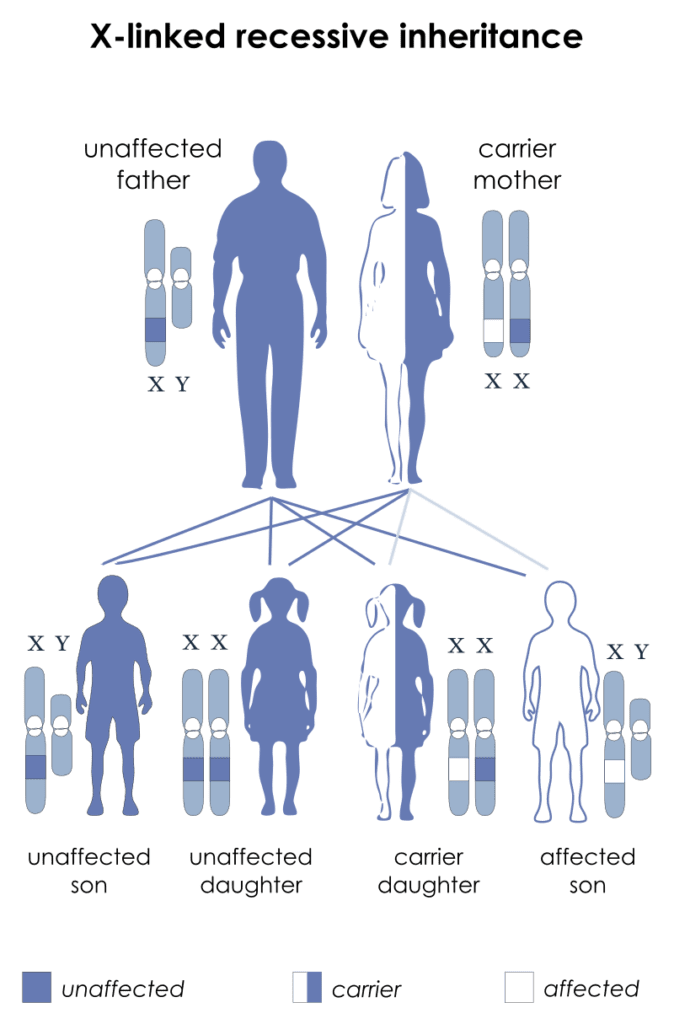
It is inherited as an X-linked disease. X-linked genetic Causes:
DMD is a genetic disease. Those who receive it have a defective gene related to a muscular protein called dystrophin. This protein keeps muscle cells undamaged. Its absence causes rapid muscular degradation as a child with DMD grows.
It is inherited as an X-linked disease. X-linked genetic diseases are conditions caused by an abnormal gene on the X chromosome and appear mostly in men. Women that have a deficient gene present on one of their X chromosomes are bearers of that disorder. Carrier females usually do not show symptoms because women have two X chromosomes and only one bearer of the deficient gene. Males have one X chromosome that is inherited from their mother and if a male inherits an X chromosome that includes a defective gene he will develop the disorder.
Women bearer of X-linked diseases have a 25% chance with each maternity to have a carrier daughter like themselves, a 25% possibility to have a non-carrier daughter, a 25% chance to have a son impacted with the disease, and a 25% chance to have a not affected son.
If a man with an X-linked disorder is able to imitate, he will pass the defective gene to all of his daughters who will be bearers. Men cannot pass an X-linked gene to their sons because they always pass their Y chromosome instead of their X chromosome to the male child.
Some females who inherit an individual copy of the disease gene for DMD (gene carriers) may expose to some of the symptoms associated with the disorder such as weakness of some muscles, especially those of the arms, legs, and back Carrier females who develop signs of DMD are also at risk for developing heart abnormalities, which may present as exercise intolerance or shortness of breath. If left untreated, heart abnormalities can cause life-dangerous difficulties in such affected females.
DMD is caused by alterations of the DMD gene located on the short arm of the X chromosome. Chromosomes, which are present in the nucleus of human cells, carry the hereditary evidence for each individual. Human body cells normally have 46 chromosomes. Human pairs of chromosomes are numbered from 1 through 22 and the sex chromosomes are hereditary suggesting X and Y. Male gender have one X and one Y chromosome and the female sex has two X chromosomes. Each chromosome has a short arm specified “p” and a long arm indicated “q”. Chromosomes are further classified into many bands that are numbered.
The DMD gene regulates the production of dystrophin, a protein that appears to play an essential role in maintaining the integrity of cell membranes in skeletal (voluntary) and cardiac muscle cells. Dystrophin is found connected to the internal side of the membrane that surroundings muscle fibers. Mutation of the DMD gene will result in a lack of the dystrophin protein, leading to the degradation of muscle fibers. The body can restore some muscle fibers, but over time more and more muscle fiber is lost. Dystrophin is present in BMD, an associated disease, but it is shortened or only present at insufficient levels to perform its functions properly.
Although most boys with DMD inherit the abnormal gene from their mothers, some may develop the disease as the result of a spontaneous mutation of the dystrophin gene that occurs randomly for unidentified reasons.
Signs and Symptoms of Duchenne muscular dystrophy (DMD):
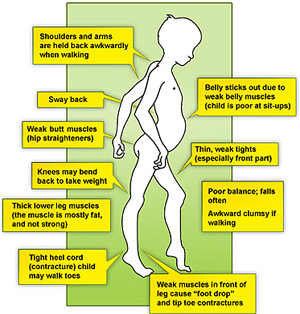
If your child has DMD, you’ll notice the first signs before they turn 6 years old. Usually, firstly affects the muscles of the legs, so they’ll maybe start to walk much later than other children their age. Once they can walk, they may fall down and have difficulty to climbing stairs or getting up from the floor. After some years, they might also begin to paddle or walk on their toes.
DMD can also harm the lungs, heart, and other body parts. As they get older, children might have other signs, including:
- Shortness of breath.
- Headaches.
- Shortened, tight muscles in their legs, are called contractures.
- Trouble concentrating.
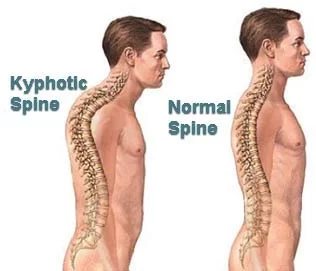
- A curved spine is also called scoliosis.
- Sleepiness.
- Problems with learning and memory.
- Shortness of breath.
- scoliosis.
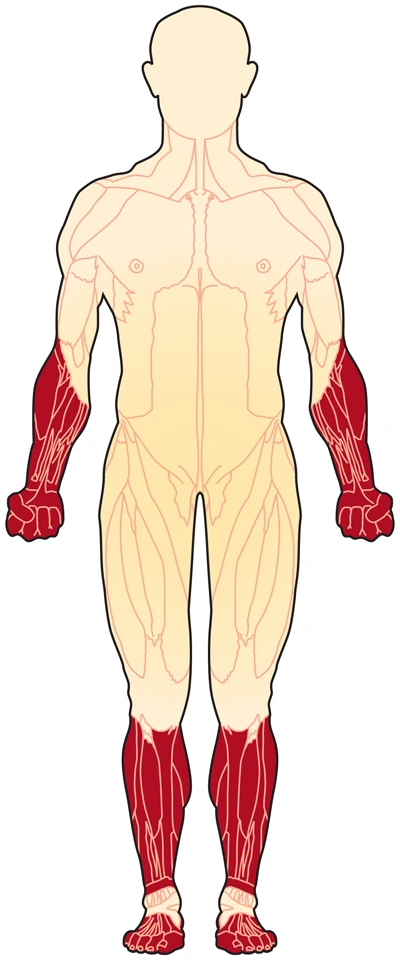
- Muscle weakness: Begins in the lower limbs and pelvis, but also occurs less severely in the upper limb, neck, and other areas of the body.
- Problems with motor activity (running, hopping, jumping).
- Frequent falls.
- It is difficult to get up from a lying position or climb stairs.
- Difficulty in breathing due to a weakness of the respiratory muscles.
- Gradual deterioration of muscle weakness.
Calf muscles become expanded (pseudohypertrophy), and thigh muscles become thin.
Muscles of the forearm and tongue may become expanded.
Weakness in chest and throat muscles.
A classic sign of DMD is trouble getting up from a lying or sitting position as presented by a positive Gowers’s sign.

Muscle stiffness can cause cramps at times, but DMD isn’t painful. Some children with the diseases have learning and behavior problems, DMD doesn’t affect the child’s intelligence. With life anticipation of about 18 years of age, heart and respiratory complications are most commonly the cause of death in patients with DMD.
Investigations:
Hereditary counseling is advised for people with a family history of the disorder. DMD can be identified with about 95% accuracy by inherited studies performed during pregnancy. Creatine kinase (CPK-MM) levels in the bloodstream are immensely high. Electromyography (EMG) shows that deficiency is caused by damage to muscle tissue rather than by the destruction of nerves.
DNA test:
The muscle-specific isoenzyme of the dystrophin gene is composed of 79 exons, and DNA examination (blood test) and analysis can usually identify the specific type of alteration of the exon or exons that are affected. DNA testing confirms the diagnosis in many cases.
Muscle biopsy:
If DNA examination fails to find the mutation, it may be performed a muscle biopsy test. A small sample of muscle tissue is removed using a biopsy needle. The key tests carried out on the biopsy sample for DMD are immunohistochemistry, and immunocytochemistry, and they should be represented by an experienced neuromuscular pathologist. These tests provide information about the presence or absence of the protein. A positive test is considered an absence of the protein for DMD. Where dystrophin is present, the tests show the amount and molecular size of dystrophin, helping to differentiate DMD from milder dystrophinopathy phenotypes.
Prenatal tests:
This test can be considered when the mother is a known or suspicious carrier. Many mutations are liable for DMD, and some have not been determined, so genetic testing may be falsely negative if the suspicious mutation in the mother has not been established.
Prior to invasive testing, determination of the fetal sex is important; while males are sometimes affected by this X-linked disorder, women’s DMD is exceptionally rare.
Treatment of Duchenne muscular dystrophy (DMD):
Medical Treatment:
There is no known medication for DMD. Treatment aims to control symptoms to improve better life.
Steroid medication can slow the waste of muscle strength. They may be started when the child is analyzed or when muscle strength starts to decline.
Other treatments may include:
- Albuterol is used for people with asthma
- Fish oil
- Coenzyme Q10
- Creatine
- Amino acids
- Green tea extracts
- Vitamin E
However, the assets of these treatments have not been proven. Genetic therapies may be helpful to many patients, depending on the genetic cause. Each therapy only works on a minor number of patients, depending on their particular mutation.
Treatments include:
- Vitolarsen
- Ataluren
- Eteplirsen
- Golodirsen
Other treatments may include:
- Orthopedic appliances are used for improving mobility (such as braces and wheelchairs).
- Drugs are used to help and improve heart function, such as angiotensin-converting-enzyme inhibitors, diuretics, and beta-blockers
- Assisted ventilation is used during the day or night.
- Drugs are used to help and improve heart function, such as angiotensin-converting enzyme inhibitors, diuretics, and beta-blockers.
- Proton pump inhibitors (for people with gastroesophageal reflux)
- Spine surgery to treat gradual scoliosis for some individuals.
Physiotherapy Treatment of Duchenne muscular dystrophy (DMD):
The lack of physical activity and the use of steroids can lead to too much weight gain. inaction such as bed rest) can make the muscle disorder poor. Physiotherapy may help to retain muscle strength functioning. Speech therapy is often needed.
One of the restrictions of the above measure is that they focus on either focus ambulant or non-ambulant patients. However, as the disorder progresses, the result indicators change, making it complicated to use a single outcome measure to examine the patient. Studies are being carried out to build a consistent measure for muscular dystrophy conditions.
Locomotion aids will be given to help the child be as independent as possible. These can include a walker in the initial phases and can gradually progress to a powered wheelchair. In-home uplifts are useful for the protectors when they need help to move the child. Standing structures also become useful when the child can no more stand on their own. This helps the child obtain the advantages of standing, such as greater bone density, and stretching the muscles even if the child cannot stand on their own. Knee-ankle-foot orthosis (KAFOs) may be used as well. It has been found to sustain the child’s independent mobility. These should be used side by side mobility aids, such as a zimmer frame.
Some families may consider surgical procedures for their children. Common surgeries for children with DMD include foot surgery, insertion of a supply tube, and spinal surgeries to correct scoliosis. There is many of information to examine before surgery, such as the effect of general anesthesia. Families need to evaluate the benefit of the surgery with the dangers before making a decision. For example, evidence has been found that surgery to correct scoliosis has improved respiratory function, and it also increases the cosmetic appearance and comfort of the child.
Preschool Age:
In this stage, the child will be healthy and not need much treatment.
Management entails:
Provided information about DMD.
Recommendation to a professional team (for example, physiotherapist, a pediatrician or neurologist, and specialist nurse) to supervise child health.
Guidance about the right level of exercise.
Hereditary advice for the family.
Treatment in Age 5-8 Years:
Between the ages of 6-11, there is a steady decrease in muscle power and by the age of 12, most children are wheelchair bound. There are other complications around children being reliant on wheelchairs, such as scoliosis and breathing problems. Some support may be needed for the lower limbs through night-time ankle splints or with knee-ankle-foot orthoses. There is no proof of an important advantage from any interference for increasing ankle range of motion.
Treatment with corticosteroids can help to sustain the child’s muscle strength. This includes taking medication such as deflazacort or prednisolone as a long-term treatment.
Treatment in 8 Years-Late Teenage Years:
After some time the age of 8 years, the child’s leg muscles become considerably weakest. Walking gradually gets more tricky, and a wheelchair is needed. The age period at which this occurs changes from person to person, but it is usually around age 9-11 years.
With corticosteroid treatment, with DMD some patients can walk for longer. An RCT in DMD children aged 6 to 10 years indicates that bicycle ergometer and treadmill exercise along with physiotherapy treatment programming considerably improves functioning capacity of walking (6-minute walk test) and balance. The physiotherapy management program included slight calf muscles, triceps, and biceps muscles), gait, and balance exercises.
Treatment in Late Teenage Years-Twenties:
At this stage, muscular weakness becomes more problematic. Developing help and community alterations are needed. Complications such as chest diseases are likely to rise, so more therapeutic monitoring and treatment are required.
Outlook (Prognosis): Duchenne muscular dystrophy leads to gradually deteriorating impairment. Death often occurs from lung disorders, although advances in considerate care have caused in many men living to age 35 years.
Outcome scales: Outcome scales for an individual with DMD vary according to the progression of the disease.
Outcome scales to quantify disease progression include:
- Time is taken to climb four steps.
- Time is taken to rise from the floor.
- Performance of upper limb.
- 6-minute walking test.
Exercises for Duchenne muscular dystrophy (DMD):
Aerobic Exercise:

Aerobic exercise increases the heart rate. Those with muscular dystrophy should be able to exercise while maintaining communication. Aerobic exercise will depend on condition, but low-impact exercises such as fast dancing, walking, cycling, and swimming, are options.
Ideally, 20 minutes of exercise a day between four and six times per week, but you might want to start by doing five or 10 minutes a day and building your fitness levels up slowly. Ensure warm-up is done gently before stretching and exercising muscles, it decreases the chance of injury.
Some exercises and stretches are adapted for muscular dystrophy patients.
Stretching Exercise:
Forearm Supination Stretch:
Position: Supine

Instructions: The forearm holds just above the wrist and turns the arm to a palm-up position. Stabilize the elbow at the side of the body. Hold for 60 seconds and then reposition after repeating 60 seconds.
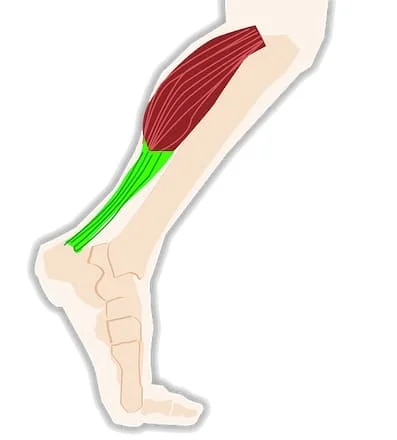
Achilles(Gastrocnemius) Stretch:
(1) Position: Supine

Instructions: patient position is supine lying, place a small roll under the knee. Grip the heel and pull to stretch the Achilles then flex the foot. Hold for 60 seconds and then reposition after repeating for 60 seconds.
(2) Position: Self Stretch
Instructions: The patient’s position is one foot in front of the other foot while standing at a wall. Keep the back knee straight, Lean forward and toes pointed forward. Hold for 60 seconds and after than relax and again repeat.

Hamstring Stretch:
(1) Position: Supine
Instructions: Stabilize at the knee and flex the hip 90 degrees. Slowly raise the lower leg until a stretch is felt in the back of the thigh, with another hand. Hold for 60 seconds and then reposition after repeating for 60 seconds.

(2)Position: Wall Self Stretch
Instructions: position at the corner of two walls and place a heel on the wall and the other leg along the wall on the floor. Until a stretch is felt, slowly move closer to the wall in the back of the thigh. Hold for 60 seconds and repeat 1-2 times.
IT Band Stretch and Iliopsoas:

Position: Prone
Instructions: Support the knee with one hand, stabilize the pelvis with one hand. . Pull it up then toward the other leg. Hold for 60 seconds and then reposition after repeating 60 seconds.
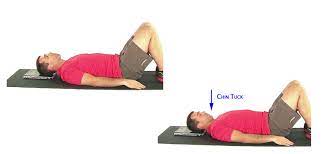
Neck Extensor:
Position: Self Stretch
Instructions: patient position is a comfortable neck position looking forward. Insert (Tuck) the chin down while extending the back of the neck. Hold 5-10 seconds and repeat 5-10 times.
Soleus Stretch:

Position: Prone
Instructions: Flex your knee 90 degrees, while lying on your stomach, Stabilize the lower leg. Grip the foot and heel and press down to stretch the calf. Hold for 60 seconds and then reposition after repeating 60 seconds.
Trunk Rotation:

Trunk Rotation
Position: Self Stretch
Instructions: Patient position is supine lying with knees bent, swing them to one side allowing the hips and lower back to rotate in the same direction. Keep shoulders down. Hold for 10-20 seconds and then repeat on the other side and after repeating each side 10-20seconds.
Wrist Extension Stretch:

Position: Seated
Instructions: Patient position is sitting position, place palms down at your side. Slowly move your hands backward until feeling the stretch. Hold for 60 seconds and then reposition after repeating for 60 seconds.
Wrist and Finger Extension:
(1) Position: Seated

Instructions: Slowly extend the wrist, and hold the palm with the second hand. Continuing to extend the wrist and finger, move one hand towards the fingers. Hold for 60 seconds and then reposition after repeating for 60 seconds.
(2) Position: self stretch
Instructions: Until a feel the stretch, place palms together in front of your face, slowly lower hands, keeping elbows out. Hold for 60 seconds and then reposition after repeating for 60 seconds.
Strengthening Exercise:
Generally, strengthening exercises involve the major muscle groups.
Strengthening the muscles of the stomach and back (‘core’) and arms and legs muscles.
Back strength help to improve balance and posture, which can help with day-to-day activities, such as wheelchair transfers, and reduce the risk of falling.
Avoid ‘eccentric’ activity. Repetitive exercises where the muscle is being lengthened, for example, squats.
Eccentric exercises put greater force on the muscle and can lead to muscle soreness and damage.
Important to improve the endurance of muscles, rather than strengthening or trying to build up muscle bulk.
Examples of muscle-strengthening exercises include:
- cycling
- lifting weights
- climbing stairs
- hill walking
- exercise with resistance bands
- dance
- push-ups, sit-ups, and squats
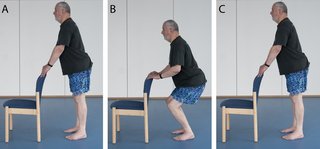
Sit-to-stand:

position: sitting to standing.
Instructions: Patient sits on the edge of the chair, feet, and hip-width apart. Lean slightly forwards, then stand up slowly using your legs, not use your arms. Do not look down, keep looking forward. Stand straight and then slowly sit down, using your hands or arms.
5 repetitions. The slower the repetitions, the better.
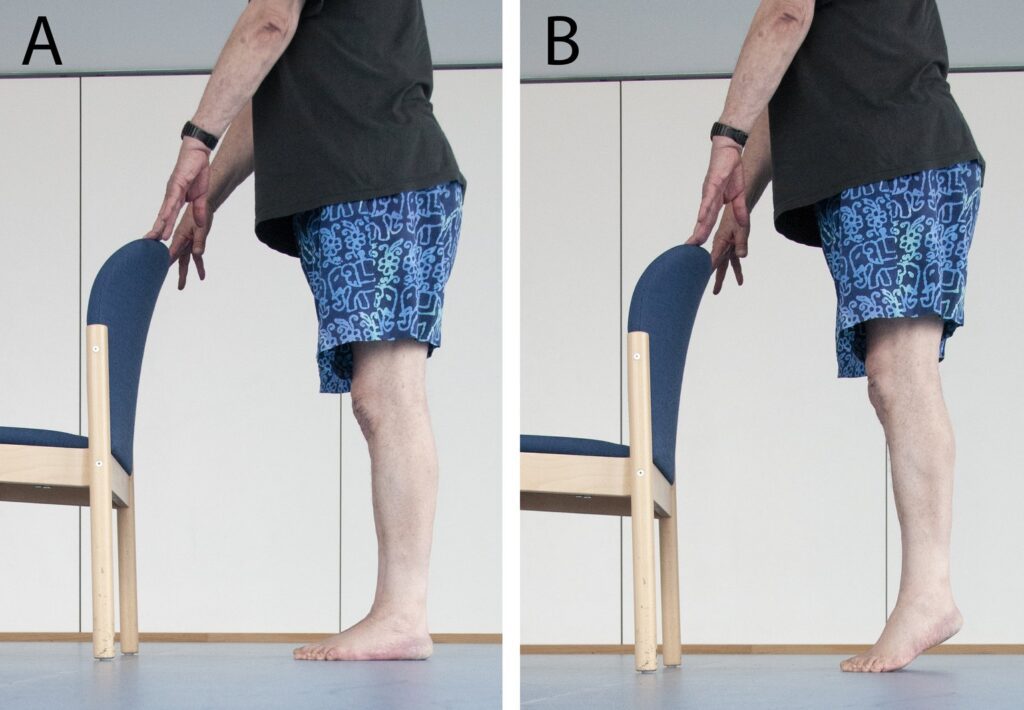
Mini-squats:
Position: stand behind the chair.
Instruction: Rest your hands on the back of the chair for stability and stand with your feet and hip-width apart. Bend your knees slowly as far as possible. Keep facing forward, and aim to get them over your big toe. Keep back straight at all times. Gently come up to standing, clenching (squeezing) buttocks as you do so.
5 repetitions. The slower the repetitions, the better.
Calf raises:
Position: stand behind the chair
Instructions: For stability, rest your hands on the back of a chair. As far as is comfortable, lift both heels off the floor. Perform the exercise without support, to make this more difficult.
5 repetitions. The slower the repetitions, the better.
Sideways leg lift:
Position: stand behind the chair.
Instruction: For stability, rest your hands on the back of a chair. As far as is comfortable, raise your one leg to the side and keep your back and hips straight. Avoid tilting on the right. Back to the starting position and after then raise your right leg to the side as far as possible.
5 repetitions. The slower the repetitions, the better.
Leg extension:

Position: stand behind the chair.
Instructions: For stability, rest your hands on the back of a chair. Standing straight, raise your one leg backward, keeping it straight. When you take your leg back, avoid arching your back . You feel the effort in the back of the bottom and thigh.
5 repetitions. The slower the repetitions, the better.
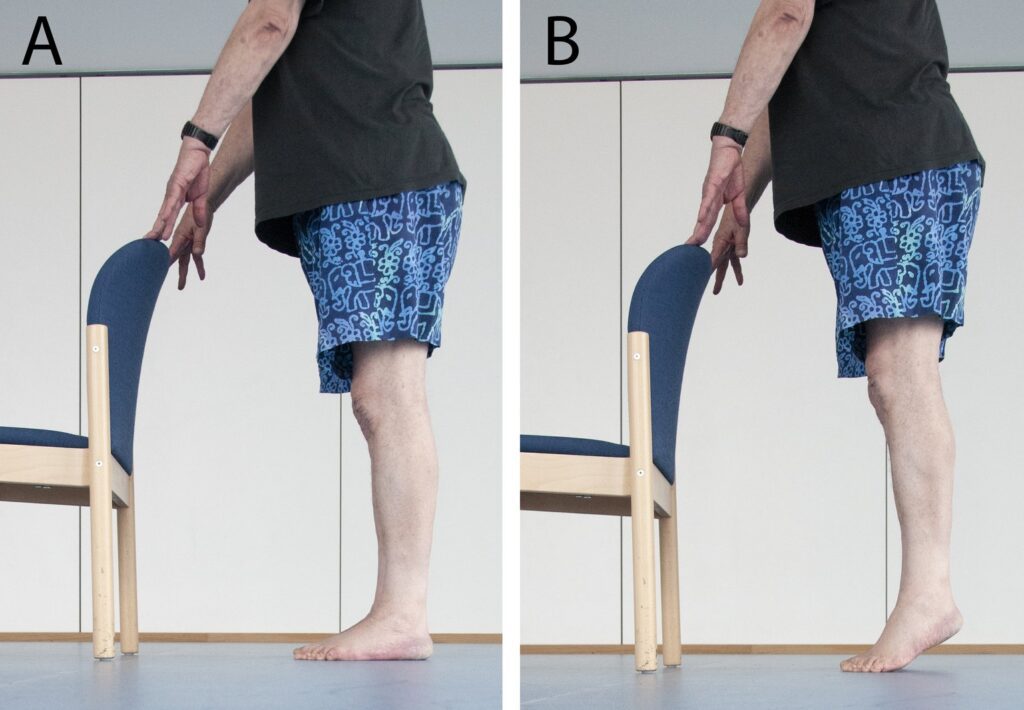
Wall press-up:
Position: stand facing the wall
Instructions: Stand at arm’s length facing the wall. At chest level, place your hands flat against the wall, with fingers pointing upwards. Straight your back, keep your elbows by your side, and slowly bend your arms. As much as you can close the gap between you and the wall.Slowly back to the starting position.
Attempt 3 sets of 5 to 10 repetitions.
Biceps curls:

Position: standing
Instruction: Hold a pair of light weights dumbells (filled water bottles will do) and stand with your feet and hip-width apart.Keeping your arms by your side, slowly bend them until the weight in your hand reaches your shoulder. Slowly lower again.
This can also be carried out while sitting.5 repetitions. The slower the repetitions, the better.
Complications:
As with all treatments, there are adverse effects that should be taken into concern when dealing with the patient.
Examples of known adverse effects are:
- Deformities
- Enduring, gradual improvement including declined mobility and declined capabilities care for self
- Cardiomyopathy
- Congestive heart failure (rare)
- Pneumonia or other respiratory infections.
- Respiratory failure
- Heart arrhythmias (rare)
- Mental impairment (varies, usually minimal)
- Fluid retention and hypertension.
- Weight gain and growth inhibition.
- Osteoporosis with increased risk of vertebral fractures.
- Respiratory Care.
- Impaired fat and glucose metabolism.
- Cushingoid features
- Weight gain and growth inhibition
Respiratory Care:
Routinely checked respiratory function in DMD patients. This allows therapists to check who may need help with assisted coughing and respiration in the future.
Evaluation of respiratory functions include:
- Carbon dioxide levels should also be monitored.
- Maximum inspiratory and expiratory pressure.
- Peak cough flow.
- Spirometric measurements of FEV, FEV, and maximal mid-expiratory flow rate.
Airway clearance is of importance to inhibiting pneumonia and atelectasis. In clinical practice, a variety of manual techniques can be used to clear the patient’s airways.




2 Comments