Cervical Spine
Table of Contents
Introduction
The cervical spine is comprised of the initial 7 vertebrae, alluded to as C1-7 (see the pictures underneath). It has the capability to give versatility and soundness to the head while interfacing it with the moderately stationary thoracic spine. The cervical spine might be separated into 2 sections: upper and lower.
The cervical spine, or neck section of the spine, is made up of seven vertebrae, which are stacked bones. The initial two vertebrae of your cervical spine are one-of-a-kind in shape and capability. Your most memorable vertebra (C1), likewise called the chart book, is a ring-molded bone that starts at the foundation of your skull. It’s named after Map book, of Greek folklore, who held the world on his shoulders. The chart book holds your head upstanding. Your subsequent vertebra (C2), likewise called the hub, permits the map book to turn against it for the side-to-side “no” pivot of your head.
Your seven cervical vertebrae (C1 to C7) are associated at the rear of the bone by a sort of joint (called feature joints), which consider the forward, reverse, and turning movements of your neck.
Your cervical spine is additionally encircled by muscles, nerves, ligaments, and tendons. “Shock-engrossing” plates, called intervertebral circles, are situated between every vertebra. Your spinal string goes through the focal point of your whole spine. Your spinal string sends and gets messages from your cerebrum, which controls all parts of your body’s capabilities.
Your cervical spine has a few capabilities, including:
- Protecting your spinal cord. The nerves of your spinal rope go through a huge opening (called the vertebral foramen) that goes through the focal point of your vertebrae as a whole — from the foundation of your skull through the cervical vertebrae, the thoracic (center back) vertebrae and finishing between the first and second lumbar (lower back) vertebrae. Taken together, every one of the stacked vertebrae of your spine structure a defensive focal trench that safeguards your spinal line.
- Supporting your head and allowing movement. Your head weighs 10 to 13 pounds on average, which is held up by your cervical spine. It also allows you to tilt forward or backward, rotate from side to side, and bend your head and neck to one side (ear-to-shoulder; lateral flexion).
- Providing a safe passageway for vertebral arteries. Through small holes in cervical spine vertebrae C1 through C6, vertebral arteries deliver blood to the brain. There are no other vertebrae in the entire spine with perforations in the bone that let arteries pass through.
Upper Cervical Spine
The upper cervical spine comprises the map book (C1) and the pivot (C2). These initial 2 vertebrae are very not the same as the remainder of the cervical spine (see the picture beneath). The chart book verbalizes superiorly with the occiput (the atlantooccipital joint) and poorly with the hub (the atlantoaxial joint).
The atlantoaxial joint is liable for half of all cervical turns; the atlantooccipital joint is answerable for half of flexion and expansion. The one-of-a-kind elements of C2 life systems and their enunciations convolute evaluation of its pathology.
Atlas (C1)
The chart book is ring-formed and doesn’t have a body, in contrast to the other vertebrae. Combined leftovers of the map book body have become pieces of C2, where they are known as the odontoid cycle, or nooks. The odontoid cycle is held in close nearness to the back part of the foremost curve of the map book by the cross-over tendon, which settles the atlantoaxial joint. The apical, alar, and cross-over tendons, by permitting spinal section pivot, give further adjustment and forestall back relocation of the sanctums according to the map book.
The chart book is comprised of a thick front curve, a dainty back curve, 2 noticeable sidelong masses, and 2 cross-over processes. The cross-over foramen, through which the vertebral supply route passes, is encased by the cross-over process.
On every horizontal mass is a prevalent and sub-par feature (zygapophyseal) joint. The unrivaled articular features are kidney-molded, curved, and face up and internal. These unrivaled aspects articulate with the occipital condyles, which face descending and outward. The generally level sub-par articular aspects face descending and internal to express the unrivaled features of the hub.
As indicated by Steele’s standard of thirds, at the level of the map book, the odontoid cycle, the subarachnoid space, and the spinal line each involves 33% of the region of the spinal channel.
Axis (C2)
The pivot has an immense vertebral body, which contains the odontoid cooperation (sanctums). The odontoid cycle expresses with the premier bend of the graph book through its front articular viewpoint and is held set up by the get-over ligament. The turn is made from a vertebral body, profound pedicles, laminae, and get-over processes, which go about as association centers for muscles. The turn communicates with the graph book through its dominating articular viewpoints, which are angled and face up and outward.
Embryology
C2 has a complex embryologic development. It is gotten from 4 solidifying places: 1 for the body, 1 for the odontoid collaboration, and 2 for the mind bends. The odontoid cycle wires by the seventh gestational month.
After entering the world, an insignificant cartilaginous plate space called the neurocentral synchondrosis secludes the odontoid communication from the assortment of C2. The synchondrosis is seen in basically all children developed 3 years and is absent in those developed 6 years. The apical piece of the sanctuaries solidifies by age 3-5 years and wires with the rest of the development around age 12 years. It is important to distinguish this synchondrosis from a break.
Bits of the occiput, map book, and turn are gotten from the proatlas. The hypocentrum of the fourth sclerotome structures the preeminent tubercle of the clivus. The centrum of the proatlas sclerotome transforms into the apical cap of the alcoves and the apical ligaments.
The mind-bends portions of the proatlas are apportioned into rostral and ventral parts. The rostral part approaches the first piece of the foramen magnum and the occipital condyles; the caudal part shapes the unparalleled piece of the back bend of the graph book and the equal atlantal masses. The alar and cruciate ligaments are formed from the level pieces of the proatlas.
Vasculature
There is a wide vein anastomotic association around the refuges, dealt with by the matched front and back climbing courses rising up out of the vertebral veins around the C3 level and the carotid vein arcade from the groundwork of the skull. The front and back climbing conductors show up at the groundwork of the dens through the adornment ligaments and run cephalad at the edges to show up at the tip of the connection. The anastomotic arcade similarly gets feeders from the rising pharyngeal veins that join the arcade right after going through the occipital condyle.
Various plans around or including your cervical spine integrate the following with:.
Muscles supporting your cervical spine
The following are the primary muscles that attach to your cervical spine:
- Sternocleidomastoid. It passes from behind your ear to the front of your neck, one on each side. It is attached to both your collarbone and breastbone (sternum). This muscle enables you to tilt your chin upward and rotate your head from side to side.
- Trapezius. From the bottom of your brain, through your cervical and thoracic spine, and out to your shoulder blade, located these two triangle muscles. They help with raising your shoulder blade, rotating your head to the left or right, and bending your head forward or backward.
- Levator scapulae. The top of your shoulder blade (scapula) and your first four cervical vertebrae are where this muscle is attached. It supports head rotation, sideways head bending, and shoulder blade elevation.
- Erector spinae. Several muscles make up this muscle group. These muscles support proper posture, rotation of the neck, and extension of the neck backward in the cervical spine.
- Deep cervical flexors. Your cervical spine’s anterior region is occupied by these muscles. Your cervical spine remains stable and you are able to flex your neck forward with their assistance.
- Suboccipital muscles. Your cervical spine’s upper end and the base of your head are joined by these four muscle pairs. They let you turn and extend your head.
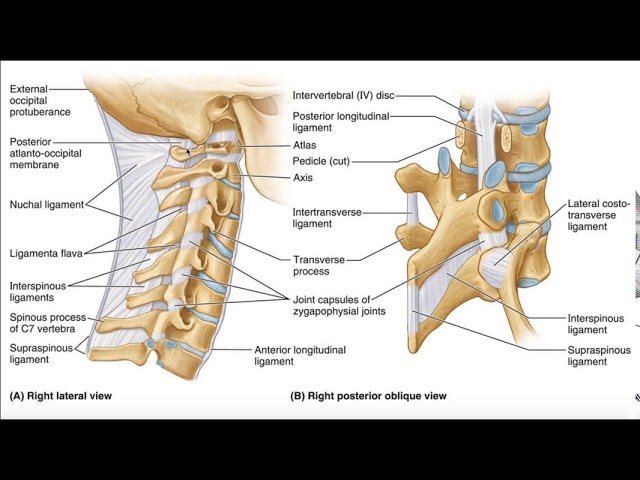
Ligaments of your cervical spine
Your cervical spine’s ligaments serve as a structural support system by joining one bone to another. Three major cervical spine ligaments are:
- Anterior longitudinal ligament. This ligament extends from the base of your skull, down the front of the cervical vertebra. To prevent neck motion backward, it extends.
- Posterior longitudinal ligament. Beginning at C2, this ligament runs the length of your cervical vertebrae. To prevent forward neck motion, it extends.
- Ligamentum flava. The internal opening of each vertebra, where your spinal cord passes, is lined with these ligaments on the back side. Your spinal cord is protected from the back by these ligaments.
Disks in the cervical spine
Situated in between each vertebra, the cervical disks function as “shock absorber cushions”. There are seven cervical vertebrae in total, with one disk between every two vertebrae. Apart from providing support against strains on your neck, the disks facilitate easier head flexion and rotation when engaging in physical activities.
Nerves in the cervical spine
In your cervical spine, there are tiny openings called foramen between each pair of vertebrae via which eight pairs of spinal nerves leave. They’re labeled C1 through C8. In addition to providing feeling, they activate the muscles in your hand, arm, shoulder, and neck.
- Cervical nerves C1, C2, and C3 control your forward, backward, and side head and neck movements. The C2 nerve provides sensation to the upper area of your head; the C3 gives sensation to the side of your face and the back of your head.
- Cervical nerve 4 controls your upward shoulder motion and is one of the nerves that control your diaphragm (muscle at the bottom of your rib cage that helps you breathe). C4 provides sensation for parts of your neck, shoulders, and upper arms.
- Cervical nerve 5: The deltoid muscles in your shoulders and biceps are under the control of cervical nerve root – 5. Your upper arm down to your elbow is sensed by C5.
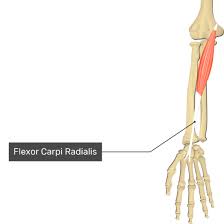
- Cervical nerve 6 is responsible for the extensor muscles of the wrist and biceps. Your hand and forearm’s thumb side are sensed by C6.
- Cervical nerve 7: Your wrist extensor muscles and triceps are controlled by cervical nerve 7. Your middle finger receives feeling from the back of your arm via C7.
- Cervical nerve 8: Your hands are under the control of cervical nerve 8, which also supplies feeling to your forearm and the pinky side of your hand.
Spinal cord
Signals from the brain are transmitted to the body’s other organs by the spinal cord, which is an essential component of the central nervous system. It is composed of nerve tissue that produces reflex control and voluntary movement facilitation, and it is protected by the vertebral column. Depending on how severe and where the injury occurs, spinal cord damage can cause major disabilities or paralysis.
Lower Cervical Spine
While C3–C7, the five cervical vertebrae that comprise the lower cervical spine, are similar to one another, they differ significantly from C1 and C2.
Every vertebral body has two surfaces: a concave superior surface and a convex inferior surface. The uncinate processes, which are elevated processes or hooks on the superior surfaces of the bodies, articulate with the echancrure, also known as the anvil, a depressed region on the inferior lateral aspect of the superior vertebral body.
These uncovertebral joints, also known as the Luschka joints, are especially evident in the vicinity of the pedicles. They are thought to be the outcome of degenerative alterations in the annulus that cause the annulus to fissure and the joint to form. Osteophytic spurs have the potential to constrict the intervertebral foramina in these joints.
While the spinous processes of C7 are often nonbifid and have a somewhat bulbous tip, the spinous processes of C3–C6 are typically bifid.
Anterior and posterior columns
Anterior and posterior columns provide a handy division of the subaxial cervical spine. The normal cervical vertebral body is enclosed in supporting disks to form the anterior column. The anterior longitudinal ligament reinforces the anterior surface, while the posterior longitudinal ligament, extending from the axis to the sacrum, reinforces the posterior body.
Disk-vertebral body articulations, uncovertebral joints, and zygapophyseal (facet) joints are examples of articulations. The uncovertebral joints in the posterior region of the body define the lateral extent of most surgical exposes, and the thicker disk anteriorly contributes to appropriate cervical lordosis.
The joint capsule is thinnest posteriorly and the facet joints are placed at a 45º angle to the axial plane, permitting a sliding motion. The posterior column is further strengthened by the interspinous, posterior, and ligamentum flavum.
Nerve supply
The cervical spine’s neuroanatomy, as depicted in the picture, shows an expanded cord and lateral gray matter extension made up of anterior horn cells. The length is 13–14 mm on the side, and 7 mm is the width from front to back. Cerebrospinal fluid (CSF) is required 1 mm anteriorly and posteriorly in addition to the dura 1 mm. To accommodate the cervical spinal cord, 11 mm is required.
The spinal nerve, which arises from the union of the anterior and posterior nerve roots, exits at each vertebral level.
The foramina gradually get smaller until they reach C6–C7, where they are greatest at C2-C3. 25–33% of the foraminal space is occupied by the spinal nerve and spinal ganglion. The uncovertebral joints border the neural foramen anteromedially, facet joints border it posterolaterally, the pedicle of the vertebra above borders it superiorly, and the pedicle of the lower vertebra borders it inferiorly. The intervertebral discs and the edge of the end plates produce the foramina medially.
There are connections between the spinal nerve proper and the sympathetic nervous system. From C2 to C7, the spinal nerves leave their appropriately numbered vertebral bodies above. There are eight cervical spinal nerves because the numbering of them starts above the atlas. The first one exits between the occiput and the atlas (C1), and the last one exits between C7 and T1.
Vasculature
The paired posterior spinal arteries on the cord’s dorsum and the bigger anterior spinal artery situated in the central sulcus make up the vascular anatomy. It is widely acknowledged that the anterior spinal artery supplies the first two-thirds of the cord, while the posterior arteries provide the last one-third.
Facet Joints
Diarthrodial synovial joints with fibrous capsules make up the facet joints of the cervical spine. In the lower cervical spine compared to other regions of the spine, the joint capsules are more pliable, facilitating the facets’ sliding motion. At 45° from the horizontal plane and 85° from the sagittal plane, the joints are inclined. This alignment is crucial for weight-bearing and aids in preventing excessive anterior translation.
Nerve supply
Mechanoreceptors (types I, II, and III) innervate the fibrous capsules, and free nerve terminals have been discovered in the dense capsular tissues and subsynovial loose areolar tissues. In actuality, the cervical spine has a greater number of mechanoreceptors than the lumbar spine.
In addition to potentially modulating protective muscle reflexes that are crucial for averting joint instability and degeneration, this neuronal input from the facets may be significant for proprioception and pain perception.
Both the anterior and posterior rami innervate the cervical spine’s facet joints. The anterior rami of the first and second cervical spinal neurons innervate the atlanto-occipital and atlantoaxial joints. Two branches of the posterior ramus of the third cervical spinal nerve—a medial branch known as the third occipital nerve and a connecting branch—innervate the C2-C3 facet joint.
One level cephalad and caudad to the joint, the posterior rami medial branches supply the remaining cervical facets, C3-C4 to C7-T1. As a result, the medial branches above and below innervate every joint from C3-C4 to C7-T1. As these medial branches wrap around the waists of the articular pillars, they send off articular branches to the facet joints.
Intervertebral Discs
The spaces between the vertebral bodies of C2–C7 are home to intervertebral discs. Every vertebral body caudad to the axis has an intervertebral disk between them. These disks are made up of two end plates that are connected to the neighboring vertebral bodies, the nucleus pulposus in the center, and the annulus fibrosis around the nucleus. They transfer compressive loads over a range of motion as force dissipators. Because the anterior disks are thicker, they support normal cervical lordosis.
Weight-bearing, stability, and cervical spine motion are all impacted by the intervertebral disks. The collagenous layers (lamellae) that make up the annular fibers are positioned 65–70° from the vertical and alternate in direction with each subsequent layer. Because only half of the lamellae have been positioned to withstand force delivered in this direction, they are therefore susceptible to damage from rotating forces.
Nociceptor innervation occurs in the middle and outer third of the annulus. The disc contains phospholipase A2, which may act as an inflammatory mediator.
Pathophysiology
The kind of injury may be predicted by the force and direction applied.
- Flexion
- Extension
- Rotation
- Lateral bending
- Distraction (stretching)
- Compression (axial loading)
In complicated mechanism injuries, such as high-speed rollover motor vehicle collisions, many forces may be created.
Take note that it could take some time to realize the full extent of the injury.
Initial partial lesions may develop into complete lesions.
In spinal cord injury, many pathophysiologic processes occur. This is because of changed blood flow, vasogenic edema, and free radicals, which cause clinical decompensation.
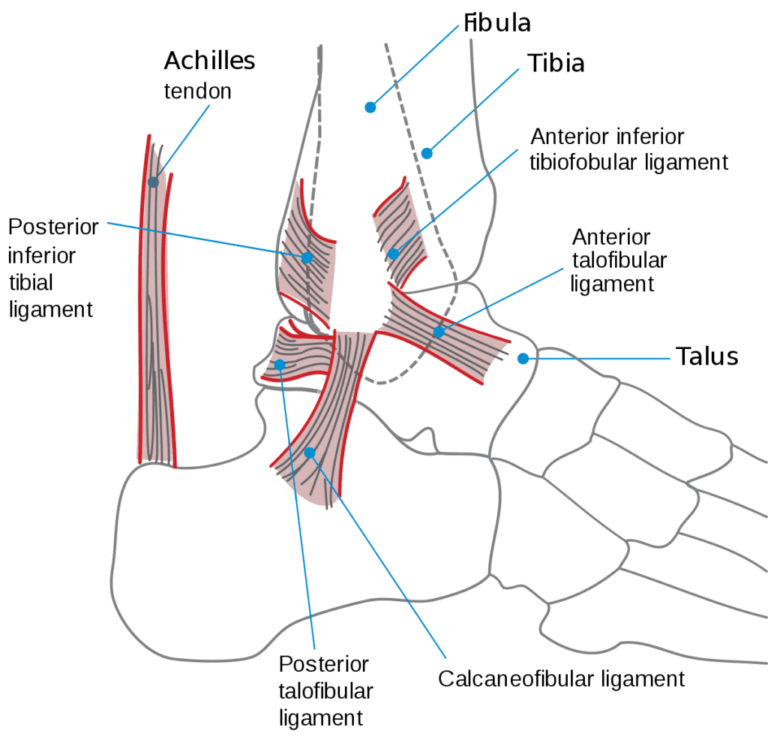
Ligaments
Despite the fact that the cervical spine is made up of seven cervical vertebrae separated by intervertebral disks, the intricate ligamentous network maintains the individual bony components’ appearance and function as one continuous structure.
As said, the anterior and posterior columns make up the cervical spine. Additionally, it can be helpful to consider the following in terms of a third (middle) column:
- The anterior longitudinal ligament, the anterior two-thirds of the vertebral bodies, the annulus fibrosus, and the intervertebral disks make up the anterior column.
- The posterior longitudinal ligament, the posterior third of the vertebral bodies, the annulus fibrosus, and the intervertebral disks make up the middle column.
- The posterior arches, which consist of the pedicles, transverse processes, articulating facets, laminae, and spinous processes, comprise the posterior column.
The spinal column’s structural stability depends on the longitudinal ligaments. A network of ligaments, comprising the nuchal and capsular ligaments as well as the ligamentum flavum, stabilizes the posterior column alignment while the anterior and posterior longitudinal ligaments preserve the skeletal stability of the anterior and middle columns.
The other two columns offer support in the case that trauma disrupts one of the three, thereby preventing cord injury. Spinal cord damage is more likely when two columns are disrupted because the spine may then move as distinct pieces.
Here is a quick description of some cervical spine ligaments that are important for stability and proprioceptive feedback.
Holding the odontoid process (dens) against the anterior arch, the transverse ligament, which makes up the majority of the cruciate ligament, extends across the anterior ring of the atlas from the tubercles. Between the transverse process and the dens lies a synovial cavity. This ligament stabilizes the cervical spine during flexion, extension, and lateral bending and permits the atlas to rotate on the dens. The most crucial ligament in stopping aberrant anterior translation is the transverse ligament.
The ipsilateral medial occipital condyles, the ipsilateral atlas, and the lateral sides of the dens are all connected via the alar ligaments. They permit flexion and extension but inhibit excessive lateral and rotational motion. The joint complex becomes hypermobile when the alar ligaments are injured, as in whiplash, and this can cause the vertebral arteries to twist and mechanoreceptors and nociceptors to become stimulated. This could be connected to the common problems (such as headache, neck pain, and dizziness) that individuals with whiplash injuries experience.
The two main ligaments that stabilize the intervertebral joints are the anterior longitudinal ligament (ALL) and the posterior longitudinal ligament (PLL). Both ligaments are present over the whole length of the spine; in the cervical spine, the ALL is not as well developed as the PLL and attaches to the disks more firmly. At the level of the atlas, the PLL unites with the tectorial membrane, while the ALL becomes the anterior atlanto-occipital membrane. They both proceed to the occiput. Excessive flexion and distraction are avoided by the PLL.
The stability between the vertebral arches is preserved by the ligamentum flavum, supraspinous ligament, and interspinous ligaments. The ligamentum flavum extends from the anterior surface of the cephalad vertebra to the posterior surface of the caudad vertebra, the supraspinous ligament runs along the terminals of the spinous processes, and the interspinous ligaments run between neighboring spinous processes.
Excessive flexion and anterior translation are controlled by the ligamentum flavum and the interspinous ligament, in particular. On the ventral aspect, the ligamentum flavum also joins and strengthens the facet joint capsules. The ligamentum nuchae, which is the supraspinous ligament’s cephalad continuation, is crucial for maintaining the cervical spine’s stability.
Compared to adults, children’s craniocervical junctions differ significantly anatomically. Children’s craniocervical junction instability presents special surgical complications. Although the grounds for cervical fusion are technically identical to those for adults, the use of internal fixation is limited in children due to considerable anatomical abnormalities in the craniocervical junction, which complicate the procedure.
The small bone and ligamentous structures impede treatment and are frequently exacerbated by syndromic craniovertebral abnormalities. Recent developments in imaging have led to better results. Menezes examined 850 kids who had craniocervical fusion surgery. The author provides a thorough analysis of the fusion process in addition to indications, ways to prevent complications, and strategies for managing them.
Differential Diagnosis
- Acute torticollis
- Cauda Equina Syndrome
- Cervical strain
- Hanging injuries
- Neck trauma
- Septic shock
- Spinal cord infection
- Spinal cord injuries
- Spinal cord neoplasms
- Thoracic outlet syndrome
Treatment / Management
According to advanced trauma life support (ATLS) guidelines, administer resuscitation.
- Provide sufficient pain management
- Preserve the immobility of the cervical spine and reduce neck movement, especially when transporting.
- The extent of the injury determines what further care is necessary.
Conservative treatment for minor cervical spine fractures that do not result in neurological impairments can involve pain management, bracing, and follow-up. Surgery can be necessary if the cervical damage is unstable.
Depending on the injury, several surgical procedures may be necessary. It may be necessary to fuse the cervical vertebrae internally using metal plates and screws, or not. Whereas axial fractures frequently need external fixation with a halo, with external pins anchoring the vertebrae, sub-axial fractures are frequently stabilized with internal fixation.
If there is compression of the spinal cord or nerve, surgical excision of a section may be required for decompression of the spine. This may involve a discectomy, laminoplasty, laminectomy, foraminotomy, or other procedures. Decompressing the spinal cord and stabilizing the spine are the primary objectives of treatment.