Ostiopetrosis
Table of Contents
Definition-
Osteopetrosis is a bone disease that makes bones abnormally dense and prone to breakage (fracture). Researchers have described several major types of osteopetrosis, which are usually distinguished by their pattern of inheritance: autosomal dominant, autosomal recessive, or X-linked.
Osteopetrosis (“marble bone disease”) is a descriptive term that refers to a group of rare, heritable disorders of the skeleton characterized by increased bone density on radiographs. The overall incidence of these conditions is difficult to estimate but autosomal recessive osteopetrosis (ARO) has an incidence of 1 in 250,000 births, and autosomal dominant osteopetrosis (ADO) has an incidence of 1 in 20,000 births. Osteopetrotic conditions vary greatly in their presentation and severity, ranging from neonatal onset with life-threatening complications such as bone marrow failure (e.g. classic or “malignant” ARO), to the incidental finding of osteopetrosis on radiographs (e.g. osteopoikilosis).
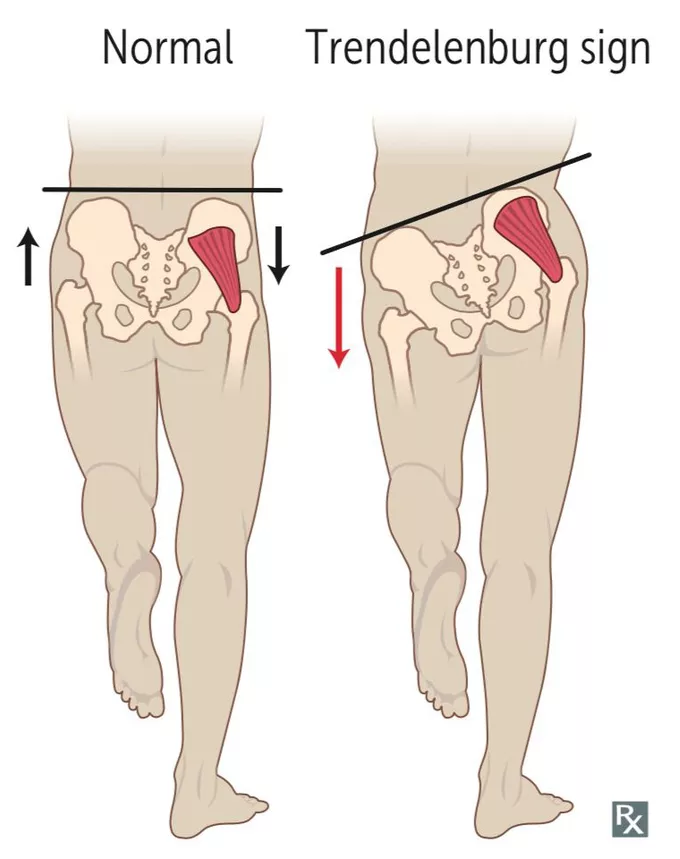
Classic ARO is characterised by fractures, short stature, compressive neuropathies, hypocalcaemia with attendant tetanic seizures, and life-threatening pancytopaenia. The presence of primary neurodegeneration, mental retardation, skin, and immune system involvement, or renal tubular acidosis may point to rarer osteopetrosis variants, whereas onset of primarily skeletal manifestations such as fractures and osteomyelitis in late childhood or adolescence is typical of ADO. Osteopetrosis is caused by failure of osteoclast development or function and mutations in at least 10 genes have been identified as causative in humans, accounting for 70% of all cases.
These conditions can be inherited as autosomal recessive, dominant, or X-linked traits with the most severe forms being autosomal recessive. Diagnosis is largely based on clinical and radiographic evaluation, confirmed by gene testing where applicable, and paves the way to understanding natural history, specific treatment where available, counselling regarding recurrence risks, and prenatal diagnosis in severe forms. Treatment of osteopetrotic conditions is largely symptomatic, although haematopoietic stem cell transplantation is employed for the most severe forms associated with bone marrow failure and currently offers the best chance of longer-term survival in this group.
The severe infantile forms of osteopetrosis are associated with diminished life expectancy, with most untreated children dying in the first decade as a complication of bone marrow suppression. Life expectancy in the adult onset forms is normal. It is anticipated that further understanding of the molecular pathogenesis of these conditions will reveal new targets for pharmacotherapy.
Osteopetrosis refers to a group of rare, inherited skeletal disorders characterized by increased bone density and abnormal bone growth. Symptoms and severity can vary greatly, ranging from neonatal onset with life-threatening complications (such as bone marrow failure) to the incidental finding of osteopetrosis on X-ray.
Depending on severity and age of onset, features may include fractures, short stature, comprehensive nephropathy (pressure on the nerves), hypoglycemia with attendant titanic seizures, and life-threatening pancytopenia. In rare cases, there may be neurological impairment or involvement of other body systems. Osteopetrosis may be caused by mutations in at least 10 genes. Inheritance can be autosomal recessive, autosomal dominant, or X-linked recessive with the most severe forms being autosomal recessive. Management depends on the specific symptoms and severity and may include vitamin D supplements, various medications, and/or surgery. Adult osteopetrosis requires no treatment by itself, but complications may require intervention.
Causes of Ostiopetrosis:
Mutations in the TCIRG1 gene cause about 50% of cases of autosomal recessive osteopetrosis. Mutations in the IKBKG gene cause X-linked osteopetrosis. Mutations in other genes are less common causes of osteopetrosis. In about 30% percent of affected people, the cause is unknown. Osteopetrosis, or marble bone disease, is a rare skeletal disorder due to a defective function of the osteoclasts. This defect renders bones more susceptible to osteomyelitis due to decreased vascularity. This disorder is inherited as autosomal dominant and autosomal recessive various types of osteopetrosis are caused by genetic changes (mutations) in one of at least ten genes. There is nothing a parent can do before, during, or after pregnancy to cause osteopetrosis in a child.
The genes associated with osteopetrosis are involved in the development and/or function of osteoclasts,[4] cells that break down bone tissue when old bone is being replaced by new bone (bone remodeling). This process is necessary to keep bones strong and healthy. Mutations in these genes can lead to abnormal osteoclasts, or having too few osteoclasts. If this happens, old bone cannot be broken down as new bone is formed, so bones become too dense and prone to breaking. Mutations in the CLCN7 gene cause most cases of autosomal dominant osteopetrosis, 10-15% of cases of autosomal recessive osteopetrosis (the most severe form), and all known cases of intermediate autosomal osteopetrosis.
Mutations in the TCIRG1 gene cause about 50% of cases of autosomal recessive osteopetrosis.
Mutations in the IKBKG gene cause X-linked osteopetrosis.
Mutations in other genes are less common causes of osteopetrosis.
In about 30% percent of affected people, the cause is unknown.
People with questions about the specific cause of osteopetrosis in themselves or a family member are encouraged to speak with a genetics professional.
Signs and symptoms of Ostiopetrosis:

Osteopetrosis is characterized by overly dense bones throughout the body. Symptoms include fractures, low blood cell production, and loss of cranial nerve function causing blindness, deafness, and/or facial nerve paralysis. Affected individuals may experience frequent infections of teeth and the bone in the jaw
Osteopetrosis, Autosomal Recessive; Malignant Infantile Type-
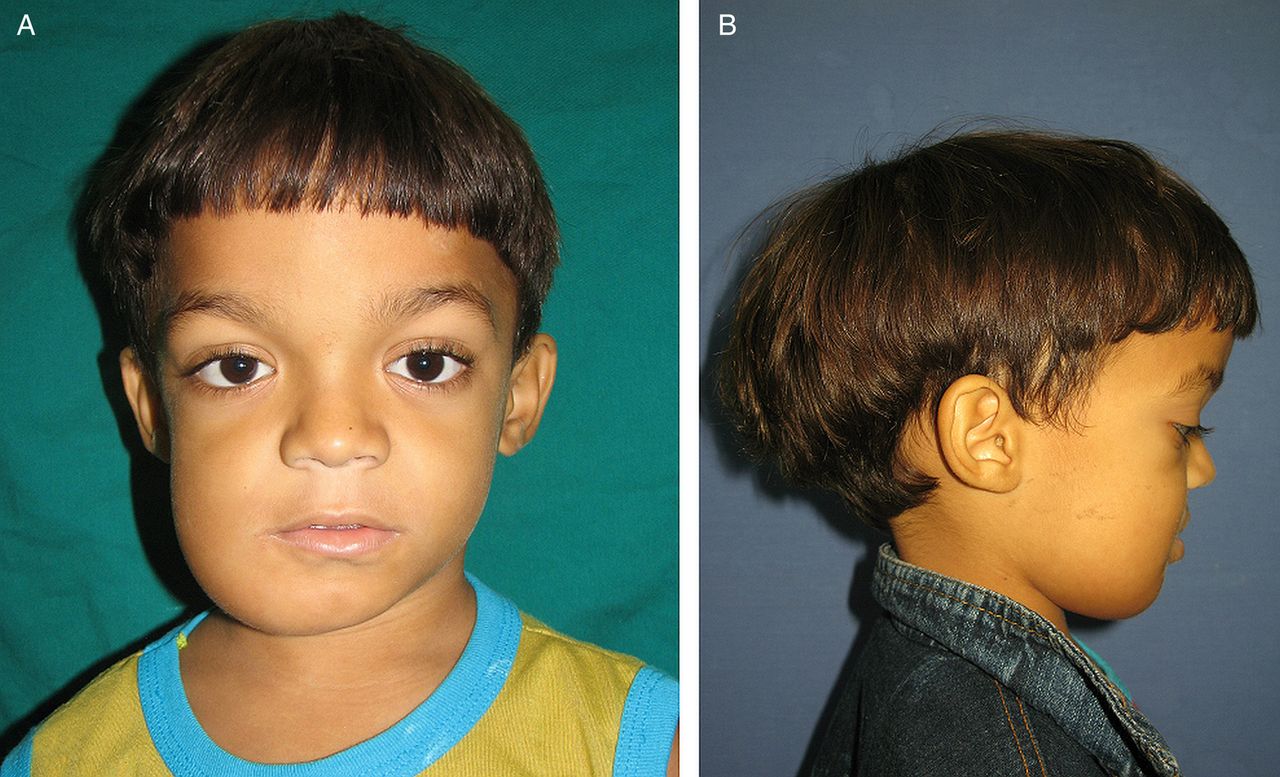
The most severe type of osteopetrosis, malignant infantile type, is apparentfrom birth, and if left untreated, can lead to death in the first decade of life. Symptoms vary depending on the exact gene change (mutation). Affected individuals may have an abnormally large head (macrocephaly). They may also have hydrocephalus, characterized by inhibition of the normal flow of cerebrospinal fluid (CSF) within and abnormal widening (dilatation) of the cerebral spaces of the brain (ventricles), causing accumulation of CSF in the skull and potentially increased pressure on brain tissue. Symptoms that affect the eyes may include wasting away (atrophy) of the retina, eyes that appear widely spaced (hypertelorism), eyes that protrude from their orbits (exophthalmos), cross-eyes (strabismus), involuntary rhythmic movements of the eyes (nystagmus), and blindness.
Other symptoms associated with malignant infantile type of osteopetrosis include hearing loss, abnormally small jaw (micrognathia), chronic inflammation of the mucous membranes in the nose (rhinitis), eating difficulties, and/or growth retardation. Some affected individuals experience delays in acquiring skills that require the coordination of muscles and voluntary movements (delayed psychomotor development). Some affected individuals may experience delayed tooth development or severe dental caries.
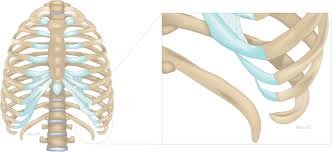
In addition, abnormal enlargement of the liver and spleen (hepatosplenomegaly); abnormal hardening of some bones (osteosclerosis); fractures, usually of the ribs and long bones; inflammation of the lumbar vertebrae (osteomyelitis); increased density of the cranial bones (cranial hyperostosis) leading to nerve compression; and/or increased pressure inside the skull may also occur. Patients can also present with seizures due to low levels of calcium in the blood. Symptoms of severe neurodegeneration can manifest in rare variants of malignant infantile osteopetrosis.

Osteopetrosis, Autosomal Dominant; Adult Type-
A milder form of osteopetrosis, the adult type, is usually diagnosed in late childhood or adulthood. There is predominance of bone symptoms, including osteosclerosis, fractures after minimal trauma (usually of the ribs and long bones), osteomyelitis (especially of the jaw), and cranial hyperostosis.
In some cases, affected individuals may have pus-filled sacs in the tissue around the teeth (dental abscess). In many cases, individuals may exhibit no symptoms (asymptomatic). Affected individuals may also experience rhinitis, hepatosplenomegaly, anemia, and extramedullary hematopoiesis.
Diagnosis:
A diagnosis of osteopetrosis is based on a thorough clinical evaluation, detailed patient history, and a variety of specialized tests such as x-ray imaging and measurement of bone mass density (BMD) which is increased. Skeletal X-ray findings are very specific and are considered sufficient to make a diagnosis. Biochemical findings like increased concentration of creatinine kinase BB isoenzyme and tartrate-resistant acid phosphatase (TRAP) can also help make the diagnosis.
Clinical Testing and Work-Up
Genetic testing can pinpoint the mutation in over 90% of cases: this can identify forms of osteopetrosis with unique clinical associations or complications and direct the management plan. A bone biopsy is sometimes performed to confirm the diagnosis, but not routinely done as it is an invasive procedure with non-negligible risks.
Once the diagnosis is made, the following blood tests should be done:
serum calcium, parathyroid hormone, phosphorus, creatinine, 25-hydroxyvitamin D, complete blood count with differential, creatine kinase isoenzymes (specifically the BB isozyme of creatine kinase), and lactate dehydrogenase. These measurements will determine the need for supplementation and for referral to specialists. Baseline magnetic resonance imaging of the brain should be arranged to evaluate cranial nerve involvement, hydrocephalus, and vascular abnormalities.
Affected individuals should be evaluated regularly by an ophthalmologist for optic nerve involvement, and benefit from a multidisciplinary approach including endocrinology, ophthalmology, genetics, and dentistry, with input from orthopedics, otorhinolaryngology, neurology, neurosurgery, nephrology, infectious disease, and hematology specialists as needed.
Treatment of Ostiopetrosis
Initial management should focus on establishing the severity and extent of the disease.
Treatment of osteopetrosisAdult osteopetrosis–
Adult osteopetrosis requires no treatment by itself, although complications of the disease may require intervention. No specific medical treatment exists for the adult type. Surgical treatment may be needed for deformities and fracturesInfantile osteopetrosis
Vitamin DVitamin D stimulates dormant osteoclasts, and thus bone resorption. Large doses of calcitriol, along with restricted calcium intake, sometimes improve osteopetrosis though modestly and till the treatment is given. Gamma Interferon
Gamma interferon leads to long-term benefits. It improves hemoglobin, platelet counts, and white blood cell function thus decreasing susceptibility to infections.
Trabecular bone volume substantially decreases and bone-marrow volume increases. Provides better results in combination therapy with calcitriol
ErythropoietinErythropoietin is used to correct anemia. It stimulates the bone marrow to produce more red blood cells. Corticosteroids
Corticosteroids increase red blood cells and also stimulate bone resorption. But steroids are not preferred because they need to be given for a long time.
Bone Marrow Transplantation
Bone marrow transplantation can cure bone marrow failure and metabolic abnormalities in patients whose disease arises from an intrinsic defect of the osteoclast lineage. Bone marrow transplantation is the only cure for this disease. Other Treatments
Fractures occurring in these patients are treated as per need and surgery might be necessary
How can Physiotherapy help with osteoporosis?
Physiotherapy can help you strengthen your bones, as well as your muscles. It can prevent bone thinning, reduce falls and help you manage any pain. Bone is a living tissue that can be improved through some types of exercise. A physiotherapist can work with you to find activities that suit your needs and that will strengthen your bones.
Osteoporosis is more common in older people and is often the reason why they fall. Falling is a common problem for people aged 65 and over. If you are at risk of falling, a physio can help you improve your balance. Physios are the third largest health profession after doctors and nurses. They work in the NHS, in private practice, for charities, and in the workplace, through occupational health schemes.