Claw Hand Deformity
Table of Contents
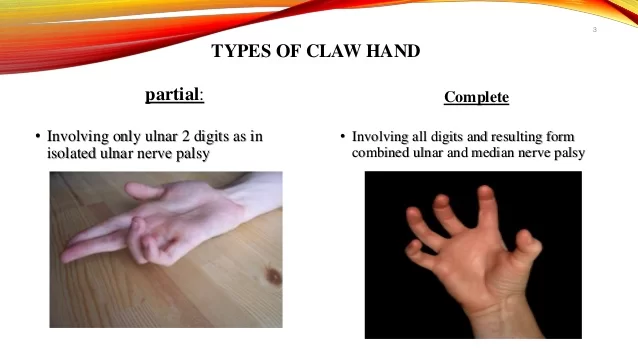
What is a Claw Hand Deformity?
Claw hand deformity, also known as clawing of the hand or claw hand syndrome, is a condition characterized by the abnormal positioning of the fingers and hand, resulting in a claw-like appearance. This deformity is usually caused by the imbalance or dysfunction of muscles and tendons in the hand.
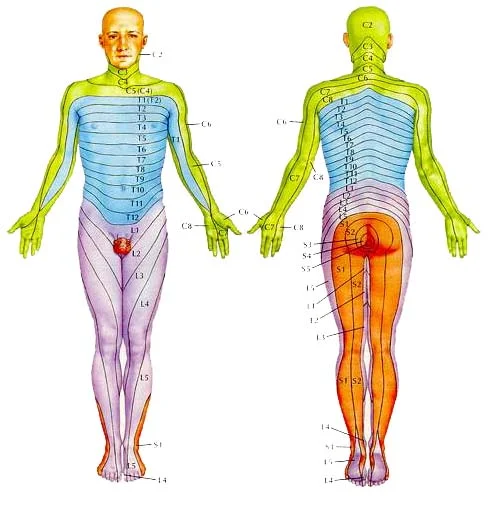
The claw hand deformity is typically associated with ulnar nerve dysfunction, which is responsible for controlling the muscles in the hand and forearm. The ulnar nerve originates from the lower neck and travels down the arm, passing through the elbow region and extending into the hand. Any damage or compression along the course of the ulnar nerve can lead to claw hand deformity.
- Ulnar nerve palsy is the loss of sensory and motor function.
- This can occur after injury to any portion of the ulnar nerve.
- The ulnar nerve is the terminal branch of the medial cord (C8, T1).
- The ulnar nerve innervates the flexor carpi ulnaris after it passes through the cubital tunnel.
Other muscles innervated by the ulnar nerve are the flexor digitorum profundus of the ring and small fingers and the following hand muscles:
- Abductor digiti minimi
- Flexor digiti minimi
- Opponens digiti minimi
- Ring
- Small finger lumbricals
- Dorsal and palmar interosseous muscles
- Adductor pollicis
- Deep head of flexor pollicis brevis
- The first dorsal interosseous. When the ulnar nerve is injured, the muscles innervated by the nerve begin to weaken. This leads to an imbalance between the strong extrinsic muscles (i.e., extensor digitorum communis) and the weakened intrinsic muscles (i.e., interosseous and lumbricals). This imbalance is characterized clinically by metacarpophalangeal (MCP) hyperextension and proximal
- interphalangeal (PIP) and distal interphalangeal (DIP) flexion.
What are the Common Cause Of Claw Hand?
- Causes of claw hand can also be due to anything that may lead to ulnar nerve palsy. Ulnar nerve palsy can arise from a laceration anywhere along its course.
- Proximal injuries to the medial cord of the brachial plexus may also present with sensory loss distally.
- Ulnar nerve palsies can also be due to cubital tunnel syndrome and ulnar tunnel syndrome.
- These are compression neuropathies at the elbow and wrist.
- Another cause of ulnar nerve palsy may be due to a failure to splint the hand in an intrinsic-plus posture following a crush injury.
- There are a few systemic diseases that may also lead to ulnar nerve palsy.
- These include leprosy, syringomyelia, and Charcot-Marie-Tooth disease. However, these systemic diseases usually involve more than one nerve.
Epidemiology :
- Claw Hand can be congenital or acquired.
- Men are more likely to acquire the condition than a woman, but the congenital form of claw hand is distributed evenly among men and women.
- There are no racial or ethnic preferences for claw hand.
Pathophysiology of Claw Hand :
Pathoanatomic components relate to the imbalance between the extrinsic and intrinsic muscles. Weakened intrinsic muscles lead to a loss of MCP flexion and a loss of interphalangeal (IP) extension. Strong extrinsic muscles will lead to an unopposed extension of the MCP joints. The flexor digitorum profundus and flexor digitorum superficialis muscles not innervated by the Ulnar nerve remain strong and lead to unopposed flexion of the PIP and DIP joints.
History and Physical sing :
- The initial presentation will include a decrease in normal hand function.
- The MCP joints will be hyper-extended, and the IP joints flexed.
- The second and third digits will not be as involved as the fourth and fifth digits with a true ulnar nerve palsy. This is because the median nerve innervates the lumbricals involving the second and third digits, and the ulnar nerve innervates the lumbricals involving the fourth
and fifth digits.
- The patient may also exhibit functional weakness while attempting a grasp, grip or pinch.
- A provocative test for claw hand is bringing the MCP joints into flexion. This will correct
the DIP and PIP joint deformities.
- Several other specific tests for ulnar nerve palsy include:
- Froment sign: Hyperflexion of the thumb IP joint while attempting to grab. This indicates a substitution of flexor pollicis longus (innervated by median nerve) for adductor pollicis (innervated by ulnar nerve).
- Jeanne sign: Reciprocal hyperextension of the thumb MCP joint indicating substitution of flexor pollicis longus (FPL) for adductor pollicis.
- Wartenberg sign: Abduction of the small finger at MCP joint indicating deficient palmar intrinsic muscle (innervated by ulnar nerve) with abduction from extensor digiti minimi (innervated by radial nerve).
- Duchenne sign: Clawing of the ring and small fingers, hyperextension of MCP joints, and flexion of PIP joints indicating deficient interosseous and lumbrical muscles of the ring and small fingers.
Functional disability / Symptoms in Claw Hand :

- Weakness, especially in turning doorknobs, keys in locks, and taking tops off jars is a common complaint due to the lack of abduction/adduction of the fingers.
- Pickup is clumsy, especially in the full claw hand where the pulps of the fingers cannot be presented to the object because of the inability to fully extend the interphalangeal joints. This results in the nails pushing the
- object away during attempts at pick-up. The thumb pinch grip is also greatly weakened and clumsy due to adductor paralysis and the collapsing interphalangeal joint converting the pulp pinch of the thumb into a nail pinch. Thumb disability is further magnified in the full claw hand
- where median innervated thenar muscles are also paralysed. Strong power grip of the fingers into the palm, however, is retained, except where the long flexors are involved in high nerve injuries.
- Fixed flexion contractures of the proximal interphalangeal joints of the clawed fingers can develop as a secondary phenomenon due to lack of active extension and trophic changes may occur due to numbness. Wartenberg’s abducted little finger is a frequent source of nuisance.
Evaluation in Claw Hand :
- EMG
- NCV
- Electromyographic and nerve conduction velocity studies are used to evaluate the ulnar nerve pathology and to rule out other diagnoses.
Differential Diagnoses
Differentiation from Other Diseases is
- Cervical Radiculopathy
- lower brachial plexopathy.
What are the Common Treatments procedure for Claw Hand?
- Non-operative management is applied if a fixed flexion contracture of more than 45 degrees occurs at the PIP joint. A strenuous hand therapy program is utilized involving serial casting.
- The majority of cases will need operative management in the form of contracture release and passive tenodesis versus active tendon transfer. This treatment is reserved for those patients with a progressive deformity that is affecting their quality of life. The goal is to prevent lasting MCP joint hyper-extension.
- Surgery is usually in the form of tendon transfers. This addresses issues including the lack of thumb adduction and lateral pinch, the claw deformity of the fingers that impairs object acquisition, and the loss of ring and small finger flexion.
- The extensor carpi radialis brevis or the flexor digitorum superficialis are the most commonly used transfers to restore thumb adduction. The brachioradialis can be used if the extensor carpi radialis brevis is required for an intrinsic reconstruction of the fingers.
- To correct the claw deformity of the fingers include static procedures or dynamic transfers. A dynamic transfer uses the flexor digitorum superficialis, extensor carpi radialis longus, extensor carpi radialis brevis, or flexor carpi radialis as a donor muscle.
- To restore the ring and small finger extrinsic muscle function, a transfer of flexor digitorum profundus ring and small to flexor digitorum profundus middle is performed.
Physiotherapy Treatment in Claw Hand
- The claw hand develops due to a weakness of the deep muscles of your hand. To improve the strength of these muscles, you will need to work on gripping objects.
- This can be done with objects around the house. Start small with objects that can be easily held and squeezed with light resistance.
- Examples of these objects include stress balls and pillows. Then work your way up to a tennis ball. Squeeze these objects with two to three fingers at a time to improve the strength of each individual finger. Additionally, it is always a good idea to see your doctor for a follow-up evaluation and for possible referral to a certified athletic trainer who can outline a progression of exercises for you.
- If you find daily tasks difficult to do because you suffer from stiffness, swelling, or pain in your hands, the right exercises can help get you back in motion.
- Physiotherapists usually suggest specific exercises depending on the condition. Some help increase a joint’s range of motion or lengthen the muscle and tendons via stretching. These exercises are helpful for osteoarthritis as well as tennis elbow and golfer’s elbow—but not when the joints are inflamed or painful. Other exercises strengthen muscles around a joint to generate more power or to build greater endurance. These are helpful for inflammation of the tendons (tendinitis) and nonpainful arthritis conditions.
Your muscles and tendons move the joints through arcs of motion, as when you bend and straighten your fingers. If your normal range of motion is impaired—if you can’t bend your thumb without pain, for example, you may have trouble doing ordinary things like opening a jar. These exercises move your wrist and fingers through their normal ranges of motion and require all the hand’s tendons to perform their specific functions. Hold each position for 5–10 seconds. Do one set of 10 repetitions, three times a day.
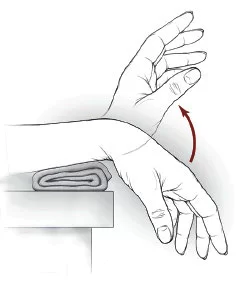
1 Wrist extension and flexion exercise
• Place your forearm on a table on a rolled-up towel for padding with your hand hanging off the edge of the table, palm down.
• Move the hand upward until you feel a gentle stretch.
• Return to the starting position.
• Repeat the same motions with the elbow bent at your side, palm facing up.
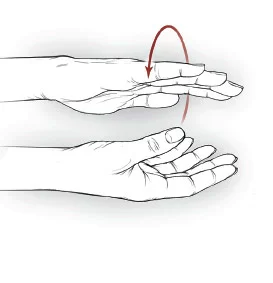
- Wrist supination/pronation
• Stand or sit with your arm at your side with the elbow bent to 90 degrees, palm facing down.
• Rotate your forearm, so that your palm faces up and then down.
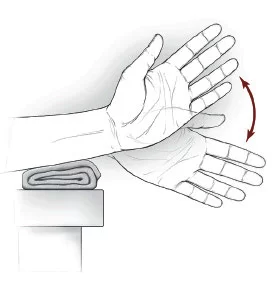
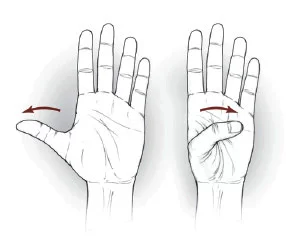
- Wrist ulnar/radial deviation Wrist ulnar/radial deviation exercise
• Support your forearm on a table on a rolled-up towel for padding or on your knee, thumb upward.
• Move the wrist up and down through its full range of motion.
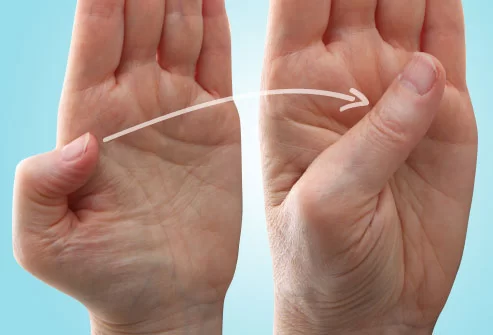
- Thumb flexion/extension
Thumb flexion/extension exercise
• Begin with your thumb positioned outward.
• Move the thumb across the palm and back to the starting position.
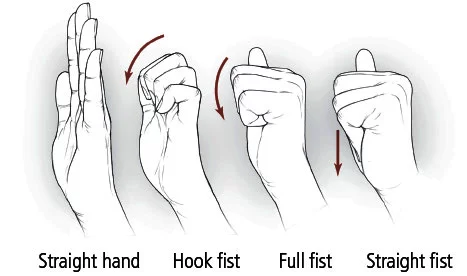
- Hand/finger tendon glide
Hand/finger tendon glide exercise
• Start with the fingers extended straight out.
• Make a hook fist; return to a straight hand.
• Make a full fist; return to a straight hand.
• Make a straight fist; return to a straight hand.
1) Make a Fist
Hand and finger exercises can help strengthen your hands and fingers, increase your range of motion, and give you pain relief. Stretch only until you feel tightness. You shouldn’t feel pain. Start with this simple stretch:
Make a gentle fist, wrapping your thumb across your fingers.
Hold for 30 to 60 seconds. Release and spread your fingers wide.
Repeat with both hands at least four times.

2) Finger Stretch
Try this stretch to help with pain relief and to improve the range of motion in your hands:
Place your hand palm-down on a table or other flat surface.
Gently straighten your fingers as flat as you can against the surface without forcing your joints.
Hold for 30 to 60 seconds and then release.
Repeat at least four times with each hand.
3) Claw Stretch
This stretch helps improve the range of motion in your fingers.
Hold your hand out in front of you, palm facing you.
Bend your fingertips down to touch the base of each finger joint. Your hand should look a little like a claw.
Hold for 30 to 60 seconds and release. Repeat at least four times on each hand.

4) Grip Strengthener
This exercise can make it easier to open door knobs and hold things without dropping them.
Hold a soft ball in your palm and squeeze it as hard as you can.
Hold for a few seconds and release.
Repeat 10 to 15 times on each hand. Do this exercise two to three times a week, but rest your hands for 48 hours in between sessions. Don’t do this exercise if your thumb joint is damaged.

5) Pinch Strengthener
This exercise helps strengthen the muscles of your fingers and thumb. It can help you turn keys, open food packages, and use the gas pump more easily.
Pinch a soft foam ball or some putty between the tips of your fingers and your thumb.
Hold for 30 to 60 seconds.
Repeat 10 to 15 times on both hands. Do this exercise two to three times a week, but rest your hands for 48 hours in between sessions. Don’t do this exercise if your thumb joint is damaged.

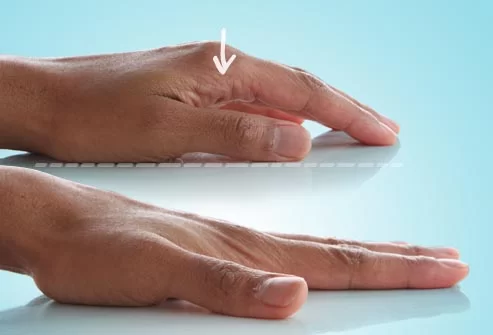
6) Finger Lift
Use this exercise to help increase the range of motion and flexibility in your fingers.
Place your hand flat, palm down, on a table or other surface.
Gently lift one finger at a time off of the table and then lower it.
You can also lift all your fingers and thumb at once, and then lower.
Repeat eight to 12 times on each hand.

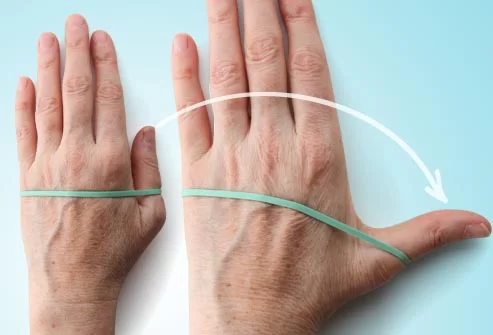
7) Thumb Extension
Strengthening the muscles of your thumbs can help you grab and lift heavy things like cans and bottles.
Put your hand flat on a table. Wrap a rubber band around your hand at the base of your finger joints.
Gently move your thumb away from your fingers as far as you can.
Hold for 30 to 60 seconds and release.
Repeat 10 to 15 times with both hands. You can do this exercise two to three times a week, but rest your hands for 48 hours in between sessions.
8) Thumb Flex
This exercise helps increase the range of motion in your thumbs.
Start with your hand out in front of you, palm up.
Extend your thumb away from your other fingers as far as you can. Then bend your thumb across your palm so it touches the base of your small finger.
Hold for 30 to 60 seconds.
Repeat at least four times with both thumbs.

9) Thumb Touch
This exercise helps increase the range of motion in your thumbs, which helps with activities like picking up your toothbrush, fork and spoon, and pens when you write.
Hold your hand out in front of you, with your wrist straight.
Gently touch your thumb to each of your four fingertips, one at a time, making the shape of an “O.”
Hold each stretch for 30 to 60 seconds. Repeat at least four times on each hand.

10) Thumb Stretches
Try these two stretches for your thumb joints:
Hold your hand out, palm facing you. Gently bend the tip of your thumb down toward the base of your index finger. Hold for 30 to 60 seconds. Release and repeat four times.
Hold your hand out, palm facing you. Gently stretch your thumb across your palm using just your lower thumb joint. Hold for 30 to 60 seconds. Release and repeat four times.
11) Play With Clay
Playing with putty or clay is a great way to increase the range of motion in your fingers and strengthen your hands at the same time. And it won’t even feel like exercise. Just follow the kids’ lead — squish the clay into a ball, roll it into long “snakes” with your palms, or use your fingertips to pinch spikes on a dinosaur.
Complications
- More complications occur after intrinsic muscle transfers than adductor plasty because of the unique balance of the extensor hood mechanism.
- The transfer may not be suitable if the chosen muscle has insufficient strength or excursion. Elongation is also a problem with sewing the transfer into the lateral bands of the extensor hood.
- Tendon transfers that are not strong enough can be treated with a therapy program to strengthen the muscle but often require surgical revision.
- The transfer may also not be suitable if the chosen muscle has too much strength or too short of excursion. When the transfer is sewn too tightly into the lateral band, it can produce a swan-neck deformity of the digit.
- Tendon transfers that are too tight or too strong can be treated with a passive range of motion therapy to allow stretching to occur.
Post-operative and Rehabilitation Care
A very experienced hand therapist plays a vital role in the postoperative care of tendon transfers for ulnar nerve palsy. Protecting the transfers with custom splints while mobilizing uninvolved joints requires strict adherence to postoperative protocols. Following most procedures, the hand is immobilized for 3 to 4 weeks, followed by a blocking splint to allow movement within the restraints of the splint for the next 3 to 4 weeks. Passive exercises are started at 6 weeks and strengthening at 8 weeks for the adductor-plasty and 10 to 12 weeks for the intrinsic tendon transfers.




One Comment