Horner syndrome:
Table of Contents
Overview:
Horner’s syndrome is known as a Oculosympathetic paresis. Another name of this condition are Bernard-Horner syndrome and Von Passow Syndrome. Horner’s syndrome or oculosympathetic paresis is results from an disturbance of the sympathetic nerve supply to the eye and symptoms are arise when the group of nerve are damaged or sympathetic trunk is damaged. The Bernard-Horner syndrome is common in France. Von Passow syndrome is an associate with Horner syndrome of iris heterochromia.
Horner syndrome is a condition that affects the eye and surrounding tissue on one side of the face and resulting the paralysis of some nerves. It is caused by the disturbance of a nerve pathway from the brain to the head and neck. Signs and symptoms of Horner syndrome are irregular pupil size(Miosis), a drooping eyelid (Ptosis) and lack of perspiration, apparent enophthalmos on the affected side of the face.
What is Horner’s syndrome?
This syndrome is described by the Swiss ophthalmologist Johann Friedrich Horner in 1869.
Horner’s syndrome known as another term is occulosympathetic paresis. It is a affects the eyes and one part of the face. It happens due to a disturbance of the sympathetic nerve pathway and it connect the brain stem to the eyes and face. The sympathetic nerves controls involuntary functions of the eye, like dilation and constriction of the pupils of the eye and perspiration.
Usually, Horner’s syndrome is seen only one side of the face. This syndrome can occur in both female and male or any age group of people. It may affect races and ethnic persons. Ptosis, Miosis and Anhidrosis three major sign seen in this condition is known as the triad symptom.
Horner syndrome is occur by the result of another medical problem, like a brain stroke, tumour or spinal cord injury. In some cases, no any underlying cause can be found. The symptoms of this condition are not dangerous, but they can indicate a serious health problems. There is no specific treatment for Horner syndrome, but treatment for the related cause can restore nerve function.
Ratio of this condition About 1 in 6,250 babies are born with Horner syndrome.
Inheritance of this syndrome:
Horner syndrome is not inherited. It occurs in individuals with no history of the disorder in their family. The Acquired Horner syndrome and the congenital Horner syndrome have nongenetic causes. In rare cases congenital Horner syndrome is passed within a family in a pattern that seen it autosomal dominant, which means one altered gene present in each cell and that is sufficient to cause the disorder.
What are the causes of horner syndrome?
Horner’s syndrome is also be congenital (By birth) or iatrogenic (Happen due to any medical treatment). In some cases, This syndrome may be the happen of repeated minor head trauma. Although most causes are relatively benign, Horner’s syndrome is become a serious disease in the neck or chest.
Congenital: Horner’s syndrome is present in babies by birth is known as a congenital horner’s syndrome. it present in a some percentage of the population. It present birth time due to any type of birth trauma, injury to the nerves or carotid artery during delivery. It may be caused by a tumor. If the syndrome is present in babies from birth to 2 years of child, the iris may be lighter on the affected side.
Acquired: there are many different conditions that may result in Horner’s syndrome. It affects the neck, chest, and lungs. The disruption of the blood supply to the brain may give the symptoms.
Some of the many conditions that may produce Horner’s syndrome including:
- Trauma to the neck or head.
- Infections.
- Tumour at the top of the lung.
- Lung cancer.
- Thyroid tumour.
- Migraines or cluster headaches.
- Cerebrovascular — interruption of the blood flow to the brain caused by a stroke, aneurysm, or blood clot (embolism).
- Cancerous (malignant) or noncancerous (benign) lesion or tumour on the cervical nerves on one side of the body (very rare).
- Surgery.
The general cause of Horner’s syndrome is damage to the nerve pathway from the brain to the face and it’s called the sympathetic nervous system. The sympathetic nervous system regulates many things including pupil size, heart rate, blood pressure, sweat, and others. The exact cause of this syndrome is unknown.
There are three different section of this pathway and it’s called neurons. That neurons may be damaged in Horner’s syndrome. They are the first-order neurons, second-order neurons, and third-order neurons. Each set of neurons has a different causes for the damage of this pathway.
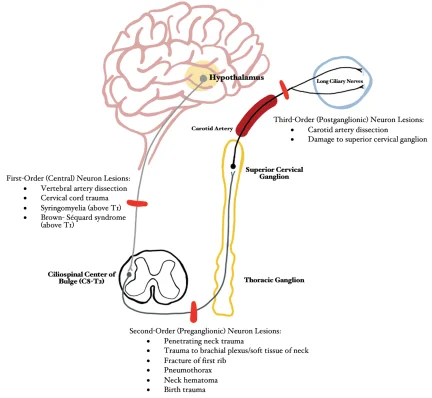
First Order Neuron:
The first-order neuron pathway runs from the brain to the top of the spinal cord. It arise from the posterolateral part of hypothalamus then descend uncrossed through the midbrain and pons after that it terminate in the cell column of the spinal cord at the level of C8-T2.
Symptoms of first order neuron lesion:
- Hemisensory loss
- Dysarthria
- Dysphagia
- Ataxia
- Vertigo
- Nystagmus
Injury to this pathway may be caused by the following conditions:
- Injury to the neck.
- Brain Stroke.
- Any type of Tumour.
- multiple sclerosis disease that affect the protective outer covering of neuron.
- Spinal column cavity or cyst.
Second Order Neuron(Second order pre ganglionic pupilomotor fibres):
The second-order neuron pathway start from the spinal column to the upper chest area and to the side of the neck. In this pathway the spinal cord is at the level of T1 and enter the cervical sympathetic chain. They are in close proximity to the pulmonary apex and the subclavian artery. The fibers ascend therough the sympathetic chain and synapse in the superior cervical ganglion at the level of the separation of the common carotid artery(C3-C4).
Applied anatomy:
- Aneurysm or dissection of the aorta.
- Lesion of the subclavian or common carotid artery.
- Neuroblastoma.
- Lymphadenopathy.
Injury to this path may be caused by the following:
- Chest cavity surgery.
- Damage to heart’s main blood vessel.
- A tumour on the neurons protective outer covering.
- Lung cancer.
- Any traumatic injury.
Third order Neuron(Third order post ganglionic pupilomotor fibres):
The third-order neuron pathway runs from the neck to the skin of the face and also control the iris and eyelids muscle.
This fibres exit the superior cervical ganglion and ascend along the internal carotid artery. Branch off vasomotor travels along the external carotid artery to supply the blood vessels and sweat glands of the face. Internal carotid artery enter the cavernous sinus then it enter the orbit through the superior orbital fissure along with the trigeminal nerve through the long ciliary nerves. The long ciliary nerves supply the dilators of iris and miller muscle.
Third order neuron lesions:
- Internal carotid artery dissection associated with the one side face or neck pain.
- Raeder syndrome(Paratrigeminal nerve)
- Carotid cavernous fistula.
- Cluster or migraine headache.
- Herpes zoster.
- Diplopia from sixth nerve palsy.
Injury to this pathway may be caused by the following:
- Damage to the carotid artery or jugular vein on the side of your neck.
- Severe headaches, including migraines and cluster headaches.
- Any Infection or tumor at the base of your skull.
The common causes for children with Horner’s syndrome include:
- Neuroblastoma (Tumour in the nervous system).
- Injury during birth to their shoulders or neck.
Symptoms of the Horner’s syndrome:

Horner syndrome usually affects only one side of the face. Common signs and symptoms includes:
- A Decrease pupil size (miosis).
- Little bit or small dilatation of the affected pupil in dim light.
- Drooping of the upper eyelid (ptosis).
- Minor elevation of the lower lid, it’s called upside-down ptosis.
- Decrease the sweating on the affected side of the face.
- Ptosis (drooping of the upper eyelid).
- Miosis (constriction of the pupil).
- Enophthalmos (sinking of the eyeball into the face).
- Unable to completely close or open the eyelid.
- Facial flushing.
- Headaches.
- Loss of ciliospinal reflex.
- Bloodshot conjunctiva, depends on the affected area of lesion.
- Straight hair at affected side.
- Heterochromia iridum, The iris of the affected eye is blue-Gray as it is by birth.
Symptoms Horner syndrome in children may include:
- Light iris colour in the affected eye of a child under the age of 1 year.
- Changes are seen on the affected side of the face that is typically appear from heat, physical exertion or any emotional reactions.
Pathophysiology of Horner’s syndrome:
Horner syndrome is occur due to a deficiency of sympathetic activity. In this condition the site of lesion is on the ipsilateral side.
First-order neuron disorder: It affect the Central lesions that involve the hypothalamospinal tract.
Second-order neuron disorder: It also known as Preganglionic lesions. It result compression of the sympathetic chain by the lung tumour. The second order neuron releases acetylcholine.
Third-order neuron disorder: It also known as Post ganglionic lesions. In that a tumour is present in the cavernous sinus or a carotid artery dissection. It releases nor-epinephrine.
Partial Horner’s syndrome: Sometimes in case of a third order-neuron disorder, anhidrosis is present in the middle part of the forehead or it can be absent, that resulting the partial Horner’s syndrome.
When to go to the doctor?
Many different factors can cause the horner syndrome, but some are more serious than others. It is important to give accurate diagnosis. Take a emergency care if signs and symptoms of horner syndrome appear suddenly. It is appear after a accidental injury, or accompanied by other signs or symptoms like,
- Impaired vision.
- Dizziness.
- Altered speech.
- Difficulty in walking.
- Muscle weakness or lack of muscle control.
- Severe, sudden headache or neck pain.
If above any symptoms are appear so that first meet to the doctor.
Diagnosis of Horner syndrome:
First doctor will do a physical examination and ask about patient’s medical history to find out if patient’s has any illness or injury that could have caused the nerve damage. Then, doctor will put eye drops in to the eyes to check how the pupils react.
Physical examination: The doctor will check the patient by an examination and note any visible signs. Doctor will ask patient if you are experiencing other symptoms, such as pain.
Medical history: The doctor will ask to patient about any past illnesses, injuries, and any other surgeries.
Eye examination: A neuro-ophthalmologist – an ophthalmologist who specialise in neurological conditions – they perform tests to measure the response of the pupils of the eye to certain medications. The doctor will put eye drops which containing a small amount of the drug to dilate the pupils. If one pupil is not dilate or open that means it indicate the Horner’s syndrome is present. so that another tests with other types of drugs can give confirmation of the diagnosis.
After that doctor do a special examination or test to find the diagnosis. The Three tests are useful in confirming the presence and severity of Horner syndrome:
Cocaine drop test: Cocaine eye drops block the re uptake of post-ganglionic nor epinephrine that resulting in the dilation of a normal pupil from. However, in Horner’s syndrome the lack of nor-epinephrine in the synaptic cleft causes mydriatic failure.
Paredrine test: This test helps to identify the cause of the miosis. If the third order neuron is intact, then the amphetamine causes neurotransmitter vesicle release, the releasing nor-epinephrine into the synaptic cleft that resulting in robust mydriasis of the affected pupil.
If the lesion present in the third order neuron, then the amphetamine will give no any effect and the pupil remains constricted, not fully open.
Dilation lag test: It is important to diagnose the ptosis that caused by Horner’s syndrome. The ptosis caused by a lesion to the oculomotor nerve. The ptosis occurs with a constricted pupil, in the latter, the ptosis also occurs with a dilated pupil.
Radiological investigations:
Imaging tests: If symptoms indicate the present of a tumour, lesion or any structural abnormality, by the different test check that growth and determine by it is cancerous or benign.
- xrays
- MRI (magnetic resonance imaging)- Powerful magnets and radio waves make detailed images.
- CT scan (computerised tomography)- Several X-rays from different angles are put together to show a more complete picture.
- Carotid ultrasound- Sound waves make an image of your carotid artery.
The doctor also may want to test your blood or urine to check for any health problems that could cause nerve damage.
Treatment of Horner’s syndrome:
Treatment of Horner syndrome depends on the that particular causes. In some cases, however, no supportive treatment is known. Therefore recognition of the syndrome and convenient refer to appropriate specialist doctors. Whether surgical care is necessary it also depends on the particular cause of the horner syndrome. The surgical treatment include neurosurgical care for aneurysm-related Horner syndrome and vascular surgical care conditions like carotid artery dissection or aneurysm.
The treatment of Horner syndrome depends on the affect area and cause of the lesion or tumor. In some cases, surgical excision of the lesion or growth may be appropriate. Radiation and chemotherapy may be helps to patients with malignant tumors. In some of cases, if the Horner’s syndrome’s symptoms are mild, no any special treatment is needed.
Team of special doctors are following:
Pulmonologist, Neurologist or neuro-ophthalmology.
Surgeon or oncology.
Neurosurgeon.
Genetic counseling may be of helpfull for patients and their family members, If patient have the genetic form of this disorder, so that require the genetic counselling to patient and their family members. Another specialist treatment is symptomatic and supportive.
Acute onset of painful Horner’s should be taken a neurological emergency and patient should be evaluate for dissection of the internal carotid artery as described following. That patients has increased risk for cerebral infarction.
Carotid artery dissection: Suitable imaging modalities should be obtained emergently and it may include MRI and MR angiography or CT angiography of the neck. Conventional angiogram remains the gold standard. Patients should be treated promptly by anti coagulation under the supervision of a neurologist.
Neuroblastoma: Children with Horner’s syndrome without exact cause like if trauma should be identify for systemic malignancy particularly neuroblastoma with the help of the paediatrician doctor. doctor should be check the neck and abdominal masses and tested for urinary catecholamine metabolites. Therefore consultation to the paediatric doctor for proper diagnosis.
Brainstem or myelopathic lesions: Patients with brainstem or myelopathic signs needed imaging of the brain and the spinal cord by investigation of MRI. Cavernous sinus and cellar region should be identify in patients with Horner’s syndrome with ophthalmoparesis especially isolated sixth cranial nerve palsy. Those patients should be under the care of a neurologist or neurosurgeon for treatment of the underlying causes.
Thoracic malignancy: Onset of Horner syndrome without any neurological signs should prompt imaging of the neck and thorax for check the lesions of the pulmonary apex or the para-vertebral area. CT or MRI scans should be decided to based on the suspected etiology.
Blepharoptosis: Once serious conditions have been ruled out and the patient is stable, visually symptomatic ptosis can be managed surgically. The Since characteristically the levator palpable function is normal in Horner’s syndrome, surgery typically involves strengthening the action of the levator muscle. The approach may include either aponeurotic advancement or Muller’s muscle- conjunctiva resection.
Doctor advised to patient to do actively whole eye ball movement in front of mirror. If patient have dropping eye do the upper eye muscle or eyebrow pull up and then down repeat it 5 to 7 time with 5 sec hold.
Complication of Horner’s syndrome:
In this syndrome some symptoms are serious. If that symptoms are appear, then person should contact to the doctor immediately. These serious symptoms include:
- Dizziness.
- Problems seeing.
- Sudden or severe neck pain or a headache.
- Muscles weakness or unable to control the muscle movements.
Associated conditions of Horner’s syndrome:
Another conditions may have symptoms that are similar to Horner’s syndrome. Associated conditions are Adie syndrome and Wallenberg syndrome.
Adie syndrome:
This neurological disorder also affects the eye. In normal case, the pupil is larger in the affected eye. However, in some cases, it may see smaller and look like Horner’s syndrome. So that special tests are use to confirm the differential diagnosis.
Wallenberg syndrome:
This condition is also rare. This condition is caused by a blood cloting. However, further tests are usefull to find other symptoms, causes and confirm the diagnosis.
Other Differential Diagnosis:
- Anisocoria.
- Adie pupil.
- Argyll Robertson pupil.
- Holmes-Adie pupil.
- Iris spincter muscle damage.
- Senile miosis.
- Third nerve palsy.
- Unilateral Use of mitotic drugs.
- Unilateral use of mydriatic drugs.
Prognosis:
The prognosis of Horner’s syndrome also depends on that cause. The symptoms of Horner’s syndrome do not have a affect on the quality of life or eye vision. However, it may indicate the presence of a serious or life-threatening illness that requires proper medical attention.
FAQ
What are the 3 classic signs of Horner’s syndrome?
Signs and symptoms of Horner syndrome includes decreased pupil size(miosis), a drooping eyelid(ptosis) and decreased sweating(anhidrosis) on the affected side of the face. This three sign is known as the triad sign or symptom.
What pathway is damaged in Horner’s syndrome?
The Sympathetic nerve pathway is damaged in the horner syndrome. This pathway is start from the hypothalamus of the brain then descend down to the spinal column after that reach to the skin or face. This whole pathway divided in the phase : Fist order neuron, Second order neuron and third order neuron. So this disease symptoms and treatment is depends according to which type of pathway is damage.
Which muscle is paralysed in Horner syndrome?
The affected side pupil may be round and constricted (miosis) in this syndrome. In Horner syndrome, the anisocoria is more in darkness than in light. So the affected pupil dilates more slowly than the normal pupil does because the affected pupil lacks the pull of the dilator muscle ( dilation lag). The dilator muscle is more commonly affected in this syndrome.
What is the most common cause of Horner’s syndrome?
It is caused by damage to the sympathetic nerves. The causes of Horner’s syndrome different and may include a tumour, stroke, injury or underlying disease that affecting the surrounding areas of the sympathetic nerves pathway. the exact cause is unknown in this syndrome.
How does Horner’s syndrome affect vision?
Individuals who have Horner syndrome after age of 2 yrs do not generally have iris heterochromia. The abnormalities in the eye area related to Horner syndrome do not generally affect vision or health. It affects the eye muscles like eye opening and closer muscles , pupil dilators muscle.
What neurological disorder causes droopy eyelids?
Myasthenia Gravis related cause of droopy eyelids, Symptoms: Droopy Eyelid, Double Vision & More. Myasthenia Gravis is one type of neurological condition. It begins with droopy eyelids and can progress to weakness in voluntary muscles elsewhere in the body. The National Neuroscience Institute gives its symptoms.
What is oculomotor nerve palsy?
The oculomotor nerve is the 3 cranial nerve. The oculomotor nerve palsy or oculomotor neuropathy is one of an eye condition resulting from damage to the third cranial nerve or a nerve branch thereof. Due to this nerve affection the eye movements are decreased or loss.







One Comment