Wrist and Hand Examination
Table of Contents
Introduction
A Wrist and Hand examination were done in a systematic way that helps to diagnose for treatment of Wrist and Hand related conditions.
- A hand as well as a wrist form a group of complex, delicately balanced joints that are considered the most active portion of an upper extremity. Optimal overall function is essential to so many activities of daily living.
- The hand, as well as wrist examinations done in a structured manner, will assist to facilitate the most appropriate working diagnosis for the management.
- Diagnosing hand as well as wrist conditions is often difficult & for this reason, a bilateral comparison may be useful.
Subjective History
- Thorough history-taking is an essential first step in treating a patient. Every physiotherapist may develop their style and technique, however, a good interview may include the basic elements discussed below:
- Mechanism of an injury – How an injury occurred as well as what was the cause, for instance, a fall on the outstretched hand
- Insidious or sudden injury.
- Handedness, occupation, previous injury, and fracture history
- Location of the pain
- Presence as well as the location of the numbness, pins as well as needles, and/or tingling.
- Aggravating and relieving factors.
- Functional limitations.
- Were any diagnostic test/imaging done as well as what were the results?
Observation
- Observe an upper extremity as a patient enters the room
- Examine hand in function
Deformities
The attitude of the hand - Palmar Surface
- Creases
Thenar as well as Hypothenar Eminence
Arched Framework
Hills and Valleys - Dorsal surface
- Hills and Valleys
Height of metacarpal heads - Ganglions: Cystic structure which arises from the synovial sheath
Boutonniere Deformity
- Introduction
Extensor injuries of the hand are more common in young, except healthy males. Various injury mechanisms include hyperflexion, direct blunt trauma as well as penetrating trauma. - When left untreated, disruption of an extensor mechanism over zone III as well as detachment of a central slip leads to the Boutonniere deformity. The described deformity is characterized by flexion of a proximal interphalangeal joint (PIP) as well as hyperextension of a distal interphalangeal joint (DIP) because of a volar subluxation of lateral bands.
- Definition
A Boutonniere deformity is a deformity of the fingers in which the proximal interphalangeal joint (PIP) is flexed as well as a distal interphalangeal joint (DIP) is hyperextended. This is the extensor tendon injury over zone III. It is called a “buttonhole deformity.”
Swan Neck Deformity
- Description
- Swan-Neck Deformity (SND) is the deformity of a finger that is mainly characterized by the hyperextension of a proximal interphalangeal joint (PIP) as well as flexion of a distal interphalangeal joint (DIP).
- Reciprocal flexion of a metacarpal phalangeal joint (MCP) may be present. A Swan-Neck deformity is most commonly happened by an imbalance in the extensor mechanism of a digit.
- The deformity develops when this is a loss of an extension at the distal phalanx or tightening of the extensor mechanism at the proximal phalanx, both intrinsic as well as extrinsic, at the proximal interphalangeal joint.
Wrist as well as Hand Osteoarthritis
- Introduction
- Hand osteoarthritis (OA) is a common chronic condition involving one or even more joints of a thumb as well as fingers. This is associated with pain, decreased grip strength, loss of the range of movement(ROM), as well as joint stiffness leading to impaired hand function as well as difficulty with daily activities.
- Estimates of the prevalence of symptomatic hand osteoarthritis range from 13% to 26% and are greater in females.
- Evidence suggests the following:
- Long-term use of the night splint offers significant benefits to increasing pain, hand function, and strength, as well as a range of motion for patients with osteoarthritis.
- Programs of joint protection, advice, as well as home exercises are effective at improving grip strength as well as hand function.
- Low-level laser therapy is effective at improving the range of motion.
- No rehabilitation interventions were found to increase stiffness.
Dupuytren’s Contracture
- Introduction
- Dupuytren contracture is the benign, myeloproliferative progressive disease of a palmar fascia that results in the shortening, thickening, as well as fibrosis of a fascia & aponeurosis of a palm.
- Dupuytren disease is predominantly a myofibroblastic disease that affects a hand/fingers as well as results in contracture deformities.
- Commonly affected digits are those farthest from a thumb, for instance, a fourth (ring) as well as fifth (pinky) digits.
- The disease starts in a palm as painless nodules that form along longitudinal lines of the tension.
- The nodules form cords that produce contracture deformities within fascial bands as well as tissues of a hand.
- Dupuytren contracture is usually seen in Caucasians as well as a disorder often presents bilaterally. When unilateral, a right side is more likely to be involved compared to a left.
- In many people, there is a family history of men being more susceptible to a condition than women.
Hand Rheumatoid Arthritis
- Introduction
- Rheumatoid arthritis (RA) is a chronic inflammatory disease affecting hand joints as well as leading to impairment in hand functions.
- The most common clinical presentation of Rheumatoid Arthritis is polyarthritis of the small joints of the hands: the first proximal interphalangeal (PIP), and second metacarpophalangeal (MCP) joints as well as the wrist.
- A hand is one of the main elements of the rehabilitation of patients with rheumatoid arthritis (RA) because of deformities, which happen in approximately 90% of the patients.
- This is a serious issue, both in a psychological as well as functional aspect, attached to muscle strength reduction, the limited range of movement as well as non-acceptance of the changes in a shape of a limb.
- Adults with Rheumatoid Arthritis may have access to specialist physiotherapy, with, periodic review.
Functional Tests
- Aims: To obtain as well as quantify the asterisk to assess/reassess after an intervention is performed, for instance, turning a doorknob, holding the key, starting a pain-free grip or even key grip, opening the jar, turning on the tap, lifting the saucepan.
- Grip strength may be a good reliable tool to utilize (available cheaply on the internet).
Palpation
- Wrist (Dorsal to Volar)
- Radial Styloid
- Scaphoid
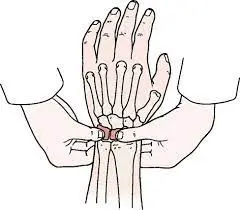
- Structure
- A scaphoid is situated below a radius at a radial (lateral) side of a wrist. This has a boat-like shape with many articulation surfaces. Over 80% of a bone is covered in cartilage. On a palmar surface of a bone, there is the tubercle that may be palpated at a base as well as the medial aspect of a thenar eminence when a hand is extended. This may also be palpated at a base of an anatomical snuffbox.
- 1st MC/Trapezium joints
- Lunate
- The lunate is one of the eight carpal bones of our wrist joint. This lunate bone is situated in the center of the proximal row of the carpal bones of the wrist joint.
- Lister’s Tubercle
- Ulnar Styloid
- TFCC
- Triangular Fibrocartilage Complex Injuries
- Introduction
A triangular fibrocartilage complex (TFCC) is a load-bearing structure that is situated between a lunate, triquetrum, as well ulnar head.
A function of our triangular fibrocartilage complex is to act as the stabilizer for an ulnar aspect of the wrist joint. - The triangular fibrocartilage complex is at a risk for either acute or chronic degenerative injury.
Forced ulnar deviation as well as positive ulnar variation carry associations with injuries to the - TFCC.
Patients with Triangular Fibrocartilage Complex Injuries may present with ulnar-sided wrist pain that can present with clicking or point tenderness between a pisiform as well as an ulnar head. - Triangular Fibrocartilage Complex Injuries are reported to accompany distal radius fractures in 39 to 84% of cases
- MRI imaging is wonderfully helpful as a preliminary diagnostic tool; arthroscopy is also one of the diagnostic gold standards.
- Management options include conservative therapies namely, rest, NSAIDs, as well as corticosteroid injections & operative treatment.
- The prognosis for Triangular Fibrocartilage Complex Injuries injury is generally favorable.
- Triquetrum
- Pisiform
A pisiform is one of the eight as well as the smallest carpal bones which forms part of a wrist joint.
This is the small pea-shaped bone. This develops in the tendon as well as in the sesamoid bone. The name of the pisiform bone is derived from the Latin word pisum which means “pea”. - This may be felt on an anteromedial side of a wrist.
- Hook of Hamate
- A hamate bone is one of eight carpal bones which forms part of a wrist joint. The word hamate for the bone of hamate arrives from the Latin word hamulus which means “a little hook”. This is the wedge-shaped bone with the hook, such as a process that may be found in a medial side of a wrist. Sometimes this is called unciform bone.
Palpation of Hand
- Bone
- Metacarpals:-5, Phalanges:-14, (Palpate for swelling, as well as tenderness)
- Palm of Hand
- A Thenar Eminence (3 muscles of the thumb, Atrophy seen in the carpal tunnel syndrome)
- Hypothenar Eminance (3 muscles of a little finger, Atrophy along with ulnar nerve compression)
- Palmar Aponeurosis (Dupuytren’s Contracture).
- Distal Radioulnar Joint Instability
- Assessment for the dorsal-volar instability
- Procedure Grasp the distal radius as well as ulna between the thumb & index of opposite hands 3-4 cm proximal the to wrist joint.
- Translate radius relative to the ulna in neutral, supination, as well as pronation.
- Positive test
- Crepitus
- Translation>5mm
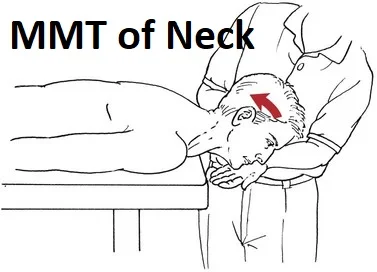
Neurological Assessment
- An upper Extremity Nerve Palpation:
- The aim is to reproduce symptoms if the peripheral nerve entrapment diagnosis is suspected.
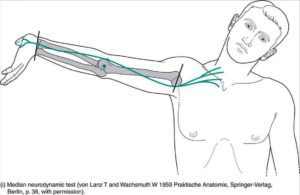
- To palpate the three major nerves of an upper extremity refer to the figure below.
- Median: Position of the patient supine, 90 degrees of shoulder abduction as well as elbow extension. Palpate medially to a bicep (mid humeral), and palpate distally at the wrist.
- Radial: An upper arm (0 degrees of the abduction, palpate proximal to a lateral epicondyle), distal radius, as well as snuffbox.
- Ulnar: An Upper arm (medial mid humeral area, shoulder 90 degrees of abduction, elbow 120 degrees of flexion) as well as a cubital tunnel.
Motion Testing
- If the patient is pain-free to the end range, a therapist can choose to apply overpressure.
- Wrist
Flexion/Extension
Radial/Ulnar deviation - 1st carpometacarpal
Extension, Abduction as well as Opposition. - Metacarpal-phalangeal (MCP)
Flexion, Extension as well as Abduction/Adduction. - Inter-phalangeal (IP)/Distal IP/Proximal IP
- Flexion as well as Extension.
Red Flags
- The section deals with screening a patient for possible serious pathologies which could cause wrist or even hand pain. These described conditions could warrant referral or even consultation.
- Infections
- Heat
- Swelling
- Pain
- Redness
- Inflammation
- Fracture/dislocation:
- Top 5 physical findings that are most useful in screening for wrist fracture. Localized tenderness, Pain on the active movement, Pain on the passive movement. Pain on the grip, Pain on the supination
- Anyone of the described above findings associated with the history of the trauma may be sent for radiographs
- Additional potentially tremendous serious conditions
- Scapholunate instability
- Arthritides
- Rheumatoid Arthritis
- Lyme disease
- Tuberculosis
- Peripheral Vascular Disease
- Peripheral Neuropathy
- History of the trauma, fall on an outstretched hand (FOOSH). Older age >65. The risk is the same for men/women
- Upper extremity nerve injuries that involve: Median; Radial; as well as Ulnar.
Special test
- A therapist can elect to do various special tests while a physical examination of the individual with wrist or even hand complaints. Mentioned below are potential tests that can be utilized categorized by possible diagnosis or tissue involvement.
- Scaphoid Fracture clinical examination (Tenderness of the Anatomical snuff box, tenderness of the Scaphoid tubercle, as well as Axial loading of the thumb)
- Definition/ DescriptionScaphoid bone (left hand):
- A scaphoid bone is the most frequently fractured carpal bone. In young children as well as the elderly population, scaphoid fractures are rare. The scaphoid bone is stronger as compared to the relatively weak distal radius in these age groups.
- The delay in diagnosis of scaphoid fractures may lead to a variety of adverse outcomes
- which include nonunion (no consolidation), delayed union, reduced grip strength, as well as a range of movement, along with osteoarthritis of a radiocarpal joint. Timely diagnosis, appropriate immobilization, as well as referral to the surgical opinion when indicated may reduce the likelihood of adverse outcomes.
- Scaphoid fractures are common, however, they present unique challenges due to the particular geometry of the fractures as well as a tenuous vascular pattern of a scaphoid. Delays in diagnosis as well as inadequate management for acute scaphoid fractures may lead to non-unions as well as subsequent degenerative wrist arthritis.
Neurodynamic tests
Introduction
- A neurodynamic assessment evaluates the length as well as mobility of various components of the nervous system.
- They are performed by the therapist placing progressively more tension on a component of a nervous system that is being tested & are divided into upper as well as lower limb tests.
- Upper Limb Tension Tests (ULTTs) are also famous as Brachial Plexus Tension or even Elvey Test.
- These described tests are most commonly designed to put stress on the neurological structures of an upper limb.
- These tests may be first described by Elvey as well thus also known as the Elvey test but most commonly called the Upper limb tension test.
- A shoulder, elbow, forearm, wrist as well as fingers are kept in specific positions to put stress on the particular nerve (nerve bias) as well as further modification in the position of each and every joint is done as the “sensitizer”.
- A ULTT’s equivalent to a straight leg raise designed for a lumbar spine.
Upper Limb Tension Test (one)1 (ULTT1, for checking Median nerve impingement)
- Indications:
- Radiating pain in the upper limb,
- Tingling sensations in first three fingers(thumb, index finger as well as middle finger).
- Action performed:
- Shoulder depression
- Shoulder abduction 110 degrees,
- Shoulder external rotation with the elbow is 90 degrees of flexion,
- Forearm supination
- Wrist as well as finger extension
- Elbow extension.
- Structural differentiation:
- Proximal symptoms, Relieve wrist as well as finger extension.
- Distal symptoms (provocation): Contralateral flexion of the neck.
Upper Limb Tension Test 2A (ULTT2A, For checking Median nerve impingement)
- Indications of the test:
- Radiating pain in the upper limb,
- Recent shoulder arthroplasty surgery,
- Recent Dislocation of a shoulder as well as Instability.
- Action done:
- Shoulder girdle depression
- Shoulder abduction 100 degrees
- External rotation with
- elbow at 90 degrees
- Forearm supination
- Wrist as well as finger extension,
- Elbow extension.
- Structural differentiation:
- Proximal symptoms: Relieve wrist as well as finger extension,
- Distal symptoms (provocation): Contralateral flexion of the neck.
Upper Limb Tension Test 2B (ULTT2B, Radial nerve compression checking)
- Indications:
- Radiating pain in the upper limb,
- Supinator tunnel syndrome,
- De Quervain`s disease,
- Cervical Radiculopathy
- Action performed:
- Shoulder girdle depression,
- Shoulder abduction 20-30 degrees,
- Shoulder internal rotation,
- Forearm pronation,
- Wrist, finger as well as thumb flexion,
- Elbow extension.
- Structural differentiation:
- Proximal symptoms: Relieve wrist as well as finger flexion.
- Distal symptoms (provocation): Contralateral flexion of the neck.
Upper Limb Tension Test 3 (ULTT3, checking Ulnar nerve compression)
- Indications:
- Pain radiating to the 4th as well as 5th digits,
- Thoracic outlet syndrome,
- Carpal tunnel syndrome.
- Action done:
- Shoulder girdle depression,
- Shoulder abduction 110 degrees,
- Shoulder external rotation,
- Forearm pronation,
- Wrist as well as Finger extension,
- Elbow flexion.
- Structural Differentiation:
- Proximal symptoms: Relieve wrist as well as finger extension.
- Distal symptoms (provocation): Contralateral flexion of the neck.
Tinel’s Test
- Purpose
- A Tinel test is mainly used to test compression neuropathy, commonly in diagnosing carpal tunnel syndrome.
- Technique
- This is done by lightly tapping (percussing) over a nerve to elicit the sensation of tingling or “pins as well as needles” in a distribution of a nerve.
- A Tinel sign is the tingling or even prickling sensation elicited by a percussion of an injured nerve trunk at or distal to a site of a lesion. A sign may also indicate nerve regeneration.
- When we say this test is Positive: A test is positive when the tingling or even prickling sensation is felt in a distribution of the nerve.
Scaphoid shift test
- Purpose
- A scaphoid shift test is a provocative maneuver mainly utilized to examine the dynamic stability of a scaphoid as well as reproduce the patient’s symptoms.
- This is also utilized to diagnose scapholunate interosseous ligament instability (SLIL). Watson first described this test at an American Research in General Orthopedics conference in New Orleans in March 1978.
- A test is commonly found helpful while an examination of a wrist & more specifically a scaphoid.
- Besides stability, an examiner may also be able to reflect a quality of an adjoining articular surface.
- Clinically Relevant Anatomy
- The ligaments that are thought to provide a principal help to a scaphoid are the radioscaphocapitate ligament, a scaphoid-trapezoid-trapezium ligament as well as a scapholunate interosseous ligament.
- A scapholunate interosseous ligament(SLIL) is a link between the carpal scaphoid as well as the lunate bone. This ensures the stability of a scapholunate joint as well as assists to keep the entire wrist stabilized.
- A scapholunate interosseous ligament is an intra-articular structure (for instance, synovial) composed of three regions:
- Dorsal ligament: Transversely oriented collagen fibers providing primary restraint for distraction as well as torsional/translational motions.
- Palmar ligament: Provides rotational stability.
- Proximal fibrocartilage: Negligible contribution to restraint of abnormal movement.
- Technique
- To Do a scaphoid shift test, a patient may rest his arm with his elbow on a table as well as his forearm lifted. An examiner sits across a table & places his arm next to a patient’s arm (like in the arm wrestling position right to right or left to left).
- A patient’s hand is mildly pronated as well as the examiner places his thumb on a palmar side of a scaphoid (on a scaphoid tubercule), his other fingers are wrapped around the back of the wrist at a distal part of a radius. It will allow an examiner to put pressure on a scaphoid along with his thumb.
- With his other hand, an examiner holds a patient’s hand at a metacarpal level.
- A hand is put into ulnar deviation movement as well as in slight dorsal flexion; in the position, a scaphoid lies almost ‘in line with an ulna.
- From this position, a hand is moved passively by an examiner into radial deviation movement as well as slight palmar flexion. Meanwhile, the constant pressure is given by a thumb on a scaphoid tubercle.
- While a radial deviation & slight palmar flexion, a distal part of the scaphoid tilts forward as well as thereby pushes against an examiner’s thumb (which is pushing in an opposite direction) causing stress on the joints.
- The stress is overcome in the normal wrist (minimal motion may be tolerated) but results in dorsal displacement (‘shift’) of a scaphoid in relation to the other carpal bones in the wrist of the patient with ligamentous laxity.
- When a thumb force is then abruptly taken away a shift will be decreased as well as a scaphoid will fall back in its neutral position, which can result in the painful ‘thunk’.
- This is essential to do this technique on both wrists as well as compare them.
- Interpretation
- Positive test: The palpable and/or audible reduction of a subluxated scaphoid as well as elicitation of symptomatic pain, usually on the dorsal side.
- Negative test: Scaphoid moves normally, pushing back on an examiner’s thumb with ulnar deviation of a wrist, as well as there is no symptomatic pain.

De Quervain’s Tenosynovitis
- Description
- De Quervain’s Tenosynovitis is a painful, inflammatory condition caused by tendons on a side of a wrist at a base of a thumb. Pain, which is the main complaint, gets worse with the abduction motion of a thumb, the grasping motion of a hand, as well as the ulnar deviation of the wrist joint. Thickening as well as swelling may also be present.
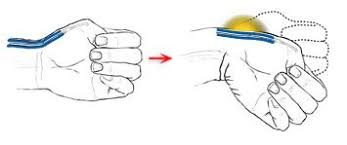
Finkelstein Test
- Introduction
- Finkelstein’s test is mainly a classic provocative test to diagnose De Quervain’s disease.
- Finkelstein hypothesized that an entry of a muscle belly of an extensor pollicis brevis (EPB) as well as abductor pollicis longus (APL) tendons into the first extensor compartment was responsible for the findings shown in his eponymous test.
- Clinically Relevant Anatomy Extensor pollicis brevis muscle (highlighted in green): Posterior view Extensor Pollicis Brevis (EPB)
- Radial abduction of the wrist joint(0-25°)
- Thumb extension of the wrist joint (90°)
- Abductor Pollicis Longus (APL)
Wrist radial abduction (0- 25°)
Thumb abduction (70°- 80°) - Purpose of Testing
A Finkelstein test is mainly utilized in a diagnosis of De Quervain’s syndrome. The fact implies the tenovaginitis as well as tenosynovitis of the M. extensor pollicis brevis & M. abductor pollicis longus. - Finkelstein maneuver is helpful for testing to diagnose De Quervain’s Tendonitis or even the first dorsal compartment tendonitis called after the Swiss surgeon Fritz de Quervain.
- It is the condition brought on by irritation or even inflammation of the wrist tendons at a base of a thumb. Inflammation causes a compartment (a tunnel or the sheath) around a tendon to swell as well as enlarge, making thumb & wrist motion painful.
- Testing Position
Sitting or even standing. - Technique
- To start with, a patient must sit comfortably as well as relax on an examination table. After that, examine the patient’s hand in the air, while the other hand rests just beside the body.
- A physical therapist then asks a patient to make a fist around the thumb & to do the ulnar deviation.
- The modified version of a test is that a patient must sit comfortably as well as relax on an examination table
- A patient may hold his afflicted hand in the air, during the other hand may be resting against his/ her body. A physiotherapist grasps an afflicted hand of a patient as well as rotates this in ulnar deviation. He pulls a patient’s thumb across the palm of his/ her hand. This causes additional stress on the extensor tendons of a thumb.
- A patient actively (or actively assistive) flexes the thumb maximally as well as wraps fingers over the thumb, making the fist. A patient then ulnar deviates his/her wrist to stretch the muscles of the 1st extensor compartment. A test is positive if a patient complains of pain over the 1st extensor compartment of a wrist.
- Interpretation
Negative result: A patient does not feel any pain radiating up the inside of his arm from the thumb. - Positive result: Ask a patient if he feels pain radiating up the inside of his arm from a thumb. If a patient reports noticeable pain after that, Finkelstein’s test is positive, which indicates De Quervain’s syndrome.
Lunotriquetral dissociation
- Definition
- Lunotriquetral dissociation (LTD) is the second most common ligamentous cause of carpal instability as well as is classified by Mayo‘s well-known Classification of Carpal instabilities as an instance of dissociative carpal instability (CID).
- An intrinsic meaning of dissociation is a division of the concrete substance. CID, used in the context, is a compound term to describe the injury to one of the major interosseous ligaments of a wrist, that is in the case of LTD the injury of the lunotriquetral ligament.
- Interpretation
- Negative result: A patient does not feel any pain radiating up the inside of his arm from the thumb.
- Positive result: Ask a patient if he feels pain radiating up the inside of his arm from a thumb. If a patient reports noticeable pain after that, the Finkelstein’s test is positive, which indicates De
- Clinically relevant autonomy
- A lunotriquetral (LT) ligament is the intrinsic ligament of a wrist, more particularly the interosseous carpal ligament that provides stability to a proximal carpal row.
- The ligament has a thin, horseshoe-shaped structure as well as may be divided into 3 parts: the dorsal, the proximal as well as the volar.
- A volar as well as dorsal portions attach directly to a bone, during a proximal portion attaches to a hyaline articular cartilage of the wrist as well as the hand joint.
- A volar portion is the most substantial one of 3 parts due to this ensuring functional stability within a lunotriquetral compartment.
Phalen’s Test
- Purpose
The purpose of this test for carpal tunnel syndrome (CTS) - Clinically Relevant Anatomy
- Median Nerve
Formed by spinal roots C6, C7, C8, as well as T1. - C6 innervates: Lateral side forearm: wrist extensors
- C7 innervates: Middle finger: wrist flexors
- C8 innervates the Medial side of the forearm, ring finger as well as little fingers. Flexors like
- T1 innervates: Medial side of the upper arm
- Innervates: Pronator teres, Palmaris longus, Flexor carpi radialis, Flexor digitorum superficialis, Flexor digitorum profundus (lateral half), Pronator quadratus, Flexor pollicis longus, Abductor pollicis brevis, Opponens pollicis, Flexor pollicis brevis, as well as Lumbricals
- A Phelan’s test is the provocative test that is mainly utilized in a diagnosis of CTS. It happens when a median nerve is compressed or even squeezed at a wrist. Pain is often worst at night. Daily activities namely driving as well as typing can increase the symptoms. The most common complaints are;
- Pain as well as tingling of hands & fingers.
- Numbness in the fingers (specifically the thumb, forefinger as well as the part of a middle finger)
- Pain in or near a wrist.
- Pain extending into an arm (less frequent)
- Skin lesions in a territory of a median nerve are possible owing to compression of the blood vessels in a carpal tunnel.
- Technique
- A patient places her flexed elbows on the table, allowing her wrists to fall into maximum flexion. A patient is mainly told to push the dorsal surface of the hands together as well as hold the position for 30-60 seconds. The position may increase pressure in a carpal tunnel, in effect compressing a median nerve between a transverse carpal ligament as well as an anterior border of a distal end of a radius.
- Another way to describe a standard Phalen’s test: A patient leaves her elbows bent between 0 ° -30 °. After that, a physiotherapist asks a patient to take supinate her forearm.
- After this, a physiotherapist carries a maximum palmar flexion of the wrist as well as holds this for 60 seconds.
- While this test a patient may be asked to explain each ten to fifteen seconds what she feels.
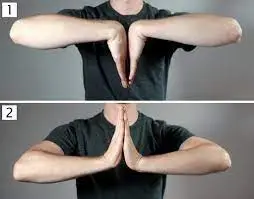
Reverse Phalen’s test
- A patient maintains the position of the full wrist as well as finger extension for ten to fifteen seconds.
- The pressure of the carpal tunnel increases after five seconds (compared to 20-30 seconds for a standard Phalen test). The longer this position is held, the greater the pressure on a wrist as well as carpal tunnel.
- Positive test: Both the Phalen test, as well as Reverse Phalen’s tests, are considered positive when a patient’s symptoms are reproduced, the test gives the same symptoms as that experienced with carpal tunnel syndrome, such as paresthesia (burning, tingling, as well as numbness) in a distribution of a median nerve.
- Negative test: The Patient feels no pain or other symptom, even if a movement is maintained for 3 to 4 minutes or longer.
- Alternative method
- The purpose of this test is to assess for carpal tunnel syndrome (CTS).
- Test Position: Sitting or you may take standing.
- Performing a Test: An clinician places a patient’s wrist in the maximal extension (but not under overpressure), during maintaining a shoulder in neutral as well as elbow in extension (avoids compressing nerve proximally) & finger extension. The position is maintained for thirty seconds or until numbness, as well as tingling, is felt in a median nerve distribution (palmar surface of 1st, 2nd, 3rd, as well as radial half of 4th digit).
- Positive test: An examiner may record the number of seconds at which symptoms are produced.
- Diagnostic Accuracy: This is not known.
- Performing a Test: According to Neumann, a carpal tunnel is formed by a palmar surface of the carpal bones (scaphoid, lunate, triquetrum, pisiform, trapezium, trapezoid, capitate, as well as hamate) & a transverse carpal ligament.
- The transverse carpal ligament attaches to our pisiform bone as well a hook of the hamate on the ulnar side & the tubercles of a trapezium as well as scaphoid on the radial side. These borders create a carpal tunnel through which the tendons of a flexor digitorum profundus, flexor digitorum superficialis, flexor pollicis longus as well as median nerve travel.
- It is not a wide space at all. When pressure is increased in the area, people typically feel numbness as well as tingling on the palmar side of the thumb, 2nd, 3rd, as well as radial half of the 4th digit.
- Note: Symptoms felt in a palm of a hand indicate pathology Proximal to a carpal tunnel.
- A position of the wrist, as well as finger extension, stretches a median nerve as well as therefore adds compression in a carpal tunnel, leading to numbness & tingling in a palmar surface of the 1st, 2nd, 3rd, as well as radial 1/2 of 4th digits.
Tinel sign
- Introduction
- Tinel’s sign is the tingling or “pins and needles” feeling you get when the healthcare provider taps the skin over the nerve. Tinel’s sign can be the indicator that a patient has nerve compression or damage where they are tapping.
- Testing for a Tinel’s sign is the method for the physical therapist provider to assess for signs of nerve damage or even nerve irritation at a specific site.
- A clinician may call a sign either Tinel’s sign or even Hoffmann, Tinel sign. The names come from individuals who first described it in 1915, physiologist Paul Hoffmann as well as neurologist Jules Tinel.
- Benefit
- A healthcare provider may test for Tinel’s sign if he is concerned about nerve damage or even irritation at a specific site.
Carpal Compression Test
- Carpal Compression Test (Apply pressure with the thumbs over the median nerve within the carpal tunnel, located just distal to the wrist crease.
- The test is positive if the patient responds with numbness as well as tingling within twenty seconds.
- If the patient does not respond with numbness & tingling within twenty seconds, then the test is negative.

Carpometacarpal Compression Test
- Assesses for 1st carpometacarpal joint pathology, most commonly arthritis.
- The aim of this test is to produce an axial compression of a thumb first.
Carpometacarpal joint with the “mortar and pestle” action.
Elicit pain from CMC/basal thumb osteoarthritis. - Procedure
- Grasp the patent’s 1st metacarpal with one hand as well as a distal radius with the other
Apply the longitudinal compression along the 1st metacarpal into the carpal bone, axially compressing the carpometacarpal joint
Apply the rotatory motion to the metacarpal
Positive Test
Pain at 1st carpometacarpal joint.
Froment’s Sign
- Purpose
- Froment’s sign is the physical examination of a hand to test for palsy of an ulnar nerve which results in decreased functionality as well as muscle weakness of a pinch grip.
- This tests the strength of the adductor policies of a thumb, which is innervated by an ulnar nerve & is weakened in the ulnar nerve palsy.
- Froment’s sign presents after damage to an ulnar nerve, which innervates the adductor pollicis as well as interossei muscles, which provide adduction of a thumb & extension of an interphalangeal joint.
- A flexor pollicis longus (innervated by a median nerve), may substitute for an adductor pollicis (innervated by an ulnar nerve) as well as cause a thumb to go into hyperflexion. Ulnar nerve palsy may be a result of the dysfunction at the cervical spine, elbow (cubital tunnel syndrome), or wrist (Guyon’s canal syndrome).
- Technique
- A patient is told to make a strong pinch between the thumb as well as the index finger and grip a flat object such as a piece of paper between the thumb as well as the index finger.
- An examiner next attempts to pull an object out of a subject’s hands.
- There is the weakness of adductor policies innervated by an ulnar nerve which may keep the interphalangial joint relatively straight; instead, the flexor pollicis longus muscle which is innervated by a median nerve is substituted for the adductor pollicis, and may cause the interphalangeal joint to go into the hyper flexed position.

Jeanne’s sign
- Similar to Froment’s sign, Jeanne’s sign is seen in response to the pinch forces. Instead of isolated thumb interphalangial joint flexion, the interphalangial flexion is accompanied by MP joint hyperextension.
- Some people have normal metacarpal phalangial joint volar plate laxity, allowing hyperextension of a wrist joint. Hence, if Jeanne’s sign is seen, one may determine whether this is related to the normally lax volar plate or to an absence of part or all (innervation is variable) of the flexors pollicis longus or both.
- The most essential observation is a comparison to a contralateral uninjured thumb. If both thumbs are fully innervated this is such (but not absolute) that a pinch pattern may be similar.
Sharpeys Test
- An examiner firmly grips a distal radioulnar joint and the proximal carpal row. After that, apply the compressive force of the carpus to the DRUJ. Next, add the rotation force in the pronation as well as supination. The positive test is pain or even clicking at the TFCC.
TFCC Stress Test
- It is sometimes called a TFCC Compression Test. A TFCC (Triangular Fibrocartilage Complex) stress test involves moving an affected wrist into ulnar deviation as well as applying the shearing or stress forces to recreate the pain.
Durkan’s Test
- Even though Phalen’s & Tinel’s are commonly taught, Durkan’s is likely a better test. Most of the time, the examination technique is called a carpal tunnel or even a medial nerve compression test.
- This involves applying direct pressure over a median nerve within a carpal tunnel long enough to blanch a skin. It typically takes about twenty to thirty seconds. The positive test is the reproduction of the symptoms.
Lunotriquetral Instability
Reagan’s Test
- Sometimes this test is called a lunotriquetral ballottement test. This examiner pronates an affected hand as well as stabilizes a lunate.
- This then pushes up on a triquetrum & down on a lunate. The examiner may observe for tenderness or pain as well as compare to a contralateral.
Thumb carpometacarpal joint Grind Test
- The positive test includes pain, subluxation, or even crepitus.
- The thumb carpometacarpal Grind Test is when the examiner grips a metacarpal bone of a thumb and applies an axial load.
- Optional: Move in gentle circles. The positive test is pain or even crepitus.
Pronator Teres Syndrome
- To do this test, the patient is standing, elbow flexed to 90°. An examiner supports an elbow with one hand as well as uses the other to embrace a patient in the handshake position.
- An examiner attempts to supinate a patient during a patient resists, trying to pronate a forearm.
- During resisting supination, an examiner after that passively extends an elbow. The positive test is the reproduction of symptoms (pain, paresthesias) in the median nerve distribution.
Belly Press Test
- Purpose
- The purpose of belly-press test is mainly utilized to isolate a subscapularis muscle, to test a subscapularis muscle for tear or even dysfunction.
- This is mainly used as the alternative to a lift-off test when a lift-off test cannot be performed due to pain or limited internal rotation range of motion of a shoulder.
- Technique
- A patient sits or stands with an elbow flexed to 90 degrees, with a palm of a hand on an upper abdomen, just below a xiphoid process.
- A patient is asked to the press palm of a hand against an abdomen, through shoulder internal rotation.
- This test is positive for subscapularis muscle dysfunction if a patient compensates for the motion through embarked wrist flexion, shoulder adduction as well as shoulder extension. The unconscious compensatory motion may result in an elbow dropping behind a trunk.
Supination Lift Test
- Purpose
- The purpose of this test is to assist in determining whether pathology is presented in a triangular fibrocartilage complex.
- The ‘‘Supination Lift Test’’ may be described for the localized tear to the peripheral, dorsal Triangular fibrocartilage complex. With the below-described test, the pain is embarked when a patient tries to lift an examination table with the palm.
- At the underside of a table, the forces a load across the TFCC with a wrist supinated as well as extended, causing dorsal impingement, & is helpful in a diagnosis of peripheral, dorsal TFCC tear.
- Technique
- A patient places his palms on the undersurface of the table as well as attempts to lift. The onset of pain upon stabilizing body weight indicates the positive supination Lift test.
- It will also result in pain or even clicking if the TFCC is involved.

Piano Key Sign
- Purpose
- The purpose of this Piano-Key Sign Test is a test carried out for a clinical assessment of wrist instability.
- This is utilized as the indicator for distal radio-ulnar joint instability as well as tears of a triangular fibrocartilage complex of the wrist.
- Technique
- In a Piano-key Sign Test, a wrist is supported in the pronation as well as a hand is stabilized in a normal position. The force is applied to a head of an ulna.
- Positive Result
- This below-described test is positive if an ulnar head returns to its anatomic position after the removal of the force given to an ulnar head.
- A bear’s resemblance to when a piano key springs up after the force from a finger is removed from the key, therefore, the name “piano-key” sign.
- The instability, & pain, are judged relative to a contralateral wrist.
- Negative Result
- No instability or motion was observed on the removal of the pressure on an ulnar head.
Bunnell-Littler Test
- Purpose
- The purpose of this test is to evaluate a source of proximal interphalangial joint flexion movement limitation by differentiating between intrinsic muscle or even capsular tightness in an affected digit.
- The typical patient presentation can include pain located in a distal intermetacarpal space as well as prolonged gripping or making the fist. Symptoms are most often seen in the ring as well as the long finger.
- Technique
- The metacarpal phalangial joint is held in the extended position as well as the physical therapist passively flexes the proximal interphalangial joint making note of an available range.
- This test is then repeated with the metacarpal phalangial joint flexed. If no change in the movement is detected between the two tests, and after that capsular restriction at the proximal interphalangial joint is implicated.
- If a movement increases when the metacarpal phalangial joint is flexed and after that lumbrical muscle tightness is implicated.
Wartenberg’s Sign
- Definition
- Wartenberg’s Sign refers to a slightly greater abduction of a fifth digit, owing to weakness or paralysis of the adducting palmar interosseous muscle as well as unopposed action of the radial innervated extensor muscles (digiti minimi, as well as digitorum communis ).
- This can not be confused with Wartenberg’s Syndrome which is given as the entrapment of the superficial branch of our radial nerve with solely sensory manifestations & no motor deficits.
- Background
- The first literature regarding the described sign appears to be the Letter to the Editor By Robert Wartenberg himself in 1939. In this, the researcher emphasizes the diagnostic importance of the sign in ulnar nerve neuropathy which is not documented.
- Sometimes the fourth finger also has the tendency to assume the position of abduction, however, usually, this is only a little that is found in an abnormal position.
- This was found to be most conspicuous when a patient was asked to extend their finger at the proximal joints.
- An essential sign has become increasingly evident from numerous experiences which indicate that the tendency of the little finger to be abducted can constitute an early (in some cases the first) as well as a late sign of ulnar palsy”.
- Adduction of a little finger is done by an interosseous as well as abduction by hypothenar muscles.
- Both groups of muscles are innervated by our ulnar nerve. However, in the abduction of the little finger, an extensor digiti minimi as well as the branch to the little finger of the extensor digitorum communis play a definite part. These both are innervated by the radial nerve. If the hand, as well as wrist muscles innervated by our ulnar nerve, are weak, those innervated by the intact radial nerve predominate in strength & abduct a little finger.
- Therefore, it is understandable why the abduction of the little finger is best seen when extensor digitorum communis comes into action & extends the fingers as well as the hand.
- In cases with the combined palsy of our ulnar nerve and radial nerve, this sign would not be present” explains the author.
- Purpose
- Wartenburg’s sign is the test that is mainly utilized to assess the integrity of motor innervations of the hand intrinsics in cases of suspected ulnar neuropathy.
- This inability to do adducted digital extension is owing to weakness in the ulnar innervated intrinsic muscles, as well as an unopposed motion of the slightly medially attached extensor digiti minimi results in extension & abduction of the fifth digit.
- A positive test indicates our ulnar nerve neuropathy however does not determine a site of compression (Guyon’s canal, cubital tunnel, as well as an arcade of Struthers).
- How to perform this test
- This is seen that the author his name is Robert Wartenberg had not prescribed the specific technique for assessment of this sign.
- The literature describes a few techniques for assessment based on an explanation given by the author.
- A study by the famous Goldman et al (2009) adopted a technique for the assessment of Wartenberg’s Sign. A patient is placed with the wrist in the normal position as well as the forearm fully pronated & instructed to do a full extension of all the fingers.
- Once digits are extended patient is told to fully abduct all fingers & then adduct all fingers. The positive sign is indicated with an observation of abduction of a 5th digit, with an inability to adduct the 5th finger when extended.
- David J Magee proposes another technique with minor variation, a patient sits with her hand resting on a table. An examiner passively spreads a finger apart as well as asks a patient to bring them together again.
- Inability to the squeeze a little finger to a remainder of a hand indicates a positive test for ulnar neuropathy.
- At the end the patient always follow the instructions which is given by the physical therapist very carefully.

The Allen Test for Blood Flow
- Purpose of this test
The purpose of this Allen test for blood flow was first described in 1929 by Edgar V. Allen as a non-invasive evaluation of arterial patency of a hand in patients with thromboangitis obliterans. - This test has since been adapted as a Modified Allen test (MAT). In the famous Allen’s original test, both our hands were tested simultaneously by the examiner compressing one artery of each hand at the same time. The MAT efficiently evaluates the adequacy of collateral circulation but needs the testing of one hand at a time.
- An Allen test is the first-line standard test that is utilized to assess an arterial blood supply of the hand. The test is done whenever intravascular access to a radial artery is planned or for selecting patients for radial artery harvesting, namely for coronary artery bypass grafting or for forearm flap elevation.
- An Allen test is part of a diagnostic work-up for vascular abnormalities of an upper limb namely, in thoracic outlet syndrome (TOS). In thoracic outlet syndrome as well as specifically vascular TOS, one possible cause may be a compression of a subclavian artery or vein as this passes through an inter scalene triangle by a muscle body of a scalene where there may be muscular hypertrophy.
- Clinically Relevant Anatomy
A hand has a complex as well as rich vascular network, that is mostly supplied by radial as well as ulnar arteries. - A radial artery runs between the brachioradialis as well as flexor carpi radialis muscles of a forearm as well as at the wrist and splits into the superficial branch to contribute to a superficial palmar arch.
- Another branch crosses dorsally deep to the tendons of an anatomic snuffbox to form the deep palmar arch.
- An ulnar artery lies under the flexor carpi ulnaris of a forearm as well as at a wrist and enters a Guyon’s canal, where this splits into the deep palmar branch as well as the superficial palmar branch.
- A superficial palmar branch forms a superficial palmar arch, during a deep branch contributes to the deep palmar arch.
- Since radial, as well as ulnar arteries both form anastomosis (the deep & superficial palmar arch) a blood supply of a hand, is ensured even if one of the arteries is occluded.
- How to done this Allen test
- An Allen Test for blood flow
A radial artery is located by the palpation at a proximal skin crease of a wrist & after that compressed with three digits. - An ulnar artery is similarly located & then compressed with three digits. With both arteries compressed, a subject is told to clench as well as unclench the hand ten times. A hand is then held open, ensuring that the wrist, as well as fingers, are not hyperextended and splayed out as well. A palm is observed to be blanched. Our ulnar artery is released & the time taken for the palm as well as especially a thumb & thenar eminence to become flush is noted.
- If a capillary refill time is less than ten to twenty seconds the test is considered positive. This test is next completed with a radial artery tested in a similar fashion.
- Both hands may be tested for comparison. When doing the Allen test, hyperextension of a hand as well as wide separation of the fingers may lead to a false-negative result.
- It is owing to occlusion of a trans palmar arch, as well as parts of the fingers & palm that may continue to remain blanched after the release of an ulnar artery.
- To prevent this from happening this test may be done with a hand partially open as described in Allen’s original work.
Wringing test
- Purpose of the test
- The purpose of this Wringing Test is the general screening examination utilized to detect carpal tunnel syndrome, Lateral epicondylitis, or even arthropathy.
- This is a basic test that may assist narrow down the focus of the regional examination.
- How to perform this wringing test
- The Patient may be awake as well as cooperative when doing the wringing test.
The Patient may be seated or even standing while a test.
The patient wrings the towel or even washcloth. With hands on both ends of a towel, a patient twists this in the opposite directions. - An examiner checks for any numbness, tingling or even shooting pain on a wrist or over an elbow area.
- Interpretation
Positive Wringing Test - Paresthesia or the presence of numbness, tingling sensation or even shooting electrical pain. It could indicate carpal tunnel syndrome.
- Elbow Pain may indicate epicondylitis or even sprain or strain along an elbow area.
Wrist Pain may indicate arthropathy, sprain, or strain along a wrist area.
FAQ
The wrist is made up of 8 small bones (carpal bones) plus two long bones in the forearm: The radius as well as the ulna. Each finger consists of one hand bone (metacarpal) & three finger bones (phalanges), during each thumb consists of one metacarpal bone & two phalanges.
The hand is made up of the wrist, palm, as well as fingers. The wrist is made up of many smaller bones as well as joints that allow the hand to move in several directions. This also includes a distal end of the forearm bones. The palm is made up of 5 bones that connect to the 14 phalanges, as well as finger bones.
The components of a wrist examination include a thorough history, visual inspection, objective assessments, as well as systematic physical examination, including palpation, as well as provocative testing to identify tenderness & abnormal movement between bones.
Typical findings in the hands include symmetrical joint inflammation typically affecting proximal interphalangeal joints, metacarpophalangeal joints as well as wrist joints. Other features of RA in the hands mainly include muscle wasting, ulnar deviation, swan neck deformity, Boutonnière’s deformity, and Z-thumb deformity as well.
Watson’s test is mainly utilized by physicians to diagnose scapholunate instability. The test has a low specificity & sometimes is positive for Capito-lunate instability. As many as twenty to twenty-five percent of normal wrists may also have the crunch.