Vertebral Artery Test
Table of Contents
Definition/Description
- The vertebral artery test (VAT), used in physical therapy, measures the amount of blood flowing via the vertebral arteries into the brain while looking for signs of illness or insufficiency of the vertebral arteries.
- The test maneuver results in a narrowing of the vertebral artery’s third division, which reduces blood flow to the contralateral side’s intracranial VA. Ischemic stroke is caused by blood loss in the brain’s pons and medulla oblongata. Patients with vertebrobasilar insufficiency (VBI) experience dizziness, nausea, syncope, dysarthria, dysphagia, alterations of the hearing or vision, paresis, or paralysis.
Clinical Anatomy
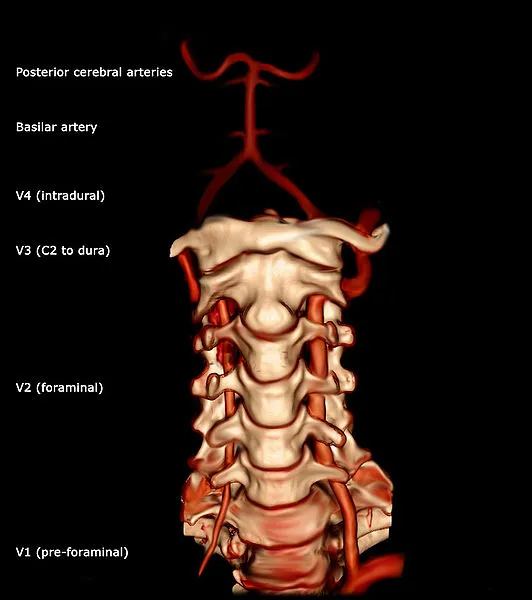
- Vertebral arteries are important neck blood vessels. It comes from the posterosuperior section of the subclavian artery, where it divides from the subclavian artery. It passes through the transverse processes of the sixth cervical vertebra’s foramina as it ascends. It then curves behind the atlas’ superior articular process. It enters the skull through the foramen magnum, where it joins the basilar artery (near the lower edge of the pons) with the opposite vertebral artery to create the basilar artery.
- Four divisions exist within the vertebral artery: Between the longus colli and the m. scalenus anterior, the first division runs posterocranially. another name for the first division is “pre-foraminal division.” The cervical vertebrae C2’s second branch passes via the foramina in the cervical transverse processes. The term “foraminal division” also applies to the second division. The portion rising from C2 is referred to as the third division. On the medial side of the rectus capitis lateralis, it rises from the latter foramen and turns behind the superior articular process of the atlas. Once within the spinal canal, it rests in the groove on the upper surface of the atlas’ posterior arch and passes directly below the posterior atlantooccipital membrane. The fourth segment medially slopes to the front of the medulla oblongata after piercing the dura mater.
Purpose
- The vertebral artery test measures the blood flow via the vertebral arteries while looking for indications of insufficiency.
- An approaching stroke may be signaled by a transient ischemic attack (TIA), which is caused by a decrease in blood flow. It might suggest that there is a danger of missing the chance to avoid lasting impairment or even death if the condition isn’t soon recognized or that there is a risk of inflicting permanent disability or even death if the cervical spine is positioned in a vulnerable posture.
- According to Johnston et al, there is a 10% chance of having a stroke 90 days after having a transient ischemic attack. Within the first two days following a TIA, 50% of these strokes take place. As a result, it’s crucial to take someone with a positive test result to the hospital so that they may undergo further testing. As a migraine, seizure, peripheral neuropathy, or anxiety attack, TIA is frequently misdiagnosed.
Technique
- Before doing a passive evaluation, the cervical spine is typically moved through its active range of motion.
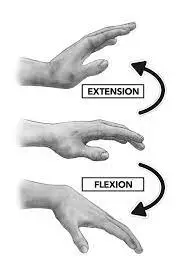
- Position the patient in the supine position and passively extend and flex the neck and head to the side.
- Turn your neck passively to the same side while maintaining the position for around 30 seconds.
- Repeat the test while looking at the opposite side.
- If there is a dip in the arms, a loss of balance, or pronation of the hands, the test is deemed positive; this shows that the brain is receiving less blood.
Modification
- Maximally rotate the head on the side that was being examined, then hold that posture for 10 seconds.
- Spend ten seconds in neutral. for 10 seconds, extend the head
- Spend ten seconds in neutral.
- 10-second maximum head extension and rotation (in the direction of the side that wasn’t tested.
The alternative vertebral artery test is shown below, it may be used in specific cases. For example, in the examination of an individual with supposed BPPV.
Evidence
For the past 30 years, people have been using this test. A number of researchers have noted a decrease in the lumen, however many of these studies are insufficient due to the scarcity of excellent samples of healthy individuals and VBI patients over a range of ages. Vertebral artery testing (VAT) has not been regularly developed as a clinical test for VBI, according to research on the procedure and differential diagnosis in patients who reported dizziness.
Today’s publications have a lot of inconsistencies. Mitchell et al. found that of the 20 studies looked at, four analyzed blood flow in the transverse area of the VA (first division), eleven in the second division, none in the third division, and five in the fourth division. No blood flow loss in the VAI was seen in 7 of the 20 examinations. There will be inaccurate positive/negative blood flow results in cervical spine rotation due to inconsistencies in the literature.
Clinical Importance
Physiotherapists should be aware of the following facts in relation to the help encouraging testing for VBI
The tests themselves are suggestive and hence preserve some intrinsic hazard. However, any possible harm to the patient will be decreased if it is carefully chosen and carried out (including just to the beginning point of stimulation of symptoms). When symptoms or indications are induced during testing, the physiotherapist should be warned of the need for additional care when deciding the course of inquiry and therapy.
The optimal tests are the most valid test for deciding if VBI actually exists and whether the collateral circulation described in the literature up to this point is adequate. Even though the tests’ effects on variations in the vertebrobasilar arterial blood flow in functional investigations have been incompatible, it seems that end-range rotation is the cervical position’s simplest rotation. A recent study has also determined that blood flow changes in the simulated manipulation position.
Physiotherapists should be aware of this while inspecting or treating the cervical spine because there is no relatively simple clinical way for defining the intrinsic level of the vertebral artery. The suggested tests will not specify all patients at risk of suffering an adverse event following cervical manipulation or mobilization.
VAT is recommended to evaluate cervical positional toleration. In order to rule out VBI, the patient should be referred for additional diagnostic procedures if the test is positive.
Vertebrobasilar Insufficiency (VBI) can be present in a patient who does well on the vertebral artery test, but it cannot be ruled out in those who perform poorly.
FAQ
The “5 D’s” (dizziness, diplopia, dysarthria, dysphagia, drop attacks, nausea and vomiting, sensory alterations, nystagmus, etc.) are examples of positive symptoms.
If the hands pronate, the arms droop, or there is a loss of balance, the test is considered positive; this shows that the brain’s blood supply has been reduced.
The patient must be allowed to sitting position and have his or her eyes open. The blood flow’s initial speed in the posterior cerebral arteries is seen within 1-2 minutes. The patient is then instructed to move his head as far to the left as possible, toss it back, and hold it there for 15 to 20 seconds.
Arteriography (or angiography), the gold-standard test for VBI, is invasive and dangerous, especially in aging people, as a result, the dangers of arteriography might outweigh the possible benefits.
When the blood supply to the back of the brain decreases or stops, it is known as vertebrobasilar insufficiency (VBI). The areas of your brain that manage balance and movement are affected by VBI. Many VBI sufferers only experience mild health issues. However, VBI increases your chance of having a stroke or transient ischemic attack (TIA, or mini-stroke).