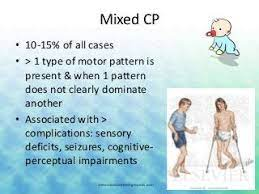
Mixed Cerebral Palsy
Table of Contents
What is mixed cerebral palsy?
- Mixed cerebral palsy happens when a child exhibits symptoms of more than one type of cerebral palsy.
- Children diagnosed with mixed type cerebral palsy have sustained an injury to the motor control centers in several parts of the brain.
- A child’s impairments can fall into both categories, spastic and non-spastic, referred to as mixed Cerebral Palsy.
- The most common form of mixed Cerebral Palsy involves some limbs affected by spasticity and others by athetosis.
- Some people have a combination of symptoms from the different types of Cerebral palsy.
- This is called mixed Cerebral palsy.
- In most cases of mixed Cerebral palsy, people experience a mix of spastic and dyskinetic Cerebral palsy.
- Symptoms of mixed cerebral palsy differ based on the location of movement impairments and the resulting combination of cerebral palsy types.
- These movement problems can happen in the legs (diplegia), one-half of the body (hemiplegia), or all four limbs (quadriplegia).
- Certain cases of brain injuries leading to mixed cerebral palsy are preventable and caused by medical negligence.
- Your family may be eligible to follow legal action if you believe your child’s injuries could have been prevented.
- Mixed cerebral palsy has symptoms of athetoid, ataxic and spastic Cerebral palsy appearing simultaneously, each to varying degrees, and both with and without symptoms of each.
- Mixed Cerebral palsy is the most difficult to treat as it is extremely heterogeneous and sometimes unpredictable in its symptoms and development over the lifespan.
What are the causes of mixed cerebral palsy?
- Brain damage is the main cause of cerebral palsy.
- Injuries to the different motor control centers of the developing brain can lead to different types of cerebral palsy.
Brain damage can be caused by:
- Infections before or after birth,
- Lack of oxygen at birth (hypoxia),
- A stroke suffered during birth,
- Toxic poisoning such as methylmercury,
- Traumatic head injury in first years of life.
- There are multiple risk factors that may increase the likelihood of a baby developing cerebral palsy.
- These involve severe jaundice, placental failure, prenatal or maternal infection, and bleeding in the brain.
Mixed cerebral palsy & types of brain damage
- The main characteristic of mixed cerebral palsy is the presence of brain injury in multiple motor control centers of the brain.
- The area or areas of the brain that are damaged will influence a child’s movement limitations and abnormalities in the brain development.
- A child’s impairments can fall into both categories, spastic and non-spastic, referred to as mixed Cerebral Palsy.
- The most common form of mixed Cerebral Palsy involves some limbs affected by spasticity and others by athetosis.
What Is the most common type of cerebral palsy?
- Spastic is the most common type of cerebral palsy, affecting up to three-quarters of people with a diagnosis.
- Mixed cerebral palsy is the second most common type, while ataxic and dyskinetic types are infrequent.
What Is the most common form of mixed cerebral palsy?
- Of children with mixed cerebral palsy, the most common combination is spastic-dyskinetic.
- These children have rigid muscles, which make it difficult to walk.
- They also struggle to control movements and may have tremors, jerky movements, and struggling grasping objects and stay balanced.
Medical Conditions Associated with Mixed Cerebral Palsy
- Children with any form of cerebral palsy face medical issues certain to each type.
- A child with mixed cerebral palsy could face specific medical problems of 2 or 3 types of cerebral palsy.
- For this reason, treatment of mixed cerebral palsy can be more challenging.
- Like as a child with the spastic quadriplegia form of spastic cerebral palsy is at risk of brain malformations.
- A child with ataxic cerebral palsy will have issues grabbing objects and buttoning shirts.
- A child with both spastic & ataxic is at risk of developing brain malformations & grasping issues.
- Children with mixed cerebral palsy are too at risk of developing seizures, ranging from mild to severe.
- They are too may have issues with swallowing, which could put them at risk for malnutrition.
- Further, children with mixed cerebral palsy are at risk of developing intellectual disabilities, ranging from mild to severe.
Additional Mixed Cerebral Palsy Symptoms
- Because mixed cerebral palsy includes more than one type of brain damage,& because there are so many associated conditions, the number of potential symptoms is extensive.

Additional symptoms of mixed cerebral palsy involve:
- Issues with social interaction and emotional health
- Pain, weakness, fatigue
- Hearing loss and vision problems
- Delayed growth
- Impaired vision
- Drooling
- Incontinence
- Infections
- Learning disabilities
- Dental issues
- Spinal deformities.
- Keep in mind that each child is various.
- While one child may have numerous cerebral palsy symptoms, another child may only develop a few.
What are the earliest signs of mixed cerebral palsy?
- Early interventions are necessary for the best outcome for a child with any type of cerebral palsy.
- But, it can be difficult for parents and even doctors to detect mild and moderate cases right away.
- The sooner you get your child screened for mixed cerebral palsy, the earlier you can start treatments for the best results.
Look for these early signs:
- Delays in what is considered normal development, like as rolling over, sitting, or crawling,
- Un common floppiness or stiffness in arms, legs, or neck,
- Inability to hold up the head,
- Atypical posture or favoring one side of the body.
Is my baby at risk for mixed cerebral palsy?
It is frequently impossible to pinpoint one exact cause of cerebral palsy, yet there are several known risk factors:
- Preterm birth
- Low birth weight
- Multiples (twins or triplets)
- Maternal infection or illness
- Specific maternal medical conditions, involving seizure disorder, developmental disability, and thyroid conditions
- Maternal fever
- Mismatched Rh factor between mother and baby
- Fertility treatments
- Toxic chemical exposure
- Infant seizures
- Infant jaundice
- Complicated labor.
- For acquired mixed cerebral palsy, which happens after birth, risk factors include injuries and not getting childhood vaccinations.
How can I prevent mixed cerebral palsy in my child?
- There is no certain way to prevent cerebral palsy.
- Sometimes it happens with no known risk factors, but there are also risk factors you cannot control.
- Control what you can to lessen the risk our child will develop mixed cerebral palsy.
- Keep up with the doctor appointments throughout pregnancy.
- Keep your child secure from accidents and get all their vaccinations.
- Medical malpractice sometimes causes cerebral palsy, especially during labor and delivery.
- Speak clearly when you feel something is wrong.
- Do not be afraid to ask questions or to request a different doctor or nurse.
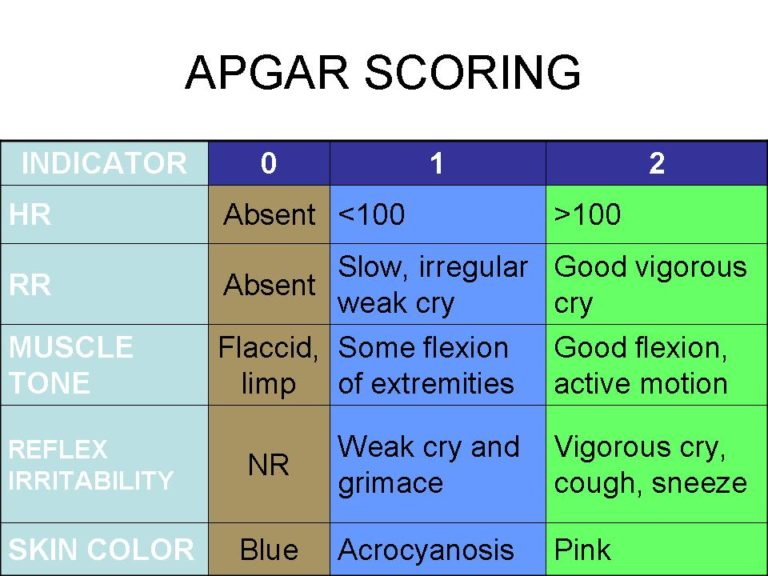
Diagnostic study:
- Physical Assessment.
- Observe LBW, preterm, and those with low Apgar scores at five minutes.
- Observe babies who have seizures, intracranial hemorrhage, and metabolic disturbances.
- Later control of movement does not occur until late infancy, diagnosis may not be confirmed until after six months of age.
Warning signs:
- Physical Signs:
- poor head control after three months,
- stiff or rigid arms or legs, arching back, floppy or limp posture,
- Can’t sit up without support for eight months,
- Uses only one side of the body/only the arms to crawl.
- Behavioral Signs:
- Utmost irritability or crying,
- Failure to smile by three months,
- Feeding difficulties,
- Persistent gagging/choking when fed,
- After six months of age, the tongue pushes soft food outside the mouth.
How is mixed cerebral palsy diagnosed?
- The symptoms of mixed Cerebral palsy depend on whether the damage was sole to the basal ganglia, or if both the cerebellum and basal ganglia were damaged.
- If both areas are damaged, this will probably cause problems with balance and coordination.
- Parents and caregivers usually begin noticing signs of involuntary or jerky movements when their child is around nine months or older.
- In many young children, irregular movement may be indicative of a developmental delay, yet not necessarily a sign of cerebral palsy.
Mixed cerebral palsy is possibly present in a child who:
- Does not kick legs,
- Looks like a stiff or rigid,
- Looks like a limp,
- Does not hold up head at three months old,
- Does not reach for objects,
- Does not smile by three months old,
- Does not roll over.
- Most children with mixed cerebral palsy are diagnosed in the first two years of life.
- Health care providers look for signs of Cerebral palsy if a baby is born early or has another health problem that is associated with Cerebral palsy.
- No single test can diagnose ataxic cerebral palsy.
- So health care professionals see at many things, including a child’s:
- development,
- growth,
- reflexes,
- movement.
Testing may include:
- brain MRI, CT scan, or ultrasound,
- blood and urine tests to check for other medical conditions, including genetic conditions,
- electroencephalography (EEG) to seems at electrical activity in the brain,
- electromyography (EMG) to check for muscle weakness,
- evaluation of how a child walks & moves,
- speech, hearing, and vision testing.
- Our age-specific overviews can give you a sense of how your child might develop from birth to age five.
Development
Your Child’s Development: Newborn
- From the moment babies are born, they respond to the world around them.
- Their reactions — being calmed by a parent’s hug or startled by a loud sound — are examples of normal infant development.
- Doctors use milestones to talk if a baby is developing as expected.
- There is a broad range of what is considered normal, so some babies may gain skills earlier or later than others.
- Babies who were born prematurely may extend milestones later.
- Always talk with your doctor about your baby’s progress.
Here is what your newborn might do:
- Communication and Language Skills
- turns his or her head side of the parent’s voice or other sounds
- cries to communicate a need (to be held/fed, to have a diaper changed, or need to sleep)
- stops crying when a need is met (when picked up, fed, changed, and put down for a nap)
2. Movement and Physical Development
- moves in response to sights & sounds
- rooting reflex: turns the side of the breast or bottle and sucks when a nipple is placed in the mouth
- Moro reflex (startle response): when startled, stretches arms & legs out, then curls them back in
- fencer’s pose (tonic neck reflex): when the head is turned to one side, straightening the arm on that side while bending the opposite arm
- grasp reflex: holds a finger placed in the palm and toes curl when touched on the sole of the foot
3. Social and Emotional Development
- soothed by a parent’s voice & touch
- has periods of the alertness
4. Cognitive Skills (Thinking & Learning)
- looks at faces when quiet & alert
- follows the faces
When Should I Call the Doctor?
- Every child develops at their admit pace.
- But if something concerns you, tell your doctor.
Additionally, tell the doctor if your baby:
- does not suck well at the breast or on a bottle nipple
- has an arm or leg that looks weaker than the other
- is very fussy/hard to soothe.
Your Child’s Development: 3-5 Days
- Though only a few days old, your baby already is able to interact in certain ways.
- When alert, your baby will probably focus on your face.
- Babies are especially drawn to the higher-pitched voices, so give in to that urge to use “baby talk.”
- You are introducing your baby to language & your baby will enjoy it.
- Doctors use milestones to talk if a baby is developing as expected.
- There is a broad range of what is considered normal, so some babies may gain skills earlier or later than others.
- Babies who were born prematurely may extend milestones later.
- Always talk with your doctor about your baby’s progress.
Here is what your newborn might do:
- Communication and Language Skills
- turns his or her head side of the parent’s voice or other sounds
- cries to communicate a need (to be held/fed, to have a diaper changed, or need to sleep)
- stops crying when a need is met (when picked up, fed, changed, and put down for a nap)
2. Movement and Physical Development
- moves in response to sights & sounds
- rooting reflex: turns the side of the breast or bottle and sucks when a nipple is placed in the mouth
- Moro reflex (startle response): when startled, stretches arms & legs out, then curls them back in
- fencer’s pose (tonic neck reflex): when the head is turned to one side, straightening the arm on that side while bending the opposite arm
- grasp reflex: holds a finger placed in the palm and toes curl when touched on the sole of the foot
3. Social and Emotional Development
- soothed by a parent’s voice & touch
- has periods of the alertness
4. Cognitive Skills (Thinking & Learning)
- looks at faces when quiet & alert
- follows the faces
When Should I Call the Doctor?
- Every child develops at their admit pace.
- But if something concerns you, tell your doctor.
Additionally, tell the doctor if your baby:
- does not suck well at the breast or on a bottle nipple
- has an arm or leg that looks weaker than the other
- is very fussy/hard to soothe.
Your Child’s Development: 1 Month
- Have you noticed how your baby’s tiny fingers curl around yours/close into fists?
- how does your small one startle at a loud noise?
- Your baby was born with these and other reflexes, which will get less noticeable as your baby grows.
- Doctors use milestones to talk if a baby is developing as expected.
- There is a broad range of what is considered normal so some babies may gain skills earlier or later than others.
- Babies who were born prematurely may extend milestones later.
- Always talk with your doctor about your baby’s progress.
Here are certain new skills your baby may have:
- Communication and Language Skills
- startles at loud noises,
- makes sounds other than crying.
2. Movement and Physical Development
- keeps hands in tight fists,
- arms and legs move similarly on both sides,
- when lying on the tummy, holds head up shortly.
3. Social and Emotional Development
- recognizes parent’s voice,
- when upset, responds to a parent’s cuddles, voice & affections,
- becomes alert when hearing an affable sound, like music.
4. Cognitive Skills (Thinking and Learning)
- will stare at an object placed in front of the face, specifically something brightly colored,
- follows faces.
When should I call the doctor?
- As your baby becomes more alert, they will watch you constantly.
- And you will be watching your little one closely too.
- So this is an excellent time to watch for any subtle signs that could point to a problem.
Tell the doctor if your baby:
- has one eye that is crossed or eyes that do not line up in the same direction,
- does not respond to pleasing sounds, like as a soft voice or gentle music,
- has legs/hands that do not move in unison: for example, only one leg kicks or just one arm shakes.
Your child’s development: 2 months
- Doctors use milestones to talk if a baby is developing as expected.
- There is a broad range of what is considered normal, so some babies may gain skills earlier or later than others.
- Babies who were born prematurely may extend milestones later.
- Always talk with your doctor about your baby’s progress.
Here are things babies commonly do by this age:
- Communication and Language Skills
- produce sounds other than the crying,
- react to the noisy noises.
2. Movement and Physical Development
- when on their belly, clasp up their head,
- move both arms & both legs,
- open their hands shortly.
3. Social and Emotional Development
- calm down when spoken to and picked up,
- look like your face,
- look happy to see you,
- smile when you talk or smile.
4. Cognitive Skills (Thinking and Learning)
- watch you as you move,
- seems at a toy for several seconds.
When should I call the doctor?
- You know your baby best.
- Share your cares — even little ones — with your baby’s doctor.
- If your baby is not meeting one or more milestones or you notice that your baby has skills yet has lost them, tell the doctor.
Your child’s development: 4 months
- Doctors use milestones to talk if a baby is developing as expected.
- There is a broad range of what is considered normal, so some babies may gain skills earlier or later than others.
- Babies who were born prematurely may extend milestones later.
- Always talk with your doctor about your baby’s progress.
Here are things babies commonly do by this age:
- Communication and Language Skills
- create sounds like ooh and aah (cooing),
- turn their head toward your voice,
- create sounds in response to being spoken to.
2. Movement and Physical Development
- use their arms to swing at the toys,
- bring their hands to the mouth,
- grasp a toy when you put it in their hand,
- grasp their head steady without support when being held,
- push up on elbows or forearms when on their stomach.
3. Social and Emotional Development
- smile to get your attention,
- chuckle (not a full laugh) when you attempt to make them laugh,
- look at you, move or make the sounds to get or keep your attention.
4. Cognitive Skills (Thinking and Learning)
- look at their hands with interest,
- when hungry, open their mouth if a breast or bottle approaches.
When should I call the doctor?
- You know your baby best.
- Share your cares — even little ones — with your baby’s doctor.
- If your baby is not meeting one or more milestones or you notice that your baby has skills yet has lost them, tell the doctor.
Your child’s development: 6 months
- Doctors use milestones to talk if a baby is developing as expected.
- There is a broad range of what is considered normal, so some babies may gain skills earlier or later than others.
- Babies who were born prematurely may extend milestones later.
- Always talk with your doctor about your baby’s progress.
Here are things babies commonly do by this age:
- Communication and Language Skills
- acquire turns making sounds with you,
- blow the raspberries,
- create squealing noises.
2. Movement and Physical Development
- roll from stomach to back,
- push up with straight arms when on their stomach,
- lean on their hand to sit with the support.
3. Social and Emotional Development
- know familiar people,
- enjoy watching in a mirror,
- chuckle.
4. Cognitive Skills (Thinking and Learning)
- put things in their mouth to explore,
- reach to the grab a toy,
- close their lips to show they do not want more food.
When should I call the doctor?
- You know your baby best.
- Share your cares — even little ones — with your baby’s doctor.
- If your baby is not meeting one or more milestones or you notice that your baby has skills yet has lost them, tell the doctor.
Your child’s development: 9 months
- Doctors use milestones to talk if a baby is developing as expected.
- There is a broad range of what is considered normal, so some babies may gain skills earlier or later than others.
- Babies who were born prematurely may extend milestones later.
- Always talk with your doctor about your baby’s progress.
Here are things babies commonly do by this age:
- Communication and Language Skills
- create different sounds like “ba-ba-ba” or “ma-ma-ma”,
- raise their arms to be picked up,
- Movement & Physical Development,
- acquire into a sitting position without any help,
- sit without any support,
- use their fingers to “rake” food toward them,
- pass things from one hand to the others.
2. Social and Emotional Development
- are shy, clingy, or fearful of strangers,
- see, reach for or cry when caregivers leave,
- see when you call their name,
- show several facial expressions, like as happy, sad, angry, and surprised,
- smile/laugh when you play peek-a-boo.
3. Cognitive Skills (Thinking and Learning)
- look for objects when dropped out of sight,
- bang two things together, like blocks.
When should I call the doctor?
- You know your baby best.
- Share your cares — even little ones — with your baby’s doctor.
- If your baby is not meeting one or more milestones or you notice that your baby has skills yet has lost them, tell the doctor.
Your Child’s Development: 1 Year (12 Months)
- Doctors use certain milestones to describe if a toddler is developing as expected.
- There is a wide range of what is considered normal, so some children may gain skills earlier or later than others.
- Toddlers who were born prematurely may achieve milestones later.
- Always speak with your doctor about your child’s progress.
Here are things toddlers commonly do by this age:
- Communication and Language Skills
- call caregiver “mama” or “dada” or another special name,
- waving goodbye,
- understand “no” (pause/stop when you say it).
2. Movement and Physical Development
- pull up to the stand,
- walk holding onto the furniture (cruising),
- with assistance, drink from a cup without a cover,
- pick up things like small pieces of food with their thumb and forefinger.
3. Social and Emotional Development
- play pat-a-cake & other games.
4. Cognitive Skills (Thinking and Learning)
- put something into a container, like a block in a cup,
- look for things that they see someone hide, like a toy under a blanket.
When should I call the doctor?
- You see your child best.
- Participate in your concerns — even little ones — with your child’s doctor.
- If your toddler is not meeting one or more milestones or you notice that your child has skills yet has lost them, tell your doctor.
Your Child’s Development: 15 Months
- Doctors use certain milestones to describe if a toddler is developing as expected.
- There is a wide range of what is considered normal, so some children may gain skills earlier or later than others.
- Toddlers who were born prematurely may achieve milestones later.
- Always speak with your doctor about your child’s progress.
Here are things toddlers commonly do by this age:
- Communication and Language Skills
- point to inquire about something or to get help,
- try to say one or two words (besides “mama” and “dada”), like a “ba” for the ball,
- look at the familiar object when you name it,
- follow directions when given with both a gesture & words.
2. Movement and Physical Development
- take some steps on their own,
- use their fingers to feed themselves.
3. Social and Emotional Development
- show affection to the caregivers with hugs and kisses,
- show caregivers object that they like,
- hug stuffed dolls or teddy bears or other toys,
- similar things doing other children while playing,
- applaud when excited.
4. Cognitive Skills (Thinking and Learning)
- stack at least two small things, like blocks,
- try to use things the right way, like a phone or book.
When should I call the doctor?
- You see your child best.
- Participate in your concerns — even little ones — with your child’s doctor.
- If your toddler is not meeting one or more milestones or you notice that your child has skills yet has lost them, tell your doctor.
Your Child’s Development: 1.5 Years (18 Months)
- Doctors use certain milestones to describe if a toddler is developing as expected.
- There is a wide range of what is considered normal, so some children may gain skills earlier or later than others.
- Toddlers who were born prematurely may achieve milestones later.
- Always speak with your doctor about your child’s progress.
Here are things toddlers commonly do by this age:
- Communication and Language Skills
- try to say three or more words (besides “mama” and “dada”),
- follow one step to the directions said with words & not gestures (“Pick up the toy.”).
2. Movement and Physical Development
- walk without holding on to anyone or anything,
- climb on & off a chair or couch without help,
- drink from a cup without a cover and may spill sometimes,
- use their fingers and maybe a spoon for the eat,
- scribble.
3. Social and Emotional Development
- point to show you something interesting,
- move away from you, yet look to make sure you are close by,
- puts hands out to get them washed,
- help with getting dressed by pushing their arm through a sleeve or lifting up to a foot,
- look at some pages in a book with caregivers.
4. Cognitive Skills (Thinking and Learning)
- copy you doing chores, like as sweeping,
- play with toys in a simple way, like pushing a toy car,
When should I call the doctor?
- You see your child best.
- Participate in your concerns — even little ones — with your child’s doctor.
- If your toddler is not meeting one or more milestones or you notice that your child has skills yet has lost them, tell your doctor.
Your Child’s Development: 2 Years (24 Months)
- Doctors use certain milestones to describe if a toddler is developing as expected.
- There is a wide range of what is considered normal, so some children may gain skills earlier or later than others.
- Toddlers who were born prematurely may achieve milestones later.
- Always speak with your doctor about your child’s progress.
Here are things toddlers commonly do by this age:
- Communication and Language Skills
- say at least 2 words together, like “more milk”,
- point to the things in a picture book when asked (“Where is the dog?”),
- point to a minimum of two body parts when asked (“Where is your nose?”),
- use more gestures, like blowing a kiss or nodding yes.
2. Movement and Physical Development
- run,
- kicking the ball,
- walk (not climb) up some stairs with or without help,
- eat with the spoon.
3. Social and Emotional Development
- notice when others are hurt or upset, like as pausing or looking sad,
- see at your face to see how to react to a new situation.
4. Cognitive Skills (Thinking and Learning)
- grasp something in one hand while using the other, like as holding a container and taking the lid off,
- try to use switches, knobs, or buttons on the toy,
- play with more than one toy at a time, like putting toy food on a toy plate.
When should I call the doctor?
- You see your child best.
- Participate in your concerns — even little ones — with your child’s doctor.
- If your toddler is not meeting one or more milestones or you notice that your child has skills yet has lost them, tell your doctor.
Your Child’s Development: 2.5 Years (30 Months)
- Doctors use certain milestones to describe if a toddler is developing as expected.
- There is a wide range of what is considered normal, so some children may gain skills earlier or later than others.
- Toddlers who were born prematurely may achieve milestones later.
- Always speak with your doctor about your child’s progress.
Here are things toddlers commonly do by this age:
- Communication and Language Skills
- say around fifty words,
- say two or more words together, with one action word, like “doggie run”,
- say words like an “I,” “me,” or “we”,
- address things in a book when you point & ask “What is this?”
2. Movement and Physical Development
- take certain clothes off by themselves,
- jump with both feet,
- use hands to twist things, like turning a doorknob or unscrewing a lid,
- turns pages in a book one at a time.
3. Social and Emotional Development
- play next to other children & sometimes play with them,
- expose you what they can do by saying “Look at me!”,
- follow simple routines when told, like picking up toys when you say “It’s clean-up time.”
4. Cognitive Skills (Thinking and Learning)
- use things to pretend, like feeding a block to a doll as if it were food,
- show simple problem-solving, like using a stool to reach something,
- follow 2-step instructions (“Pick up the toy and put it on the shelf.”),
- know at least one color, like pointing to a red crayon when asked “Which one is red?”
When should I call the doctor?
- You see your child best.
- Participate in your concerns — even little ones — with your child’s doctor.
- If your toddler is not meeting one or more milestones or you notice that your child has skills yet has lost them, tell your doctor.
Your Child’s Development: 3 Years (36 Months)
- Doctors use certain milestones to describe if a preschooler is developing as expected.
- There is a wide range of what is considered normal, so some children may gain skills earlier or later than others.
- Kids who were born prematurely may achieve milestones later.
- Always speak with your doctor about your child’s progress.
Here are things preschoolers commonly do by this age:
- Communication and Language Skills
- say the first name when asked,
- talk with you in conversation with at least two back-and-forth exchanges,
- inquire who, where, or why questions,
- say what action is happening in the picture when asked, like as running, eating, or playing,
- talk well sufficient for others to understand most of the time.
2. Movement and Physical Development
- string items together, like as large beads or macaroni,
- put on certain clothes by themselves,
- use the fork.
3. Social and Emotional Development
- calm down within ten minutes after you leave,
- see other children and join them to play.
4. Cognitive Skills (Thinking and Learning)
- make a circle when you show them how
- avoid touching hot objects, like a stove, when you warn them.
When should I call the doctor?
- You see your child best.
- Participate in your concerns — even little ones — with your child’s doctor.
- If your preschooler is not meeting one or more milestones or you notice that your child has skills yet has lost them, tell your doctor.
Your Child’s Development: 4 Years
- Doctors use certain milestones to describe if a preschooler is developing as expected.
- There is a wide range of what is considered normal so some children may gain skills earlier or later than others.
- Kids who were born prematurely may achieve milestones later.
- Always speak with your doctor about your child’s progress.
Here are things preschoolers commonly do by this age:
- Communication and Language Skills
- say sentences with four or more words,
- say certain words from a song, story, or nursery rhyme,
- speak about at least one thing that happened during the day,
- answer the simple questions, like “What is a crayon for?”
2. Movement and Physical Development
- grab a large ball most of the time,
- assist the serving food; pour drinks with help,
- unbutton certain buttons,
- hold pencil or crayon amid fingers & thumb (not in a fist).
3. Social and Emotional Development
- pretend to be something else during play, such as a teacher, superhero, or animal,
- permission to go play with other children if none are around,
- comfort others who are hurt or sad, like hugging a friend who is crying,
- avoid danger, like jumping from a high playground set,
- likes to be a “helper”,
- changes behavior based on environments, like at a library or playground.
4. Cognitive Skills (Thinking and Learning)
- name some colors,
- talk about what comes next in a well-known story,
- sketch a person with three or more body parts.
When should I call the doctor?
- You see your child best.
- Participate in your concerns — even little ones — with your child’s doctor.
- If your preschooler is not meeting one or more milestones or you notice that your child had skills yet has lost them, tell your doctor.
Your Child’s Development: 5 Years
- Doctors use certain milestones to describe if a preschooler is developing as expected.
- There is a wide range of what is considered normal, so some children may gain skills earlier or later than others.
- Kids who were born prematurely may achieve milestones later.
- Always speak with your doctor about your child’s progress.
Here are things preschoolers commonly do by this age:
- Communication and Language Skills
- describe the story they heard or made up with at least two events,
- answers the easy questions about a story after hearing it,
- keep a conversation going with more than three back-and-forth exchanges,
- use or recognize simple rhymes, like as a bat-cat.
2. Movement and Physical Development
- button certain buttons,
- hop on 1 foot.
3. Social and Emotional Development
- obey rules or take turns when playing games,
- sing, dance, or act for you,
- do simple chores, like clearing the table after eating.
4. Cognitive Skills (Thinking and Learning)
- count to ten,
- name certain letters; name numbers between one and five when you point to them,
- use words about time, like yesterday or tomorrow, morning or night,
- pay attention for 5–10 minutes during activities, like arts and crafts (screen time does not count),
- write certain letters in their name.
When should I call the doctor?
- You see your child best.
- Participate in your concerns — even little ones — with your child’s doctor.
- If your preschooler is not meeting one or more milestones or you notice that your child had skills yet has lost them, tell your doctor.
What is the treatment for mixed cerebral palsy?
- Treatment for mixed cerebral palsy depends on the types & symptoms of cerebral palsy the child develops.
- The most common examples of treatment involve:

- Physical therapy,
- Occupational therapy,
- Medications,
- Recreational therapy,
- Surgery,
- Complementary and alternative treatment,
- Speech therapy,
- Assistive devices, such as wheelchairs and walkers.
- Cerebral palsy is a neuromuscular disorder that currently has no heal.
- Some cerebral palsy treatment options available can improve a child’s daily life, health, and well-being.
Treatment Goals for Cerebral Palsy
- Treatment depends upon the type of cerebral palsy your child has, also the severity of the condition.
- Pediatricians, along with specialists, create a plan with treatment goals individualized to a child’s needs.
Although they may vary depending on the severity of the condition, the general goals of a treatment plan typically involve ways to:
- Manage medical conditions
- Manage and control pain
- Assist with behavior and social interactions
- Promote independence
- Assistance with eating, bathing, and dressing
- Optimize mobility
- Help with education and learning.
Medications
- Some medications help children with cerebral palsy control symptoms, including muscle spasms, uncontrollable limb movements, and seizures.
The most usual medications prescribed for cerebral palsy include:
- Baclofen
- Anticonvulsants
- Botox
- Stool softeners
- Sleep aids.
- Keep in mind that although medication can be successful, certain children will not derive enough benefit from it, and in those instances, surgery may be the next option.
Surgery
- Surgery can help people with cerebral palsy less muscle spasticity, increase flexibility, and gain function.
- However, it is important to note that surgery is not an appropriate option for every child with cerebral palsy, and it also comes with risks.
- Your physician will do a complete history and physical examination to determine if your child could potentially bene from surgery.
- There are various types of surgery for children with cerebral palsy.
- These involve procedures on the feet, ankles, legs, hips, wrists, arms, shoulders, or spine.
- Each child is circumstance is special, and their medical team will tailor a treatment plan to their needs.
- The treatment team may recommend surgery if the benefits exceed the risks that come along with it.
- Certain operations carry the potential to create serious medical complications such as infection, bleeding, and loss of vision.
- It is important to remember that surgery will not cure a child’s cerebral palsy.
- However, it can help make the disorder more manageable, which can significantly improve function in daily activities, school, and home life.
Complementary and Alternative Treatment Options
- Complementary and alternative medicine (CAM) is another modality many parents choose to approach treatment in a longer holistic, natural way.
- The most common types of CAM treatments for cerebral palsy patients involve:
Energy Therapy
- Energy therapy involves manipulating a child’s energy fields to promote energy flow in the body and aid in well-being.
Movement Therapy
- Movement therapy teaches body movements that help promote spiritual, physical, emotional, & mental balance.
Mind and Body Techniques
- Mind and body techniques involve massage, acupuncture, hypnotherapy, guided meditation, guided imagery, yoga, breathing exercises, and more.
Aqua Therapy
- Aqua therapy (also known as aquatic or water therapy) promotes physical function and control, improved muscle tone, confidence, & independence.
Therapies
- Various forms of therapy can provide physical, mental, social, and academic benefits for children with cerebral palsy.
- If started early in a child’s life, many forms of therapy for cerebral palsy can less impairment and the risk of developing other conditions often associated with cerebral palsy.
- Therapy is commonly combined with other treatments, such as medications, surgery, and assistive technology, which further benefit the child.
- When physicians work with families to determine their child’s medical goals, they then develop a particularized treatment plan.
- It is important to note that therapy can also benefit parents and caregivers.
- For example, nutritional therapy can assist caregivers to understand specific dietary needs, while behavioral therapy can teach parents the benefits of positive reinforcement.
The following forms of therapy are the most usual types for children with cerebral palsy.
Physical therapy treatment
- Physical therapy is one of the most important forms of treatment for children with cerebral palsy.
- Most physicians recommend physical therapy for all children with cerebral palsy, nevertheless, of how minor or severe the disorder is.
- Children diagnosed with cerebral palsy will have different degrees of muscle control, balance, and mobility, depending upon how severe the disorder is.
- Physical therapy assists with these issues by assisting children with balance, posture, crawling, climbing, walking, and muscle strengthening.

In addition, physical therapy assists children with cerebral palsy to:
- Overcome physical limitations,
- Increase independence,
- Expand the range of motion,
- Improve muscle tone,
- Decrease the chance of joint contractures and bone deformities,
- Use adaptive equipment,
- Increase fitness, flexibility, balance, and posture,
- Reduce physical discomfort and pain.
OCCUPATIONAL THERAPY

- Occupational therapy assists children improve function when performing daily activities.
- These involve activities in the home, at school or in the community, and later in life, at work.
- This type of therapy assists children in successfully carrying out tasks needing to be accomplished each day.
- A typical occupational therapy session consists of the child being trained and guided by a therapist to work on exercises that will improve function and assist with activities of daily living
SPEECH AND LANGUAGE THERAPY

- Children with cerebral palsy sometimes have trouble forming words correctly.
- Speech and language therapy aims to assist children to understand the language better and communicate more effectively.
- A speech and language pathologist implements strategies and tools to assist the child to communicate successfully.
- They take discrete strengths and weaknesses into account.
- This can be done through sign language, cues, & the use of augmentative communication devices.
- Goals are set for each child who attends speech therapy to assist them to communicate as effectively as possible.
AQUATIC THERAPY

- Aquatic therapy assists a child with cerebral palsy to improve muscle tone and physical functioning.
- It is especially beneficial for children with cerebral palsy who are unable to walk without assistance.
- This type of therapy is an alternative to traditional physical therapy.
- It takes place in water, usually a swimming pool, and combines both aerobic and anaerobic exercises that are easy for children with cerebral palsy to perform.
Aquatic therapy for cerebral palsy can involve different water-based exercises, including:
- Walking (or skipping, galloping, or running) in shallow or deep water
- Aquatic yoga
- Swimming
- Floating
- Motion exercises
- Resistance exercises
- Balance exercises
- Games
- Deep breathing exercises
- Stretching
Benefits of aquatic therapy for cerebral palsy involve improved:
- Gait
- Gross motor function
- Joint range of motion
- Cardiovascular endurance
- Posture
- Balance
- Spasticity reduction
- Circulation
MASSAGE THERAPY

- Massage therapy is extremely beneficial to children with cerebral palsy, as it improves muscle tone and function.
- Research indicates that massage therapy assists children with cerebral palsy by facilitating the lymphatic, musculoskeletal, and circulatory systems.
- It can also assist children to deal with chronic pain due to joint contractures, scoliosis, and spasticity.
PLAY AND SOCIAL THERAPY

- Regardless of disabilities, almost all children enjoy playtime, and play therapy assists them to learn to express themselves better. Although playing tends to be natural & comes easily for most children, those with cerebral palsy may find it a bit more challenging than others.
- Play and social therapy give parents, caregivers, and loved ones the chance to see how the child interacts socially during play.
- This can be extremely beneficial, especially for children who have difficulties with communication.
MUSIC THERAPY

- According to the American Music Therapy Association (AMTA), music therapy assists to establish a therapeutic relationship between the child in therapy and the instructor.
- Additionally, children who participate in music therapy may experience improvements in learning, motivation, relaxation, and language skills.
BEHAVIORAL THERAPY

- Behavioral therapy assists children that are having difficulties with emotions and who act out through inappropriate behavior. Behavior therapy uses positive reinforcement to assist change negative behaviors into more desirable, adaptive behavior patterns.
- Therapists assist children to explore their thoughts, beliefs, and emotions to mediate difficult situations the child is encountering. This helps improve confidence and well-being.
- Physical therapy is one of the most important forms of treatment for people living with cerebral palsy.
- Physical therapists assist children with cerebral palsy improve mobility, balance, flexibility, and muscle strength.
- Most doctors recommend their cerebral palsy patients receive regular physical therapy.
Goals of the Physical Therapy for Children With Cerebral Palsy
- Children diagnosed with cerebral palsy will have varying degrees of muscle control, balance, and mobility, depending upon how severe the disorder is.
- Physical therapy assists with these issues by assisting children with balance, posture, crawling, climbing, walking, and muscle strengthening exercises.
In addition, physical therapy assists children with cerebral palsy to:
- Overcome physical limitations & obstacles,
- Increase independence,
- Assist expand the range of motion,
- Build muscle tone,
- Decrease the chances of bone deformity,
- Learn about the adaptive equipment and how to use them,
- Increase the fitness, flexibility, balance, and posture,
- Reduce physical discomfort and pain.
Physical Therapy Benefits
- There are several benefits of participating in physical therapy, especially for children with cerebral palsy.
- The primary benefits include assisting children to overcome physical limitations that significantly interfere with their daily lives.
- A physical therapist will construct an in-depth treatment plan according to each child’s strengths and weaknesses.
Once the treatment plan is developed, children can benefit from their individualized physical plan, which can assist with side effects of cerebral palsy that may include:
- Muscle atrophy,
- Limited range of motion,
- Loss of joint function,
- Muscle spasticity,
- Pain in muscles and joints,
- Joint inflammation,
- Rigid muscles.
A Typical Physical Therapy Session for the Children With Cerebral Palsy
- Before any child starts physical therapy, an in-depth medical history & physical examination are carried out.
- In addition to the physical examination, a licensed physical therapist will conduct numerous other tests to assess muscle control, functions, and mechanics, like as:
- Range of motion,
- Physical strength,
- Flexibility and balance,
- Endurance,
- Joint integrity,
- Posture,
- Sensory integration,
- Cognitive functioning,
- Reflexes,
- Breathing.
- After, a care plan is created based on the child’s test results.
- A physical therapist will then set goals for the child’s progress & work with the child to meet those benchmarks.
- This commonly means the therapist and their assistants manipulate a child’s body while completing stretches, strength exercises, or games with specific movements or purposes.
- Therapy sometimes includes instructions for exercises, stretches, posturing, and balance to be performed outside the therapy sessions, at home, at school, or at work.
Where Does Physical Therapy Take Place?
- Physical therapy happens in several settings, involving outpatient medical offices or clinics, inpatient rehabilitation centers, specialized physical therapy centers, skilled nursing centers, hospitals, special education classrooms, & the home.
- The number of physical therapy sessions is dependent on several factors.
- The most important of these are prescribed for the treatment of the child.
- Additional considerations involve adaptive equipment used in the treatment and the abilities of a caregiver to provide additional therapy at home.
- Insurance coverage can dictate how often a child attends therapy in a clinical setting.
- In many cases, a physical therapist will prescribe exercises to be completed at the home.
- The physical therapist or an assistant will train the individual with cerebral palsy, the parent or caregiver, and the primary caregivers on how to properly perform exercises at the home.
- Many people with cerebral palsy need walkers, canes, standers, and other assistive devices to aid mobility.
- People with cerebral palsy sometimes need intervention to get around the house, school, and other everyday places.
- The type of assistance needed depends on the severity of the condition and symptoms.
Walkers
- Children with cerebral palsy benefit from many types of low-tech mobility aids, including walkers, canes, gait trainers, and standers.
Non-wheeled walker

- The non-wheeled walker, also known as a basic walker or a standard walker, works by having the child place their hands on the handle of the walker & hold on while taking steps.
- These walkers are more appropriate for children with normal arm strength, although all types of walkers need children to have at least a little upper body coordination and strength.
- The non-wheeled walker has four “legs” that commonly have rubber tips to help prevent slipping.
- Most are height-adjustable.
Two-wheeled walker

- A two-wheeled walker comes with two wheels attached to the front of the walker and an optional resting seat, depending on the model chosen.
- The two-wheeled seated walker is recommended for children who do not have the stamina to stand for long periods.
- Like a non-wheeled walker, the child grasps the handles on the walker while walking, yet wheels make it easier to maneuver around.
- Two-wheeled walkers come in many various sizes for different ages, ranging from toddlers to adults.
- Certain walkers can fold for easy convenience while traveling.
- For children with seated two-wheeled walkers, the seat sometimes doubles as a chair during class time.
Four-wheeled walkers

- Four-wheeled walkers are designed for children who are not quite coordinated enough to handle a standard walker or two-wheeled walker.
- In addition to assisting children to move forward using their weight, four-wheeled walkers improve cadence and velocity and assist reduce the energy used.
- Similar to the other walkers, the four-wheeled walker comes in different sizes for each age stage.
- Certain four-wheel walkers fold up easily for storage and transportation.
Gait trainers
- Gait trainers are similar to four-wheeled walkers in that they also have 4 wheels.
- Gait trainers also come with an attached seat & may be either angled or straight, depending on the needs and mobility of the child.
Canes

- Canes are a type of mobility aid for children who do not have severe symptoms in their legs yet still need added balance and support when getting around.
- Canes are frequently preferred because of their ease of use, both indoors and outdoors, and their versatility.
- Many children with cerebral palsy can participate in sports with the assistance of canes.
- There are many canes explicitly created for children with cerebral palsy.
- The most popular type is the heavy-duty cane with rubber-pronged ends to assist reduce slipping.
- Several canes today are foldable, making it easy for children to put them away while in class or load them easily into a vehicle.
- Canes commonly have adjustable holes through which children slide their arms.
- They can then hold onto the canes’ rubber handles.
- Most canes today are the height-adjustable as well.
Standers
- Children with cerebral palsy who stand for long periods may benefit from using a stander.
- Standers are specifically designed to allow people to stand for short to extended periods of time.
- A stander has numerous benefits to offer, involving:

- Facilitating muscle and bone development,
- Promoting lower extremity use,
- Allowing eye-level interaction with peers,
- Helping develop motor coordination and head control,
- Passive hamstring stretching,
- Improving bowel and bladder function.
There are many types of standers that have been proven beneficial to children with cerebral palsy:
Active Standers: Active standers are a relatively recent development and come with a sit-to-stand option. Children proceed with these standers with their arms, legs, or both.
Mobile Standers: Mobile standers assist children to stand upright, but some come with the option of sit-to-stand. A pulley propels movement in these types of standers, yet some also come with a motorized option.
Multi-position Standers: Multi-position standers permit children to be standing, lying face upward, or lying face down.
Physiotherapy treatment of mixed cerebral palsy
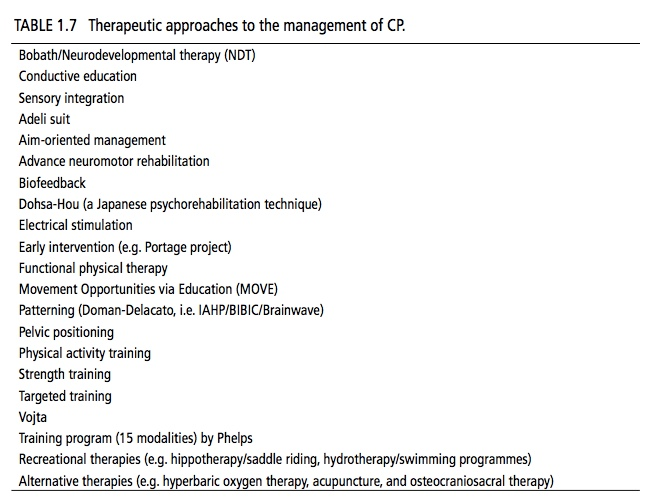
Treatment Approaches for mixed cerebral palsy
- An extensive range of therapeutic interventions has been used in treating and managing children with cerebral palsy.
- They appear that there is evidence to support the use and effectiveness of neuromuscular electrical stimulation, while conformation in support of the effectiveness of the neurodevelopmental treatment is equivocal at best.
- The effectiveness of the many other intercessions, including include: sensory integration, body-weight support treadmill training, conductive education, constraint-induced movement therapy, and hyperbaric oxygen therapy used in the treatment of cerebral palsy have not been clearly accepted based on well-controlled trials.
- We provide an outline of salient aspects of popular approaches and interventions used in the management of children with Cerebral Palsy.
- Identifies an extensive range of choices and availability of various techniques which may vary both between therapists and from country to country.
- The table below lists many of the most common physiotherapy and physiotherapy-related approaches utilized in the management of Cerebral Palsy during the past few decades.
Neurodevelopmental Treatment (NDT)

- One of the more popular approaches utilized in the management of cerebral palsy, the Neurodevelopmental Treatment Approach also known as the Bobath Approach, was developed in the 1940s by Berta and Karl Bobath, based on their particular observations working with children with cerebral palsy.
- The basis of this approach is that motor abnormalities seen in children with Cerebral Palsy are due to uncommon development in relation to postural control and reflexes reason for the primary dysfunction of the central nervous system.
- This approach aims to facilitate typical motor development and function and to fend off the development of secondary impairments due to muscle contractures, and joint and limb deformities.
- Although the effectiveness of Neurodevelopmental Treatment in Cerebral Palsy has been questioned by specific published reports, there are certain studies suggesting its efficacy.
Constraint-Induced Movement Therapy (CIMT)

- Constraint-induced Movement therapy is used predominantly in the individual with Hemiplegic Cerebral Palsy to better the use of the affected upper limb.
- The stronger or non-impaired upper limb is immobilized for a variable duration in order to Force the Use of the damaged upper limb over time.
- Antilla et al (2008) identified one high and one lower-quality trial which measured both body functions and structures, and activity and participation outcomes through the use of Constraint-induced Movement therapy.
- Use of a cast with Constraint-induced Movement therapy showed positive effects in the amount and quality of functional hand use in the impaired limb and new emerging behavior as compared to the no-therapy group, yet no effects were found on QUEST.
- The use of a sling during Constraint-induced Movement therapy also had positive effects on functional hand use on the impaired upper limb, time to complete tasks, and speed and dexterity, yet no effects on sensibility, handgrip force, or spasticity.
- Thus Antilla et al (2005) found there is moderate evidence for the effectiveness of Constraint-induced Movement therapy on functional hand use in the impaired upper limb.
- According to Patel (2005), the success of this approach has not been established, in particular in relation to the adverse effects of lengthened immobilization of the normally developing upper limb.
Patterning for ataxic cerebral palsy
- The concept of patterning is established on theories developed during the 1950s and 1960s by Fay, Delacato, and Doman.
- Patterning is established on the principle that typical development of the infant and child progresses through a well-established, pre-determined sequence; with failure to typically complete one stage of development causing impediment or impairment in the development of subsequent stages.
- Established on this principle they suggested that in children with Cerebral Palsy typical motor development can be facilitated by passively repeating and putting the child through the sequential steps of typical development, a process called patterning.
- Parents and other caregivers are taught to carry out this patterning process at home yet the approach is hugely labor-intensive and time-consuming as it requires multiple sessions every day.
- Although Patterning has been utilized for many years of its use is now surely controversial and its effectiveness has not been established.
- It is a very passive therapy, with a small opportunity to encourage the child in their active involvement and its use in children with Cerebral Palsy is not recommended.
Exercises :
- Exercises for cerebral palsy are geared toward treating either high or low muscle tone.
- High muscle tone causes stiffness and spasticity, whereas low muscle tone causes too much flexibility and weakness.
Improving muscle tone :
- Flexibility exercises and massages are often used for children with spastic cerebral palsy;
- These exercises not only help improve mobility but also can prevent painful muscle tightening that could require surgical correction.
- Strength training exercises are used to increase muscle tone in children with athetoid cerebral palsy.
Assisting posture and walking :
- Special exercises are also used to help with walking, posture, transitional movements, and sensory impairments like touch and balance.
- Posture is improved through exercises that emphasize sitting, kneeling, and standing.
- Transitional movements are those used by infants that lead to walking, such as rolling over and sitting up.
Equipment :
- Physiotherapists use a range of mobility aids to make therapy more effective.
- Braces, casts, splints, and shoe inserts are types of orthotic equipment used to help with walking, posture, and joint mobility.
- Exercise balls
- Resistance bands
- Free weights
- Swimming pools
- Hot and cold packs
- Electric muscle stimulation
- In some cases, electric stimulation is used to improve gait and upper limb function. This therapy uses small electrodes to stimulate certain muscles.
Physiotherapy by Age :
- As children get older, their physiotherapy needs to change.
- Physiotherapists have to adjust and adapt treatments at different stages in development. T
- The most important stages are when the child is a toddler and in the early school years.
Toddlers :
- Therapy for toddlers tends to focus on playtime.
- Children in early developmental stages learn and experience a lot through play, making it an important aspect of early therapy.
- Toddlers with Cerebral palsy are often reluctant to touch their faces or practice certain movements that are necessary for learning and physical development.
- A therapist can help children overcome this reluctance.
- Young children – During school age, roughly ages 5 to 12, children with cerebral palsy experience new movement issues in part because their bodies are growing.
- Physical therapy can help ensure children grow in a way that is conducive to their motor function.
- Exercises and orthotics are most commonly used at this age.
- Therapy also helps instill healthy habits and a proactive mindset.
Therapeutic Interventions
Passive Stretching for mixed cerebral palsy

- It is a manual application for spastic muscles to relieve sloppy tissue tightness.
- Manual stretching may increase the range of movements, decrease spasticity, or improve walking efficiency in children with spasticity.
- Stretch may be applied in a number of ways during neurological rehabilitation to attain different effects.
The types of stretching used include:
- Fast or Quick
- Prolonged
- Maintained
- When we look at the use of a stretch for facilitation, we employ a fast or quick stretch.
- The fast or quick stretch produces a relatively short-lived contraction of the agonist’s muscle and short-lived inhibition of the antagonist muscle which facilitates a muscle.
- It achieves its effect along stimulation of the muscle spindle primary endings which result in reflex facilitation of the muscle along the monosynaptic reflex arc.
- The presence of increased tone can ultimately first to joint contracture and changes in muscle length.
- When we look at the use of stretch to normalize tone and maintain soft tissue length we employ a steady, prolonged stretch to maintain or stop the loss of range of motion.
- While the effects are not wholly clear the prolonged stretch produces inhibition of muscle responses which may help in reducing hypertonus, for example, Bobath’s neuro-developmental technique, inhibitory splinting, and casting technique.
- It appears to have an influence on both the neural components of muscle, along the Golgi Tendon Organs and Muscle Spindles, and the structural components in the long term, along with the number and length of sarcomeres.
- Muscle Immobilised Shortened Position = Loss of Sarcomeres and Increased Stiffness related to enlargement in connective tissue.
- Muscle Immobilised Lengthened Position = Increase Sarcomeres.
Manual Stretching for mixed cerebral palsy
- Prolonged physical stretch may be applied manually, using the effect of body weight and gravity, or mechanically, using machines or splints.
- Stretch should provide enough force to overcome hypertonicity and passively lengthen the muscle.
- Unlikely to provide enough stretch to cause a change in a joint that already has contracture.
Weight Bearing for mixed cerebral palsy
- Weight-bearing has been reported to reduce contracture in the lower limb through the use of Tilt-tables, and standing frames via a prolonged stretch.
- Angles are key to making sure the knees remain extended during the prolonged stretch as the force exerted on the knee can be quite high.
- Certain research also challenges the assumption of the benefits of prolonged standing.
- Splints and casts are exterior devices “Splints and casts are external devices designed to apply, distribute or remove forces to or from the body in a controlled manner to perform one or both basic functions of control of body motion and modification or prevention in the shape of body tissue.”
- Splinting can be used to produce low-force, long-duration stretching although there is a deficiency of evidence to support this.
- A wide range of splints has been used to influence swelling, resting posture, spasticity, and active and passive Range Of Motion (ROM).
- A systematic review suggested that Lower Limb Serial Casting increased ankle dorsiflexion passive range of motion, reduced hypertonicity, and improved gait in children with Cerebral Palsy.
Splinting for mixed cerebral palsy

- Serial casting is a usual technique that is used and is most effective in managing spasticity-related contracture.
- Serial casting is a specialized technique to give an increased range of joint motion.
- The process requires a joint or joints that are tight, which are immobilized with a semi-rigid, well-padded cast.
- Serial casting requires the repeated applications of casts, typically every one to two weeks as the range of motion is restored.
- The duration of the stretch to reduce both spasticities and prevent contracture is not clear from the research and requires further research to determine the most appropriate technique and duration to produce the required effect.
Static Weight-bearing Exercises for mixed cerebral palsy
- Stimulation of antigravity muscle strength, the precaution of hip dislocation, reduction in spasticity, and improvements in bone mineral density, self-confidence, and motor function have all been achieved through the use of Static Weight-Bearing exercises like as Tilt-Table and Standing Frame.
Muscle Strengthening Exercises
- It aims to increase the power of fragile antagonist muscles and of the corresponding spastic agonists and to provide the functional benefits of strengthening in children with Cerebral palsy.
- It increases to power of weak muscles and provides strengthens muscles in cerebral palsy children.
Functional Exercises for mixed cerebral palsy
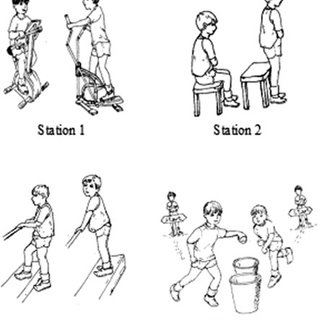
- Training related to specific functional activities combining aerobic and anaerobic capacity and strength training in ambulatory children has been shown to significantly increase overall physical fitness, the intensity of activities, and quality of life.
- Training programs on static bicycles or treadmills have been shown to be beneficial for gait and gross motor development yet have not shown to have any impact on spasticity or abnormal movement patterns.
- A study suggests the application of plyometric exercises to the physical rehabilitation programs of children with unilateral Cerebral palsy could achieve more significant improvement in muscle strength and walking performance.
Body Weight Supported Treadmill Training for mixed cerebral palsy

- Stepping movements from Reflex Stepping Reactions are normally present in newborns and infants, in front of the infant starts to bear weight, stand and walk.
- Body Weight Supported Treadmill Training, is achieved through supporting the child in a harness on the treadmill in an upright posture limiting overall weight-bearing, on a steady moving treadmill, and eliciting the stepping movements.
- Treadmill training consequently allows the development of stepping movements needed for ambulation.
- Studies using 3-4 sessions per week lasting for 3-4 months have shown an increase in the lower extremity movements and gait patterns in children with cerebral palsy.
Electrical Stimulation for mixed cerebral palsy
- The goal of electrical stimulation is to improve muscle strength and motor function. Electrical stimulation is given by Transcutaneous Electrical Nerve Stimulation (TENS) Unit which is portable, non-invasive, and can be used in the home setting by parents or the patient.
- Neuromuscular Electrical Stimulation (NMES) requires the application of transcutaneous electrical current that results in muscle contraction.
- Neuromuscular Electrical Stimulation has been postulated to increase muscle strength by increasing the cross-sectional area of the muscle and by increasing the recruitment of type two muscle fibers.
- Functional Electrical Stimulation (FES) mention to the application of electrical stimulation during a given task or activity when a specific muscle is expected to be contracting.
- Patel (2005) has shown there is certain evidence to support the use and effectiveness of Neuromuscular Electrical Stimulation in children with Cerebral Palsy yet found that many of the studies are limited by confounding variables including concomitant use of other therapies, broad variation in methods of application, heterogeneity of subjects, difficulty in measuring functional outcomes and less of control subjects.
- Mintaze (2009) proposes that neuromuscular and threshold electrical stimulation as a modality in Cerebral Palsy is used for strengthening the quadriceps muscles in ambulant diplegic children with Cerebral Palsy, who have difficulty with specific resistive strength training.
Gait Training

- kids with cerebral palsy at physical therapy to increase walking.
- Gait training is a type of physical therapy that focuses specifically on increasing walking functions.
- Many individuals with cerebral palsy may walk with an abnormal gait due to spasticity in the legs. During gait training, a physical therapist may focus on improving walking speed or correcting walking form.
- Correcting abnormal gait patterns is required because the poor form can ultimately compromise function and potentially lead to the development of chronic pain.
- Gait training may involve the use of equipment like walkers, bodyweight supporting treadmills, and parallel bars to help individuals practice walking without losing stability.
- Additionally, a PT may recommend wearing orthotics like a leg brace to support correct musculoskeletal alignment and gently stretch spastic muscles.
- Gait training focuses on increasing the functions like:
- walking speed
- walking endurance
- gross motor function
- step length
Hippotherapy

- Gross Motor Function including Muscle tone, Range of Movement, Balance, Coordination, and Postural Control in Children with Cerebral palsy has been shown to improve with Hippotherapy – Therapeutic horseback riding which may decrease the degree of motor disability.
- Many none physical benefits may also be developed via enjoyment and providing a setting for increased social interaction, and cognitive and psychosocial development.
- Sharan et al (2005) have noted satisfactory results with Hippotherapy in Bangalore, especially the post-surgical rehabilitation.
- There is limited evidence available with two lower-quality trials on saddle riding on a horse that found no connecting-group differences in muscle symmetry or in any of the seven different outcome measures, excluding the sub-item of grasping.
Sensory Integration Training for mixed cerebral palsy

- Sensory integration therapy is based on the idea that certain kids experience “sensory overload” and are oversensitive to certain types of stimulation.
- When children have sensory overload, their brains have trouble processing or filtering lots of sensations at once.
- Meanwhile, other children are under-sensitive to certain kinds of stimulation.
- Children who are under-sensitive don’t process sensory messages quickly or efficiently.
- These children may notice disconnected from their environment.
- In either case, children with sensory integration issues scuffle to organize, understand, and respond to the information they take in from their surroundings.
- Sensory integration therapy reveals children to sensory stimulation in a structured, repetitive manner.
- The theory behind this treatment approach is that, over time, the brain will adapt and permit them to process and react to sensations more efficiently.
- In this concept, struggling in planning and organizing behavior are attributed to problems in processing sensory inputs within the Central nervous system, including vestibular, proprioceptive, tactile, visual, and auditory.
- Children with sensory integration dysfunction regularly use different sensory combination strategies.
- Treatment centers on the integration of neurological processing by facilitating the individual to process the type, quality, and intensity of sensation.
Games and Activities for mixed cerebral palsy
- When working with children, physical therapists may employ fun games and activities in addition to exercises to inspire the carryover of skills learned in therapy to a child’s daily life.
- This may include using obstacle courses, balance games, or even employing technology like Wii Fit.
- Ultimately, the key to increasing motor functions is to keep moving.
- Teaching children a fun, engaging activities that they can play at home can be an effective way to promote movement outside of physical therapy sessions and improve the carryover of skills and improvements.
- Arts and Crafts
- Adaptive Sports
- Board Games
- Karaoke(singing)
- Music Glove
- Photography
- Horseback Riding
Horseback riding is one of the best activities for kids with cerebral palsy because it encourages:
- Balance,
- Strength,
- Posture,
- Coordination,
- Range of motion.
- Swimming
- Swinging
- Hula Hooping
- Dance Party
Certain examples of songs with hand motions or dance moves include:
- Hokey Pokey,
- Head, Shoulders, Knees, and Toes,
- Hand Jive,
- Cha Cha Slide,
- Cupid Shuffle,
- Macarena.
- Hand-Clapping Games
The corresponding hand motions usually involve repetitive:
- Bending and straightening of the elbows,
- Accuracy to clap your partner’s hands,
- Wrist range of motion,
- Opening and closing of the hands.
Examples of hand-clapping games involve:
- Miss Mary Mack,
- Down by the Banks of the Hanky Panky,
- Slide,
- Lemonade,
- I Went to a Chinese Restaurant.
- Hot Lava
- This game will help your child control where they place their steps and encourage balance.
14. Darts
Playing with darts is a fun, challenging activity that can assist kids with cerebral palsy practice:
- Gripping smaller objects,
- Timing when to let go,
- Aiming,
- Bending and straightening their elbow,
- Wrist movements.
- Create a Secret Handshake
Task-oriented approach for mixed cerebral palsy

- This treatment is established on the requirements of the child.
- Today the child is given the possibility to be further an active problem solver (instead of, as previously, a passive recipient of treatment) in the context of the day-to-day environment.
- The aim of this therapy for children with Cerebral palsy, as for most children with developmental disabilities, is to facilitate the child’s participation in everyday life situations, for example, to communicate with parents, siblings, and peers; to proceed from one place to another; to dress and undress; to eat, and to play.
- The choice of goals for therapy is supported by many factors: the child’s liking and the family’s preferences, the society and environment in which the family lives, and the child’s degree of disability.
- Consequently, it is important to integrate principles of motor learning into the treatment concept and adapt the principles to the prerequisites of each specific child.
- The regulated goals should be specific, measurable, attainable, relevant, and timed (SMART).
Conductive Exercise

- Conductive education (CE) is a combined educational and task-oriented approach for children with Cerebral palsy.
- Specially instructed ‘conductors’ give education to homogeneous groups of children with motor disorders.
- These proceeds have their origins in learning theory.
- The conductor who is trained in all aspects of motor and cognitive development structures the activities, especially the self-care activities.
- The emphasis of interference is on independence in attaining goals rather than on the quality of movement.
Bimanual Training

- Bimanual Training (BIT) provides bimanual training activities, which focus on increasing the coordination of both arms using structured tasks in bimanual play and functional activities with intensive practice.
- Recently has an exhaustive bimanual training program, the hand-arm bimanual exhaustive training (HABIT) been published to substantiate its effectiveness.
- This approach is founded on motor learning theory (practice specificity, types of practice, and feedback), neuroplasticity (i.e., the potential of the brain to change by repetition, increasing movement complexity, motivation, and reward), and focuses on the same use of both arms in bimanual tasks.
- Intensive Bimanual training (e.g., HABIT), was developed with the recognition that increased functional independence in the child’s environment needs the combined use of both hands.
- It as well as focuses on improving coordination of the two hands using structured task practice embedded in bimanual play and functional activities.
- Hand-arm bimanual intensive therapy including lower extremities (HABIT-ILE) integrates upper and lower bilateral extremity training.
- Usually used bilateral lower extremity tasks are ball sitting, standing, balance board standing, virtual reality (Wii-fit, Kinect), walking/running, jumping, cycling, and making scooters.
- Bimanual activities that require trunk and lower extremities postural adaptations are performed at a table of appropriate height (50% of the time) on unstable supports: sitting on fitness balls or standing on balance boards.
- Moreover, 30% of the time is devoted to activities of daily living where standing and/or walking is required (dressing, brushing teeth, doing one’s hair, transporting objects such as a tray, and household chores like as sweeping and washing dishes).
- Finally, the remaining time (20%) is spent in gross motor physical activities/play, like bowling, ball playing, jumping rope, street hockey, use of Wii-fit, balance bike (without pedals), scooter use, and wall climbing.
- These are performed in standing, walking, and running (or jumping) with the lower extremities and simultaneously involve bimanual coordination.
- These activities are graded toward more demanding tasks for the lower extremities.
Robot-assistive therapy for mixed cerebral palsy

- Robot-assisted therapy (RAT) is conducted using robotic devices that allow the patients to perform specific limb movements.
- The foremost interest in using robots is to allow the patients to achieve a large amount of movement in a limited time.
- Additionally, the attractive human-machine interface has the capacity to motivate the child to perform his or her therapy via playful games, like car races, or to perform exercises that mimic activities of daily living.
- Moreover, robotic devices permit the patient to receive visual, auditory, or sensory feedback.
- A device specifically developed for locomotion training is the Lokomat (Hocoma, CH), made of 2 active orthoses, a weight-bearing system, and a treadmill.
- This robotic rehabilitation has been proposed to increase walking and physical fitness.
Virtual reality for mixed cerebral palsy

- Virtual reality has been defined as the use of interactive simulations created with computers to perform users in virtual environments that appear, sound, and feel the same as real-world objects and events.
- Virtual reality can improve the patient’s motivation and achievement in activities of daily living.
- Preliminary data suggest that this type of therapy also improves motor function in the upper and lower extremities that are caused by Cerebral palsy.
State of the Evidence
- Novak et al. (2013) have developed a chart founded on their Systematic Review, which looked at the State of the Evidence in relation to Interventions for the management of children with Cerebral Palsy, to help with comparative clinical decision-making amongst intervention options for the same desired outcome.
- They charted the interventions using bubble charts, with the size of the circle correlated to the volume of published evidence.
- The circle size was calculated using;
The number of published papers on the topic:
- Entire score for the level of evidence (calculated by reverse coding of the Oxford Levels of Evidence, for example, expert opinion=1, randomized controlled trial [RCT]=5).
- The location of the circle on the Y-Axis of the graph correlates to the GRADE System Rating.
- The Colour of the circle corresponds to the Evidence Alert System.
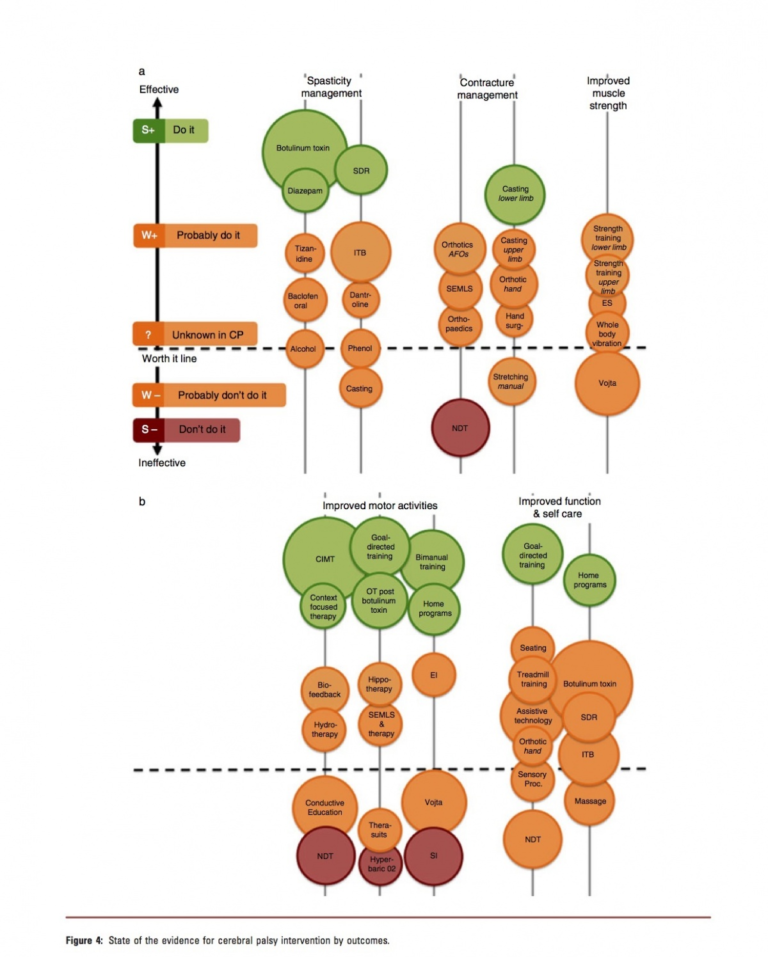
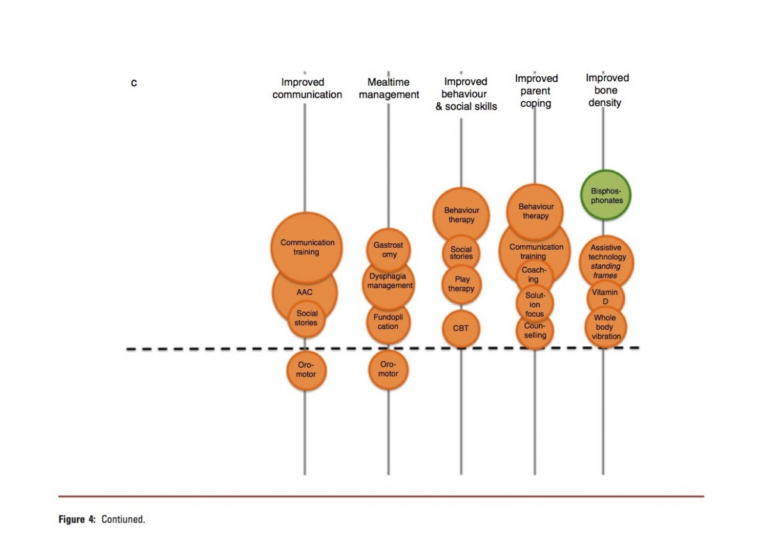
Neuropsychology for cerebral palsy:
- Cerebral Palsy is a long-lasting condition and affects people of all ages.
- Coming to terms with the symptoms and mislaying of independence at any age is a challenge.
Our clinical neuropsychologists can help to provide:
- Detailed assessment of a client’s functioning in specific to their cognition, behavior, and emotional state.
- Providing advice, consultation, teaching, and supervision to other professionals also family and carers.
- Management and guidance for anxiety and changes in mood.
Orthotics for cerebral palsy


- Orthotics may be an everyday requirement that often needs re-adjusting as the person grows.
- Our specialist orthodontist can help by designing, fitting, and altering orthoses to satisfactory complement your treatment and rehabilitation.
These include:
- Orthotics to fend off foot drops and aid walking,
- Night and day resting splints to prevent alignment and prevent contractures,
- Insoles to make better alignment, proprioception, and gait,
- Variation to shoes to assist with leg length discrepancies, alignment, and improved mobility.