Ober’s test
Table of Contents
Introduction
Ober’s test is commonly used in hip orthopedic exams to identify tightness of the Tensor Fascia Lata (TFL) or contractures of the Iliotibial Band (IT Band) that limit hip adduction. It is often used to diagnose iliotibial band syndrome. The Ober test, first described by Ober (1936), is a common and widely accepted test for measuring iliotibial band (ITB) length.
The ITB, also known as the iliotibial tract, is a lateral thickening of the fascia lata of the thigh, connected mainly to the upper part of the ilium and the lateral tubercle of the tibia, the head of the fibula, the lateral condyle of the. hip femur and lateral patella retinaculum inferior.
The ITB is also continuous with the lateral intermuscular septum of the thigh, which is anchored to the femoral shaft. The gluteal muscles and tensor fascia lata muscles insert into the ITB, which can be considered the tendon of these muscles.
Ober’s test is performed on the lower limb (upper part) on the patient’s side. The examiner stands behind the patient and moves the thighs of the examined limb into flexion, abduction, and extension positions. Stabilizing the pelvis with one hand, the examiner lowers the limb into adduction until it stops until the pelvis begins to tilt downward, or both. The length of the ITB is then indicated by the angle of hip abduction or adduction relative to the neutral position (0°) (Kendall et al., 1993).
Involved Structures
- Tensor fascia lata
- Iliotibial band
- Gluteus medius
- Gluteus minimus
- Hip joint capsule
What is Iliotibial Band Syndrome (ITBS)?
Iliotibial band syndrome is when a tendon called the iliotibial band becomes irritated or swollen when it irritates against the hip or knee bones. The tendon is located on the outside of your leg and runs from the top of your hip bone to your knee. It irritates the bones when it is too tight (tight).
There are many reasons why the iliotibial band can become tight. Tendons are flexible, elastic fibers that connect your muscles to your bones. When the muscle is squeezed, the tendon pulls on the bone and this causes the bone to move.
What are the types of iliotibial band syndrome?
You may have iliotibial band syndrome in one or both legs. If you have ITBS in both legs, it’s called bilateral iliotibial band syndrome.
How does Iliotibial Band Syndrome (ITBS) affect you?
If you are young and exercise constantly, you have a higher risk of developing iliotibial band syndrome. Examples of athletes who are more prone to ITBS include:
- Basketball players.
- Cyclists.
- hockey players
- Runners
- skiers
- Soccer players
- Even if you’re not an athlete, there are still some signs that give you a slightly better-than-average chance of developing iliotibial band syndrome.
The reasons are as follows:
- Bowed legs.
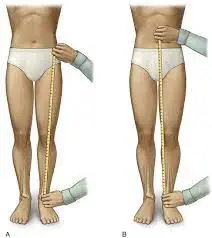
- One leg is longer than the other.
- Arthritis of the knee joint.
- Turning the ankle, foot, or foot inward during movement.
- Weakness in the hip, gluteal, or abdominal muscles.
How common is iliotibial band syndrome?
Experts note that iliotibial band syndrome often affects the training of US Marines. More than 20% develop iliotibial band syndrome. Frequent runners, especially long-distance runners, are also susceptible. Iliotibial band syndrome accounts for approximately 12% of running injuries. Women have more iliotibial band syndrome than men. Knee pain, one of the causes of which is iliotibial band syndrome, occurs in up to 25% of adults.
Purpose
The aim of this study was to evaluate the effect of progressive dissection of the ITB, gluteus medius, and minimus (med/min) muscles and hip joint capsule on the results of the Ober test in lightly embalmed cadavers and compare them with the assessment. of all structures. healthy In addition, both versions of the Ober test also assessed the change in thigh position between the gluteus med/min event and the hip capsule event.
It was hypothesized that transection of the ITB would significantly increase the range of motion of the thigh adduct, as measured by a clinometer when you perform the Ober test, and that the subsequent structural events (gluteal muscles and hip capsule) would cause additional growth in the thigh adduction.
Technique
Frank Ober described the TFL and ITB tightness test in an article entitled “Spinal Tension and Sciatica” in which he discussed the relationship of the TFL and ITB to low back pain (May 1935). This was later modified in 1937, warning against internal rotation and bending of the hip during the test.
Test position:
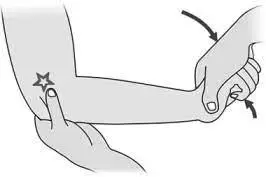
The patient should lie on his side, with the diseased side up. The lower knee and pelvis must be flexed to equalize the curvature of the lumbar region. To prevent movement in either direction, stand behind the patient and firmly stabilize the pelvis/greater trochanter. Grasp the distal end of the patient’s affected leg with the other hand and bend the leg at a right angle at the knee.
Test:
Extend and abduct the hip joint. Slowly lower your leg toward the table—bring your hip with you—until the range of motion is limited. Make sure that the hip does not rotate or flex internally during the test and that the pelvis is stable. Because allowing hip flexion and internal rotation would result in a tight TFL and not accurately measure length.
Result:
If the ITB is normal, the leg adducts and the thigh fall slightly below the horizontal plane, and the patient feels no pain. In this case, the test can be referred to as negative. If the ITB is tight, the leg will remain in an abducted position and the patient will develop lateral knee pain, in which case the test is called positive.
Modified Ober test
A variation of Ober’s test was first proposed by Kendalls in the journal Posture and Pain. This test places less stress on the medial side of the knee joint, less stress on the patella, less disturbance to a tight Rectus Femoris, and provides a full stretch of the TFL.
Test position:
The patient is on their side and the lower leg is bent at the hip and knee to flatten the lower back. The examiner stabilizes the pelvis and keeps the lateral body in contact with the table.
Note The lateral downward tilt is equivalent to hip abduction and would give way to a tight TFL.
Test:
The investigator extends his leg. Make sure the leg is not internally rotated.
Result:
With the knee straight and the hip in a neutral position, the thigh levels are about 10 degrees below the horizontal plane. This refers to normal height. The leg does not drop down, indicating strain in the ITB and TFL.
Evidence
A limited number of studies support the validity of this test. A study by Reese et al shows that using an inclinometer to measure hip adduction with both the Ober test and the modified Ober test appears to be a reliable method of measuring IT band flexibility and the technique is quite easy to use. This showed a significant difference in ROMs between testing with the knee flexed and the knee extended. Reliabilities were 0.90 and 0.91. The modified Ober test allows for a significantly greater range of motion in hip adduction than the Ober test, the two examination procedures should not be used interchangeably to measure IT band flexibility.
However, the results of Willet GM et al., “An Anatomical Study of the Ober Test” refute the hypothesis that the ITB plays a role in limiting hip adduction during both versions of the Ober test and question the validity of these tests. ITB. tension The findings highlight the influence of the gluteus medius and minimus muscles and the hip joint capsule on Ober test results.
The results of this study indicate that the Ober test evaluates the tension of the proximal structures of the hip joint, such as the gluteus medius and minimus muscles and the hip capsule, and not the ITB.
Notes
Contracted, inelastic quadriceps and shortened hamstrings increase posterior pressure on the patella. Shortening of the iliotibial region can lead to chronic pain on the lateral side and its relationship to the lateral patellar retinaculum, as well as functional disturbances in the femoral-patellar joint. Stretching the hypertrophied muscles often helps the patella move laterally when there is too much lateral pressure.
Key studies
A Clinical Biomechanics study by Gajdosik RL et al showed that hip adduction was more limited in knee flexion than in knee extension in both sexes (Pandlt; 0.009). This emphasizes the influence of knee position and gender on Ober’s test of iliotibial band length. An exercise developed by the Postural Rehabilitation Institute to recruit the hamstrings and abdominal muscles showed a significant increase in passive hip adduction angles (pandit; 0.01) and a reduction in pain (pandit; 0.01), immediately improving Ober test measurements in patients with low back pain.
The study showed that hamstring/abdominal muscle activation, rather than hamstring band stretching, may be an effective intervention for pelvic pain and a positive Ober test. The study shows ITB stretching and activation of the thigh and abdominal muscles in patients with pelvic pain as a result of the Ober test. Activation of the hamstrings and abdominals showed a reduction in pain and an increase in hip adduction ROM compared to ITB stretching alone.
Conclusion:
The study results refute the hypothesis that the ITB plays a role in limiting hip adduction during both versions of the Ober test and question the validity of these tests to determine ITB density. The findings highlight the influence of the gluteus medius and minimus muscles and the hip joint capsule on Ober test results.
Clinical Significance:
The results of this study indicate that the Ober test evaluates the tension of the proximal structures of the hip joint, such as the gluteus medius and minimus muscles and the hip capsule, and not the ITB.
FAQ
To Perform this test by placing the patient in a lateral position with the leg flexed at the hip and knee for stability. The examiner then passively abducts the upper leg and brings it slightly extended while the other hand supports the hip.
Modified Ober test: This is the same as the Ober test, but the affected area (upper limb) is extended from the knee instead of flexed to reduce the effect of the joint rectus femoris. Medial rotation is more of a concern than Ober’s test.
With the patient lying on his side, support the knee and bend it 90 degrees. Then abduct and extend your hips. Then release the knee support. Failure to adduct the knee is a positive test.
If in doubt, Ober’s test should be performed to determine the tightness of the iliotibial band. If Ober’s test is positive, a lateral floor wedge is prescribed and the patient begins a series of stretching exercises. These exercises have been shown to relieve and prevent ITBFS symptoms.
Perform this test by placing the patient in a lateral position with the leg flexed at the hip and knee for stability. The examiner then passively abducts the upper leg and brings it slightly extended while the other hand supports the hip.
Background: Recent studies have questioned the role of the iliotibial band (ITB) in lateral knee pain. The Ober test or modified Ober test is the most commonly recommended physical examination tool to assess ITB tightness.
Reference
Ober’s Test. (n.d.). Physiopedia. https://www.physio-pedia.com/Ober%27s_Test
Ober’s test. (2023, May 6). In Wikipedia. https://en.wikipedia.org/wiki/Ober%27s_test
Willett, G. M., Keim, S. A., Shostrom, V., & Lomneth, C. (2016, January 11). An Anatomic Investigation of the Ober Test. American Journal of Sports Medicine; SAGE Publishing. https://doi.org/10.1177/0363546515621762
L Gajdosik, R., M Sandler, M., & L Marr, H. (2002).The effect of knee position and gender on the Ober test for iliotibial band length. Clinical Biomechanics, 18(1), 77-79. https://doi.org/10.1016/S0268-0033(02)001687
Ober’s Test – Orthopedic Examination of the Hip – Physical Therapy Web. (2019, August 28). Physical Therapy Web. https://physicaltherapyweb.com/obers-test-orthopedic-examination-of-the-hip/
Willett, G. M., Keim, S. A., Shostrom, V. K., & Lomneth, C. S. (2016). An Anatomic Investigation of the Ober Test. American Journal of Sports Medicine, doi:10.1177/0363546515621762
O. (2022, May 26). Ober Test | OrthoFixar 2023. OrthoFixar. https://orthofixar.com/special-test/ober-test/
Ladva, V. (2023, August 6). Ober’s Test. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/obers-test/
Ober’s Test. (2022, September 5). Epomedicine. https://epomedicine.com/clinical-medicine/obers-test/
Ober’s Test – MSK Medicine. (n.d.). MSK Medicine. https://mskmedicine.com/clinical_skills/obers-test/