Ankle pain while walking: Cause, Symptoms, Diagnosis, Treatment, Exercise
There are too many causes of Ankle pain while walking and require proper diagnosis, and according to the diagnosis treatment plans are decided. The doctor will check your history of pain, and also require an imaging study for proper diagnosis. Diagnosis helps to make proper treatment.
In this article, we discuss why Ankle pain occurs while walking, how to diagnose Ankle pain and various treatment option for Ankle pain.
Table of Contents
What is ankle pain while walking
- Ankle joint is one of the most complex, and hard-working regions of the body. It has 26 bones as well as 33 small joints, all held together by a network of soft tissue made up of the muscles, tendons, ligaments, nerves, and blood vessels as well. Most cases of the foot or ankle pain are short-term and are caused by soft tissue injuries, namely sprains or strains. It supports the weight of the body while standing, walking, as well as running. It is quite common for injuries or conditions to affect the ankle and this may cause pain while walking. Ankle pain refers to any type of pain or even discomfort affecting any part of the ankle joint.
- Ankle pain usually gets better with home treatments namely rest, ice, and over-the-counter pain medication. A physiotherapy program can help the patient for strengthening muscles and preventing another injury. Doctors treat more severe pain with the braces and splits, or injections and surgery. Moreover, the most common causes of ankle pain are injury, arthritis, and normal wear, and tear.
- Depending on the cause, the patient may feel pain or stiffness anywhere around the ankle. The patient’s ankle may also swell, and the patient may not be able to put any type of weight on it. Many times, minor conditions can be treated without surgery. However, if the injury is severe, namely a broken ankle bone, or when the ankle pain fails to improve with nonsurgical treatment, surgery is needed. If the patient had an ankle injury or even surgery, a physical therapy (PT) treatment plan can also help the patient to heal. Physiotherapist strengthens the muscles that support the feet as well as ankles. Physical therapy can relieve pain as well as prevent future injuries.
What may cause general ankle pain while walking?
- Some conditions
- Gout
- Gout is one type of arthritis. This condition occurs when uric acid does not dissolve into the blood like it is supposed to. Instead, it crystallizes, accumulates in the joints, and can cause pain. The patient may first notice pain in the big toe which may then move to the ankle, heel, and other joints.
- Osteoarthritis
- Osteoarthritis is the most common form of arthritis of the joints. It is caused by a breakdown of the cartilage in the joints. This may be the cause of the ankle pain, especially, if the patient is older, overweight, or even has previously injured the ankle. Peripheral neuropathy: Damage to the patient’s peripheral nerves and can cause pain in the ankles while walking. Nerve damage can be caused by tumors, trauma, infections, or even disease.
- Injuries
- Ankle injuries can occur during any kind of daily activity, or even just walking. Injuries that most commonly result in ankle pain include:
- Bruising
- If the patient has severely bumped the ankle, namely from a hit or kick, it may cause pain while walking. Basically, pain from this type of trauma will go away in 2 to 3 weeks.
- Sprain or strain
- Sprains, as well as strains, occur from an injury to the softer tissues in the ankle. This injury could be a strained ligament or tendon. Most commonly, a sprain or strain will heal in a few weeks.
- Fractures or breaks
- If a bone is broken or fractured, the patient will likely have intense pain while walking. Breaks are usually accompanied by swelling, redness, or even loss of feeling in the toes. Ankle breaks can take weeks to heal completely and usually require a doctor’s care.
- Achilles tendon rupture
- Typically occurs if the patient is active or participating in a vigorous sport. It occurs when the Achilles tendon is torn or ruptured. It is most likely owing to an injury, namely falling or accidentally stepping into a hole while walking or running on the uneven ground.
- Heel bursitis
- A bursa is a pocket as well as a lubricant that acts as a cushion around the joint. There is a bursa that protects the back of the ankle and heel. It assists to shield the Achilles tendon. It can burst with overuse or even strenuous activity.
- Achilles tendinitis
- Along with the rupture, Achilles tendinitis is caused by an injury to an Achilles tendon. Overuse or even intense strain can cause the band that connects the calf muscle to the heel bone to stretch, resulting in tendinitis.
- Infection
- A previous cut, trauma, or even surgery can allow bacteria to enter the skin or joint around the ankle and cause an infection.
- Plantar fasciitis
- This condition is a band of tissue (fascia) that connects the heel bone to the base of the toes. It supports the arch of the foot as well as absorbs shock while walking. Tension, as well as stress on the fascia, can cause small tears in the joint. Repeated stretching as well as tearing of the facia can irritate or inflame it, even though the cause remains unclear in many cases of plantar fasciitis.
- Pseudogout
- This is a form of arthritis characterized by the sudden, painful swelling in one or more of the joints. This condition can give pain for days or weeks. This condition most commonly affects the ankle and knee joints. It is also called calcium pyrophosphate deposition disease or CPPD, the most common term “pseudogout” was coined for the condition’s similarity to gout. Crystal deposits within the joint cause both conditions, even though the type of crystal differs for each condition. It is not clear why crystals form in the joints and can cause pseudogout. However, the risk increases with age.
- Rheumatoid arthritis
- This condition is a chronic inflammatory disorder that can affect more than just the joints. In some patients, this condition can damage a wide variety of body systems, which includes the skin, eyes, lungs, heart, and blood vessels. An autoimmune disorder, rheumatoid arthritis occurs when the immune system mistakenly attacks the own body’s tissues. Unlike the wear and tear damage of osteoarthritis, rheumatoid arthritis affects the lining of the joints, causing a painful swelling that can eventually result in bone erosion as well as joint deformity. The inflammation associated with rheumatoid arthritis mainly damages other parts of the body as well. Whereas new types of medications have improved treatment options dramatically, even severe rheumatoid arthritis can still cause physical disabilities.
- Septic arthritis
- Septic arthritis is a painful infection in the joint that can come from germs that travel through the bloodstream from another part of the body. Septic arthritis can also occur when a penetrating injury, namely an animal bite or trauma, delivers germs directly into the ankle joint. Infants as well as older adults are most likely to develop septic arthritis. People who have artificial joints also have the risk of septic arthritis.
- Stress fracture
- In this condition, tiny cracks in the bones may occur. It is caused by the repetitive force, often from overuse of the joint as well as bones, namely repeatedly jumping up as well as down or running long distances. Stress fractures can also happen from normal use of the bone that is weakened by a condition such as osteoporosis. This type of fracture is most common in the weight-bearing bones of the lower leg as well as the foot. Track, as well as field athletes and military recruits who carry heavy packs over long distances, are at the highest risk, but anyone can sustain a stress fracture. If you start a new exercise program, for instance, the patient might be developed stress fractures if the patient does activity too much too soon.
- Chronic ankle instability
- Chronic ankle instability occurs when the patient had gone through multiple sprains or other injuries to the ankles. As a result of the injuries to the ankle, the ligaments surrounding the ankle joint, whose job is to keep the ankle stable as well as supported, are weakened. Over time, this can lead to aching as well as pain when the patient is walking, given this is the time that these ligaments must be engaged to assist stop the ankle from rolling. If the patient has unstable ankles, he/she may notice that the pain is worse when he/she do walking over uneven ground.
- Sinus tarsi syndrome
- The sinus tarsi are simply the term for the tunnel between two of the bones just below the ankle, towards the outer side of the foot. Sinus tarsi syndrome describes a situation where damage to the tunnel, or the ligaments, blood vessels, or even nerves in or around the tunnel, may result in some symptoms like pain, burning, tingling or even weakness at the ankle. For treating the sinus tarsi syndrome may involve helping keep the foot supported in an optimal position for the damaged structures to heal.
- Flat Feet – Posterior Tibial Tendon Dysfunction
- When the patient has a flat foot, he/she is naturally more vulnerable to a painful condition called posterior tibial tendon dysfunction (PTTD). The posterior tibial tendon is a tendon that runs down the inside of the lower leg, crossing the inside of the ankle. It plays a large as well as an important role in keeping the patient active and moving. When the tendon is damaged, often from overuse relating to flat, and unsupported feet, the pain is usually felt on the inside of the ankle. Treating PTTD involves assisting heal the damaged tendon to alleviate the ankle pain as well as keeping the flat foot supported so that the flat foot posture does not cause damage to the posterior tibial tendon again in the near future.
- Bunions
- Bunions are essentially a deformity of the big toe in the foot. Patients with bunions have a toe that points outwards and bumps on the inner side of the foot. As a bunion gets bigger as well as calluses form, it can force the patient to shift the weight to avoid pain when the patient will walk.
- Lupus
- This condition is an autoimmune disease that causes the body to attack healthy tissue. Patients with lupus often have joint pain, including ankle pain. This is from lupus-associated arthritis as well as tendinopathy. Moreover, lupus can cause kidney problems that lead to fluid buildup in the joints. There is no cure for lupus, still, the doctor can give medications to the patient to keep it under control. A healthy diet, as well as regular exercise, can also help.
- Chronic lateral ankle pain
- There are various causes for ongoing pain on the outside of the ankle joint. It is most likely because of the ligament which did not heal properly after a sprain and remains weak. This makes the entire joint less stable as well as leads to more injury and pain as well.
- Bursitis
- The ankle has two fluid-filled sacs, called bursa, that cushion the space between the tendons and bones. It can get inflamed from arthritis, overuse, high-heeled shoes, recent footwear changes, or even starting workouts again after time off. The ankle may feel stiff, tender, warm, as well as swollen.
- Osteochondral Lesions of the Talus (OLT)
- A sudden injury like the sprain can damage cartilage on the talus (heel bone) or cause fractures, blisters, or even sores in the bone underneath. The patient might notice a catch in the ankle, or it could lock up or even still hurt months after a treated injury, which could be osteochondral lesions of the talus.
- Reactive arthritis
- This type usually follows an infection in the GI tract or urinary tract. Ankles, as well as knees, are among the first places that may feel it. The doctor will treat the infection with antibiotics. There is no cure for arthritis, but anti-inflammatory drugs can help with pain as well as swelling. Exercise will keep the joints flexible. Arthritis should go away in a few weeks or months.
- Scleroderma
- This group of conditions causes the skin and connective tissues to thicken. When this affects the tissues around the joint, the patient might feel pain and stiffness. It can also weaken the muscles and cause digestive, heart, and kidney problems as well.
- Infection
- If the patient is sick, irritable, and feverish along with the ankle pain, the patient might have an infection. The joint may be swollen, become red, and warm. The doctor may use a needle to remove fluid from the ankle to drain it or test for a cause. The patient may get antibiotics to kill the bacteria.
Symptoms of the ankle pain while walking
- Ankle swelling
- Bruising
- Redness
- Numbness or tingling
- Instability while walking
- Burning pain
- Instability to bear weight on the injured leg
- Stiffness
- Weakness
How to diagnoses the Ankle pain?
- While a physical examination, the doctor will examine the patient’s ankle, foot as well as a lower limb. The doctor will touch the area of the skin around the injury to check for proper points of the tenderness and move the foot of the patient to check the range of motion as well as to know what positions cause discomfort or pain in the ankle.
- If the injury is severe, the doctor may recommend one or more of the following imaging scans to find out a broken bone or even to evaluate in more detail the extent of ligament damage:
- X-ray:-Durning an X-ray, a small amount of radiation passes through the patient’s body to produce images of the bones of the whole ankle joint and surrounding areas. This test is the best for finding bone fractures.
- Magnetic resonance imaging (MRI):-Magnetic resonance imaging mainly uses radio waves and a strong magnetic field to produce detailed cross-sectional or 3-D images of the soft internal tissue of the ankle joint, including ligaments.
- Computed tomography scan(CT scan):– Through computed tomography scans the doctor can get more detail regarding the bones of the ankle joint. CT scan takes X-rays from many angles and mixes them to make cross-sectional or 3-D images.
- Ultrasound(US):– An ultrasound uses sound waves to produce images of the ankle. These images may help the doctor to find out the condition of a ligament/tendon when the foot is in different positions.
Some special tests for ankle pain while walking
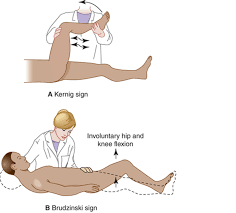
- Anterior Drawer test – to find any injury in anterior talofibular ligament at ankle:
- First of all, the patient is in the supine position, and the ankle joint is 20° of flexion after the heel is resting on the therapist’s palm which is supported on the table. Then, the therapist should stabilize the calcaneus bone. The therapist after that stabilizes the tibia and fibula while drawing the calcaneus, anteriorly observing the amount of anterior translation of the lateral aspect of the ankle and the change in end feel. The amount of anterior translation and the eventual weakening of the end feel, as well as changing from hard ligamentous to weak elastic, is observed. An anterior translation greater than one cm as compared to the normal opposite ankle as well as an evident weakening of the end feel is most indicative of the partial rupture or complete rupture of the anterior talofibular ligament in the ankle.

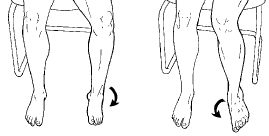
- Talar Tilt test – To find out any injury in the anterior talofibular ligament and the calcaneofibular ligament.
- To begin with, the patient is seated with an unsupported foot as well as an ankle. The position of the foot is ten to twenty degrees of plantarflexion. The distal lower limb is stabilized with 1 hand just proximal to the malleoli, and the hindfoot is inverted with the other hand. The lateral side of the talus is palpated to determine if tilting happens. The laxity is compared to the other side.
- Squeeze test
- To embark with, the squeeze test compresses the proximal fibula opposite to the tibia to assess the integrity of the bones, interosseous membrane, as well as syndesmotic ligaments. Pain happens with fracture or diastasis and is considered positive.
- Kleiger’s test or external rotation test
- First of all, the patient is in a seated position, with the knee hanging to 90 degrees, and the ankle is relaxed. After, the examiner should sit at the level of the ankle to be tested with a strong hand stabilizing the leg from behind, and the other hand grasps the ankle in a normal position and then do an external rotation of the foot. If there is pain at the site of the interosseous membrane, or even medically. Pain may radiate upward to the leg depending on the severity of the injury and affection the test is positive.

- Impingement sign ankle
- To begin with, the examiner faces the patient in a seated position. The examiner holds the calcaneus bone with the hand on the lateral side of the foot, fingers around the calcaneal tuberosity, and thumb over the anterolateral portion of the ankle joint. The medial hand grasps the forefoot as well. Basically, the foot is held in the plantarflexion. While pressure is applied with the examining thumb, the foot is brought from the plantarflexed position to full dorsiflexion. If the pain reproduced from combined movement with thumb pressure and pain is greater in dorsiflexion as compared to plantarflexion then the test is positive. If Pain is not improved with the combined movement then a test is negative.
- Cotton Test
- This test is performed to detect syndesmotic instability of the joint. This is a manual stress test, it identifies the amount of the lateral translation of the talus bone within the ankle mortise. The clinician stabilizes the proximal ankle while shifting the talus bone laterally. The positive test is marked by increased movements relative to the healthy side and is indicative of a sprain of the distal tibiofibular syndesmosis or even the subtalar joint.
- Coleman block test
- By this test, the therapist can evaluate hindfoot flexibility as well as pronation of the forefoot.
- To begin with, the initial deformity is in the forefoot followed by the subsequent changes in the hindfoot. The test is performed by placing the foot of the patient on a woodblock, 2.5-4 cm thick, with the heel as well as lateral border of the foot on the block and bearing full body weight while the first, second, & third metatarsals are allowed to hang freely into plantarflexion motion and pronation motion. The test result is based on premise that there is fixed flexion of the first metatarsal. This test negates the effect that the forefoot (1stmetatarsal in plantar flexion) may have on the hindfoot in the stance phase. If heel varus is correct during the patient is in standing on the block, the hindfoot is considered flexible, if the subtalar joint is supple and correct Coleman block test, then surgical procedures might be directed to correcting forefoot pronation, that is usually because of plantarflexion of the first metatarsal. if the hindfoot is rigid, after that surgical correction of both forefoot and hindfoot is required

Coleman block test
- The Eversion Stress Test
- The eversion stress test evaluates the integrity of the deltoid ligament as well as aids in determining the degree of instability after the medial ankle sprain.
- First of all, the patient is in the supine position, side-lying, or seated comfortably with the knee at 90 degrees of flexion, and the gastrocnemius muscle should be relaxed. The heel is held from below by one hand by the physiotherapist while the opposite hand holds the lower leg. While maintaining the ankle in a normal position, the clinician applies an abduction force to the calcaneus bone to tilt the talus. Increased talar tilt or even pain over the deltoid ligament, when compared bilaterally, indicates a positive test. A spongy or even indefinite end feel is indicative of a complete tear. In the normal position, a 2-degree or greater tilt while testing when compared bilaterally indicates a high probability of significant injury to the deltoid ligament.
- The navicular drop Test (NDT)
- First of all, tell the patient to take a standing position so there is full weight-bearing through the lower extremity as well as ensure the foot is in the subtalar joint normal position. Mark the most prominent area of the navicular tuberosity as well as to measure its distance from the supporting surface (floor or even step). Ask the patient to relax and after that measure the amount of sagittal plane excursion of the navicular with a ruler. Alternatively, the test can also be performed in reverse action, for example measuring from a relaxed position up to talar normal in a standing position. Many examiners also choose to perform this test by marking the start as well as end position of the navicular on an index card placed along with the inside of the foot and after that measuring the change with a ruler.
- Posterior drawer test
- This test of the ankle is used to test for posterior talofibular ligament injury and ligamentous instability of the ankle joint.
- First of all, tell the patient to lie supine with the knee slightly flexed to neutralize the pull of the gastrocnemius muscle of the lower limb. With the ankle joint held at 10 to 15 degrees of plantar flexion, the therapist grasps around the heel with one hand and stabilizes the tibia bone from the anterior side with the other. After that ask the patient to relax the muscles, and the examiner moves the foot posteriorly at the ankle joint while continuing to hold the tibia bone with the other hand.
- Positive test: If the absence of an end-feel, as well as the proximal tibia, falls back (excessive translation). The amount of posterior motion determines the grade of PCL tear.
Gait cycle
- The gait cycle is the time interval between the two successive occurrences of one of the repetitive events of locomotion. The human gait cycle is divided into two separate regions representing the period of time when the foot is in contact with the floor, which is known as the stance phase, and the period of time when the lower limb is not in contact with the floor, which is known as the swing phase.
- In the time of the stance phase, the foot contacts the floor, the mass of the body is supported, and after that, the body is propelled forward during the later stages of stance. The stance phase has five events: 1) heel-strike (HS), 2) foot-flat (FF), 3)midstance (MS), 4) heel-off (HO), and 5)toe-off (TO).
- Heel-strike: The beginning instant of the human gait cycle is represented as initial contact of one foot with the floor, usually termed heel strike or foot-strike.
- Foot-flat: The instant that the rest of the foot comes down in contact with the floor and usually is where full body weight is being supported by the lower leg.
- Midstance: This phase is defined when the center of mass is directly above the ankle joint center. It is also used as the instant when the hip joint center is above the ankle joint.
- Heel-off: Heel-off happens when the heel begins to lift off the floor in preparation for the forward propulsion of the body.
- Toe-off: Toe-off occurs as the last event of contact during the stance phase.
- Various events of the gait cycle remarkably happen in similar sequences as well as are independent of time. That is why the gait cycle is commonly described in terms of percentage, instead of the time elapsed. The initial heel strike is designated as 0% and the subsequent heel strike of the same foot is 100% (0–100%). During the normal gait cycle, hip, knee, and ankle joints experience the range of motion. Illustrates these ranges of movement during different speeds. Hip motion can be categorized into two basic movements: first, hip extension, which occurs during the stance phase and it has the primary role of stabilization of the trunk, and, second, hip flexion, which occurs during the swing phase. While the stance phase, the knee is the basic determinant of the lower limb stability, and in the swing phase, knee flexibility is the primary factor in the freedom of the limb to advance. At midstance, total body weight is transferred into the flexed knee. The range of movement of the ankle is not large, still, it is critical for progression as well as shock absorption during stance.
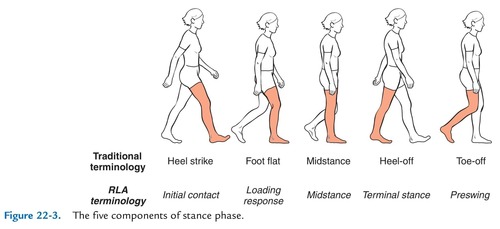
- Periods and phases of gait
- A human gait cycle embarks when one foot makes contact with the floor and ends when that same foot contacts the floor again. The gait cycle can be broken down into periods as well as phases to determine normal and abnormal gait.
- Most frequently, the gait cycle is split into two periods, the stance and the swing. The stance phase is the time during which the foot is in contact with the floor. The swing phase follows the stance phase and it is the time during which the same foot is in the air. The separation of the two phases is discerned by the toe-off. If one considers the location of the other or contralateral foot, then the stance period can be further split into three subperiods. The initial double-leg support is the subperiod during which both feet are in contact with the floor. The single-leg support is the subperiod during which the other or contralateral foot is in the air. The terminal double-leg support is the subperiod during which both the feet are again in contact with the floor. Basically, the stance period represents the first 60% of the gait cycle and the swing the latter 40%. The initial double-leg support represents the initial 10% of the gait cycle, the single-leg support represents the 40%, and the terminal double-leg support concludes the stance phase with another 10% of the gait cycle. The duration of successive periods of stance, swing, and double support are similar while the same walking trail as well as during repeated trials of the same subject. However, speed can affect the percentages with respect to the subperiods of stance, where improvement in speed will reduce the double-leg support subperiods as well as increase single-leg support. Eventually, if the person keeps moving faster and starts running, the double-leg support subperiods will disappear. On the opposite side, reduces in walking speed will have the exact opposite effect.
- The gait cycle can also be divided according to functional phases by Inman, Ralston, & Todd, 1981; Levine et al., 2012; Perry and Burnfield, 2010; Rose and Gamble, 2005). From this approach, the following phases are noted:
- Initial contact (0%–2% of the gait cycle): This phase is the start of the loading response or of the weight acceptance. It is also the starting of the stance phase as well as the first part of the initial double-leg support period. During the initial contact phase, a person will also have the presence of any impact phenomena presented very early in the floor reaction forces.
- Loading response (2%–12% of the gait cycle): This phase is the rest of the initial double-leg support phase. While this phase, a person continues as well as completes the task of weight acceptance. In terms of the anterior-posterior force, a person has the minimum (or maximum) braking peak.
- Midstance (12%–31% of the gait cycle): Midstance is the first part of the single-leg support period. Stability is the major concern as the base of support will reduce significantly as well as the center of gravity(COG) will move to its highest point through leg extension and kinetic energy transfers to the potential energy. The end of this period is distinguished by the occurrence of the “valley” or even the local minimum of the vertical floor reaction force.
- Terminal stance (31%–50% of the gait cycle): Terminal stance is the second part of the single-leg support period. Stability is still the concern and the heel strike of the other foot. The center of gravity(COG)“falls” from its highest point as well as potential energy transfers to the kinetic energy.
- Preswing (50%–60% of the gait cycle): It is the terminal double-leg support period as well as it is our second loading period. In terms of the vertical ground reaction force(VGRF), a person has the occurrence of the second loading peak or even the second local maximum or the second “hump.” During this phase time, a person also has our maximum propulsion peak in the words of the anterior-posterior force as a person prepares to propel our foot off the floor.
- Initial swing (60%–73% of the gait cycle): This phase is the first part of the swing period, as well as our major concern, is to clear the ground by flexing the entire leg. The overall flexion reduces the moment of the leg of inertia as well as increases the angular velocity of the swinging leg.
- Midswing (74%–87% of the gait cycle): This phase is the second part of the swing period, as well as our major concern, is that the opposite or contralateral leg is in single support with a small base of support thus stability is the concern. A person is also getting ready for the upcoming foot contact at the end of our swing.
- Terminal swing (85%–100% of the gait cycle): This phase is the third and last phase of the swing period, as well as our major concern, is our upcoming foot contact.
Treatment
Medical treatment
- In most cases of ankle pain even though mild or severe painful condition, pain relievers are used, such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve, others), or acetaminophen (Tylenol, others).
Physiotherapy treatment
Electrical modalities
- This type of therapeutic modality helps the patient for Reducing ankle pain, alleviate nerve pain, accelerate healing of musculoskeletal injuries, increase blood circulation in the body, heal wounds, and relax muscle spasms.
- Ultrasound(US): The US is mainly used for the tender points to reduce pain.
- Transcutaneous electrical nerve stimulation(TENS): This modality is used for pain relief, reducing redness, and for the reduction of swelling.
- Wax therapy: This method mainly helps the patient with the reduction of pain.
Exercises
- Daily one or two sessions of exercises may help the patient to relieve pain and strengthen the muscles.
Stretching exercise:-
- In the starting phase do some stretching exercises. It may improve the performance in physical activities, decrease the risk of injuries, help the joints move through their full range of motion, increase muscle blood flow, enable the muscles to work most effectively, and improve the ability to do daily activities.
- Achilles tendon and plantar fascia stretch
- To begin with, tell the patient to take a loop of the towel around the ball of the foot and pull back towards the body, during this the knees should be straight. Hold for 30 seconds in one repetition, do three repetitions in one session. Do three sessions per set.

- Sitting plantar fascia stretching exercise
- First of all, tell the patient to cross the foot over the contralateral knee, and the base of the toes put on the floor and gently pull back until the patient feels a stretch along the underside of the foot. Hold for 30 seconds per repetition. Repeat three times in one session and do three sessions per set. Do two sets per day.
- Standing calf stretch
- The patient must stand facing the wall and then put both hands on the wall which is in front of the patient. Place one foot anterior to the opposite foot with the anterior foot about 30cm away from the wall, and keep the back knee straight with the back heel flat on the ground. Slowly bend the front knee till the patient can feel the stretch in the calf of the back lower leg, after holding for thirty seconds return to normal position, repeat three times per session. Do three sessions per day.
- Deep calf stretch
- The patient must stand on the step with the heel hanging off the edge. The patient may allow holding onto something for support, then allow the patient heels to drop towards the ground and feel the stretch in the calf muscles and Achilles tendon. Hold this position for 30 seconds. Repeat this exercise 3 times in one session. Do three sessions per day.
- To do an inward towel stretching exercise:
- First of all, tell the patient to sit with the towel or band around the affected foot. Then, hold each end of the towel with the patient’s hands. Slowly turn the ankle inward, like the patient is facing the sole of the foot to the opposite. After that, pull up with the unaffected hand side of the towel to deepen the stretch. Repeat on the other side of the patient has a problem. Hold for thirty seconds per repetition. do three repetitions per session in one set. Do three sessions per day.
- To do an outward towel stretching exercise:
- To begin with, ask the patient to sit with a towel or even a band around the affected foot. Then, hold each end of the towel with the patient’s hands. This time, slowly turn the ankle outward, like the patient is facing the sole of the foot to the affected foot. After that pull up with the left-hand side of the towel to deepen the stretch. Repeat on the other side too if any tightness is present. Try to hold these stretches for 30 seconds and repeat them three times in one session. Do three sessions per day.
- Standing calf stretch to dial up the tension in the stretch, the patient can move to the standing position:
- To embark, stand facing a wall or other support, like a chair, with one foot in front of the patient by around 12 inches.
Point the toes up. Slowly lean forward until the patient feels the stretch in the back of the lower leg. Hold this stretch for thirty seconds and after that repeat on the other side too if any tightness is present. Do 3 rounds total. - Cross leg ankle stretch
- First of all, tell the patient to sit comfortably with the left leg crossed over the right knee. Then, hold the right foot with the hands, after that use the right hand to bend the left toes as well as ankle downward like the patient is pointing the toes. The patient should feel this stretch on the front of the ankle and the foot. Hold this stretch for 30 seconds and repeat on the other side too. Repeat three times per session in one set. Do two sessions and two sets per day.

- Chair Pose
- To begin with, stand tall in the tadasana position. Inhale as the patient raise both of the arms overhead, palms inward. As the patient exhales, bend both of the knees slightly, working toward getting the thighs parallel with the floor. The torso should make the right angle with the tops of the thighs. Try holding this pose for 30 seconds to 60 seconds. To come out of it, inhale and straighten the knees. Do three repetitions per session. Do three sessions per day.
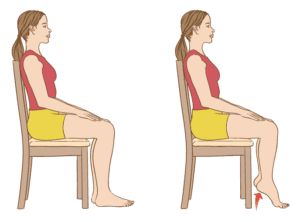
- Seated foot as well as heel raise exercise
- To embark with, the feet flat on the ground. Raise both heels off the floor as well as hold for thirty seconds before placing the heels back on the ground. After that, raise the toes off the ground and hold them for thirty seconds before returning them to the ground. Repeat three times per session. Do three sessions per day.
- Toe bend stretching exercise
- First of all, tell the patient to place the heels on the ground with the toes pointing in the air in front of the patient. Bend the toes downwards and hold for thirty seconds, then relax. Next, bend the toes upwards and hold for thirty seconds before relaxing. Repeat three times per session. Do three sessions per set in one day.
- Toe raise, point, and curl
- Toe raise, point, and curl exercise have three steps and it will help strengthen all parts of the feet as well as toes.
To do this exercise: The patient should sit up straight in the chair, with the feet flat on the ground. Then, keeping the toes on the ground, raise the heels. Stop when only the balls of the feet remain on the floor. Hold this position for ten seconds before lowering the heels down. For the next stage, raise the heels as well as point the toes so that only the tips of the big, as well as second toes, are touching the ground. Hold for ten seconds before lowering the heel down. For the last stage, raise the heels as well as curl the toes inward so that only the tips of the toes are touching the ground. Hold this position for ten seconds. Build flexibility as well as mobility by repeating each stage ten times per session in one day. - Big toe stretch
- Keeping a wide range of movement in the big toe is essential. The big toe stretch exercise also has three steps and it is designed to stretch as well as relieve pain in the toes from wearing tight shoes.
To do this exercise: Tell the patient to sit up straight in the chair, with the feet flat on the ground. Bring the left (affected) foot to rest on the right thigh. Using the fingers, gently do stretching of the big toe up, down, as well as to the side. Keep the big toe in each position for thirty seconds. Repeat this exercise three times in one session before switching to the other foot. Do three sessions per day.

- Toe splay
- First of all, doing the toe splay exercise can improve control over the toe muscles. The patient can do it on both feet at once or even on alternate feet, it totally depends on which the patient finds more comfortable.
To do this exercise: the therapist should give the command to the patient to sit in a straight-backed chair, with the feet gently resting on the ground. Spread the toes apart as long as possible without straining. Hold this position for thirty seconds. Repeat this exercise or motion three times per session. Do three sessions per day. Once an individual has built up their strength, he/she can try looping a rubber band around the toes. This will provide resistance and make the exercise more challenging in a later stage. - Golf ball roll stretching exercise
- Rolling a golf ball under the foot may help the patient to relieve discomfort in the arch as well as ease pain associated with plantar fasciitis. To do this exercise: Ask the patient to take a sitting up straight in the chair position, with the feet flat on the ground. After that, place a golf ball or another small, or even hardball on the ground next to the feet. Lay one foot on the ball as well as move it around, pressing down as hard as is comfortable. The ball should be massaging the bottom of the affected foot. Continue for thirty seconds, then repeat using the other foot too if any tightness is present. A frozen bottle of water may be a soothing alternative if there are no suitable balls are available. Do this exercise three times per session. Do three sessions per day.
- Ankle Stretch exercise
- Place one end of the sports cord over the right foot at the instep (not the tip of the shoe). Extend the right leg as well as pull up the Sportcord until the patient has the desired resistance as well as difficulty. Extend the right toe downward, as if the patient is pressing on the gas pedal in the car. Hold extended for ten seconds, and then repeat ten times. Switch legs as well as repeat with the left foot too.
- Finger flexors stretching exercise
- First of all, tell the patient to take a relaxed position like supine on the bed. Then, the physiotherapist tells the patient to take a deep breath and then release it, after that the therapist does finger extension movement passively means the examiner moves the finger of the foot towards the face side and holds it at the endpoint for the next 30 seconds. Do it three times per session. Do two sessions per day.
- Finger extensors stretching exercise
- To begin with, tell the patient to take a relaxed position like lying on the bed. After that, the examiner tells the patient to take a deep breath and release it, after that the physiotherapist does finger flexion movement passively means the examiner moves the fingers of the foot away from the face and holds it at the endpoint for 30 seconds. Do it 3 times per session. Do three sessions per day.
Range of motion exercise
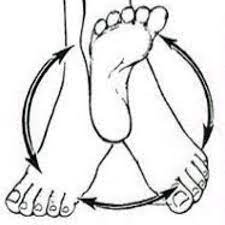
- Ankle circles range of motion exercise
- Ankle circles may help with the range of motion. The patient can do ankle circles from either a sitting or lying position: to embark by turning the ankle around slowly in circles to the left, then the right side. The patient may even find it easier to try drawing the alphabet in the air with the foot. Lead with the big toe. Keep the motions small and focus on only using the foot as well as the ankle, not the entire leg. For circles, try doing twenty in each direction with each foot. If the patient is doing the alphabet, complete 2 sets of this exercise on each foot. After 5 to 6 days, increase the repetitions in every session.
- Toe extension
- This exercise is useful in preventing or even treating plantar fasciitis, which is a condition that causes pain in the heel when walking as well as difficulty raising the toes.
- To do this exercise: Tell the patient to take a sit-up straight in the chair, with the feet flat on the ground. After that, place the affected foot on the unaffected thigh. Then, pull the toes up toward the ankle. There should be a stretching feeling along with the bottom of the foot as well as the heel cord. Hold for thirty seconds. Massaging the arch of the foot during stretching will help ease tension as well as pain. Repeat the toe extension exercise three times on each foot. Do three repetitions per session. Do three sessions per day.
- Toe flexion
- To do this exercise:
- First of all, tell the patient to take a sit-up straight in the chair, with the feet flat on the ground. Then, place the left foot on the right thigh. After that, move the toes down toward the ankle. Then, hold for thirty seconds after that release it. Do three repetitions per session. Do three sessions per day.
- Ankle flexion(dorsiflexion) range of motion exercise
- To begin with, tell the patient to take a relaxed position like lying on the bed. Then, the therapist should give the command to the patient to bend the foot toward the face side means upward as far as the patient can. At the endpoint, the hold should not be taken. Repeat 10 times in one session. Do three sessions per day. As the muscles become strong increase the number of repetitions from ten to fifteen and twenty in one session.
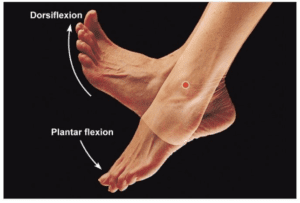
- Ankle extension(plantarflexion) range of motion exercise
- To embark with, tell the patient to take a relaxed position like supine on the bed. After that, the physiotherapist should give the command to a patient to move the foot away from the body means down as long as the patient can but at the endpoint, the hold should not be taken. Repeat ten times per session in one set. Do 3 sessions per day. As the muscles become strong improve the number of repetitions from 10 to 15 and twenty in one session.
- Ankle inversion range of motion exercise
- To begin with, tell the patient to take a relaxed position like lying on the bed. After that, the therapist should give the command to the patient to move the foot inside as far as the patient can, but at the endpoint, a hold should not be taken. Repeat 10 times in one session in one set. Do three sessions in one day. As the muscles become strong improve the number of repetitions from 10 to 15 and 20 in one session.
- Ankle eversion range of motion exercise
- To embark with, tell a patient to take a relaxed position like supine on the bed. After that, the physiotherapist should give the command to a patient to move the foot outside as far as the patient can, but at the endpoint, the hold should not be taken. Repeat ten times per session in one set. Do 3 sessions in one day. As the muscles become strong increase the number of repetitions from ten to fifteen and twenty in one session.
- Alphabet
- First of all, draw the letters of the alphabet in the air by imaging with the foot. Do lowercase as well as uppercase letters, and make sure to move from the ankle, not from the hip joint. Do ten times per session but do not hold at the endpoint. Do three sessions per day.
- Finger flexion range of motion exercise
- First of all, tell the patient to take a relaxed position like lying on the bed. After that, the therapist should give the command to the patient to move her/his fingers down but the therapist makes sure that the patient should not hold this position at the endpoint and after that release it. Do it ten times per session. Do three sessions per day. When the patient is able to do this exercise increases the repetition from 10 to 15 to 20.
- Finger extension range of motion exercise
- To begin with, tell the patient to take a relaxed position like supine. After that, the physiotherapist should give the command to a patient to move the fingers up but the physiotherapist makes sure that a patient should not hold this position at the endpoint and then release it. Do 10 times per session. Do 3 sessions per day. When a patient is able to do this exercise increase the repetitions from ten to twenty to thirty.
Strengthening exercise
- Towel pickup exercise
- First of all, place a towel on the ground in front of the chair. After that, tell the patient that with the heel on the floor, try to pick up the towel by grabbing it with the toes. Repeat this exercise ten times per session. Do three sessions per day. This exercise becomes more challenging by adding a small weight to the towel. When the patient is able to pick up the towel ten times, increase the number of repetitions by 10 to 15 to 20.

- Big toe lift and hold
- To begin with, the therapist should give the command to the patient that with the feet on the ground, lift only the big toe while keeping the other toes on the ground. Hold this for thirty seconds and then relax. Repeat this exercise three times per session. Do three sessions per day.
- Toe curls
- Doing toe curls exercise to build up the flexor muscles of the toes as well as feet, which improves the overall strength.
- To do this exercise:
The therapist should tell the patient to sit up straight in a chair, with the feet flat on the ground. Lay a small towel on the ground in front of the body, with the short side facing the feet. Place the toes of the affected foot on the short side of the towel. Try to grasp the towel between the toes as well as pull it toward oneself. Repeat this exercise ten times before switching to the other foot. To make this exercise harder, try weighing down the opposite end of the towel with the weight cuff. - Marble pickup
- Doing the marble pickup may increase strength in the muscles on the undersides of the feet as well as toes.
- To do this exercise:
To begin with, tell the patient to sit up straight in a chair, with the feet flat on the ground. Place an empty bowl as well as a bowl of around ten to twenty marbles on the floor in front of the patient’s feet. Using only the toes of the affected foot, tell the patient to pick up each marble as well as place it in the empty bowl. Repeat this exercise using the other foot too. Do this exercise ten times per session. Do three sessions per day. When the patient is comfortable and easily dop this exercise increase the repetitions from 10 to 20.
- Heel Raises
- First of all, this exercise can be performed at home as well as at the clinic, what the patient should do is stand near a wall or chair that the patient can balance against. Slowly raise the left foot back until the lower leg is at a 90-degree angle. Hold for ten seconds, and return to the starting position. Repeat five times with each leg.
- Ankle Rotations
- Raise the foot about 20 inches off the ground. After that, with the toe upward, rotate the foot to the left and then back to the right. Hold for ten seconds then return to a starting position. Repeat ten times for each leg in one session. Do three sessions per day.
- The calf raise strengthening exercise
- This is an easy one where all the patients have to do is stand on their toes for ten seconds with both the feet planted firmly in place before slowly lowering back down again on the ground. Repeat it ten times or more if needed.
- Foot dorsiflexion
- To perform this move lie down flat on the back with the hands behind the head. Slowly bend only at the knee (with keeping them straight) until the knees are over the top of their respective knees while keeping both the feet flat on the floor. Slowly straighten the knees back to their original position as well as repeat this exercise 10 times or more if needed.
- Toe pick-ups
- This exercise may help to strengthen the toes as well as improve flexibility. The motion of the toes is directed by the complex set of the muscles (primarily the flexor digitorum brevis as well as extensor digitorum brevis muscles) that are easily impaired with the foot or ankle injury.
- To begin with:
- Place a pile of 20 small objects on the ground (like jacks, hard candies, or even tiny stones). Use the toes to pick them up as well as move them to another pile. Do 3 sessions with three sets of this exercise two times per day.
- Toe Raises
- This exercise may help to strengthen the toes as well as calf muscles.
- To do this exercise:
- Tell the patient to Hold a wall or counter for balance. After that, rise up onto the tiptoes as far as the patient can go without pain. Hold the position for the next 10 seconds, maintaining the tension, then release it. In the starting phase do three sets of ten exercises, and work the way up to three sets of thirty exercises. As the patient gets stronger, he/she can begin to do single-leg toe raises, which place additional weight on the affected leg.
- Ice bottle massage exercise
- This is the best exercise for cooling down (literally). The patient would need to prepare by filling a plastic bottle with water as well as freezing it overnight.
- To round out the exercise routine:
- Tell the patient to place the frozen water bottle on the ground. After that, roll the foot over it for one to two minutes three times per day. Always keep the foot moving, but do not stop and let the bottle rest on a single spot. If the cold causes discomfort, the patient can place a kitchen towel between the bottle as well as the foot. If there is pain or even a prickly sensation, stop as well as avoid this exercise.

- Seated foot as well as heel raise
- To embark with, the patient’s feet are flat on the ground. Raise both the heels off the ground then hold for ten seconds before placing the heels back on the floor. Then, raise the toes off the ground and hold for ten seconds before coming back to the ground. Repeat ten times.
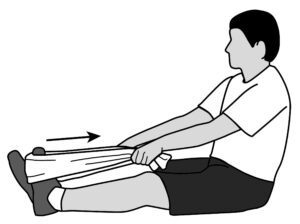
- Ankle flexors strengthening with the theraband
- First of all, tell the patient to sit on the chair as well as tie the theraband around a stable surface that would not move, like a heavy table. Extend the lower leg as well as wrap the other end of the band around the top of the foot. Do flexion of the foot, with the band resisting the motion. Hold for 10 seconds. Repeat ten times per session. Do three sessions per day for strengthening. After 5 to 6 days increase the weight from 500 gm to 1 kg and also increase repetitions.

- Ankle extensors strengthen with the theraband
- To begin with, tell the patient to sit on a chair. After that, take one side of the theraband in each hand, wrap it around the ball of the injured foot, and stretch the leg out in front of you. Then, extend the foot away from the face. Hold this position for the next 10 seconds. Repeat 10 times in one session. Do three sessions per day.
- Ankle invertors strengthen with the use of the theraband
- First of all, tie the theraband around the leg of the chair or even with the table on the same side of the injured foot. Then, wrap the other end of theraband around the inside of the affected foot. After that, try to turn the foot inside. Hold this position for the next ten seconds. Do this exercise 10 times in one session. Do three sessions per day. When the patient is adapted to the 500gm weight, increase weight to 1 kg as well as increase the repetitions.

- Ankle eversors strengthening exercise with the use of the theraband
- To begin with, tie the theraband on the leg of the chair opposite to the affected foot. After that, wrap the other end around the outside of the affected foot. Then, the therapist should give the command to the patient, try to turn the foot outside, and hold for ten seconds, repeat this exercise 10 times in one session. Do three sessions and three sets per day. When the patient is adapted to the 500gm weight, increase the weight to 1kg as well as increase the repetitions.
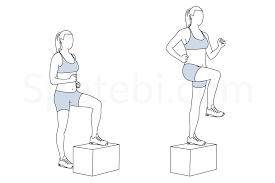
- Step-ups
- To embark with, the affected foot on the bottom stair and the good foot on the floor. Straighten the knee so he/she can lift himself up on the affected leg, then put it down. Repeat this exercise ten times in one session, minimally 3 sessions and three-set a day. When the patient is comfortable with the low repetition, then increase the number of repetitions.
- Sand walking
- Walking barefoot on sand is a great way to stretch as well as strengthen the feet as well as calves. This is a good exercise in general because the soft texture of the sand makes walking more physically demanding.
- To do this exercise:
- Head to a beach, a desert, a volleyball court, or even any other location with sand. Remove the shoes as well as socks. In the starting phase do three rounds on the sand, after 5 to 6 days increase the rounds to six.
Home remedies for ankle pain while walking
- Rest: First of all, try to avoid putting weight on the affected foot or ankle. Do not exercise while this time, instead try gently moving the affected part from time to time to stop the area from getting stiff.
- Ice: Place an ice pack or frozen vegetables, covered in a damp cloth, on the painful(affected) area for ten minutes every two to three hours.
- Compression: Wrap a crepe bandage around the affected part. It should be tight enough to support the affected part, but not so tight that it restricts the blood flow. If the bandage is hurt the toe place a small piece of cotton wool between the skin and bandage and the next toe, then tape them together.
- Elevation: Elevate the foot to reduce swelling.
- Supportive footwear: Make sure the shoes provide adequate support for the feet as well as ankles. Avoid flip-flops, sandals, or shoes that are too loose. It is especially important to wear proper footwear when playing sports. Activities namely, basketball as well as volleyball can lead to ankle injuries, especially without the correct footwear.