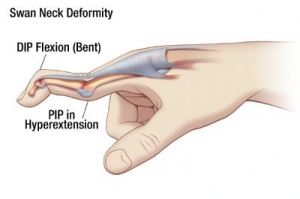
Swan Neck Deformity
Table of Contents
Definition
- Swan-Neck Deformity (SND) is a deformity of the finger distiguished by hyperextension of the proximal interphalangeal joint(PIP) and flexion of the distal interphalangeal joint (DIP).
- Reciprocal flexion of the metacarpal phalangeal joint (MCP) may also be present.
- A Swan-Neck Deformity is the cause of an imbalance in the extensor mechanism of the digit.
- The deformity evolves when there is a loss of extension at the distal phalanx or tightening of the extensor mechanism at the proximal phalanx, both intrinsic and extrinsic, at the PIP joint.
What are the Causes of Swan Neck Deformity?
- Swan-Neck Deformity is primarily engendered by destruction to the fitment of the extensor tendon.
- Injury to the extensor tendon may be the cause of a traumatic laceration, a closed avulsion from a direct blow to the DIP while the digit is extended, or debilitated at the DIP from chronic inflammation as well as extensor tendon subluxation due to an inflammatory disease most frequently rheumatoid arthritis.
- Demolition of the extensor mechanism results in laxity at the volar plate and tightness at the triangular ligament near the proximal interphalangeal (PIP).
- The resulting shape looks like a swan’s neck, which is how the condition got its name.
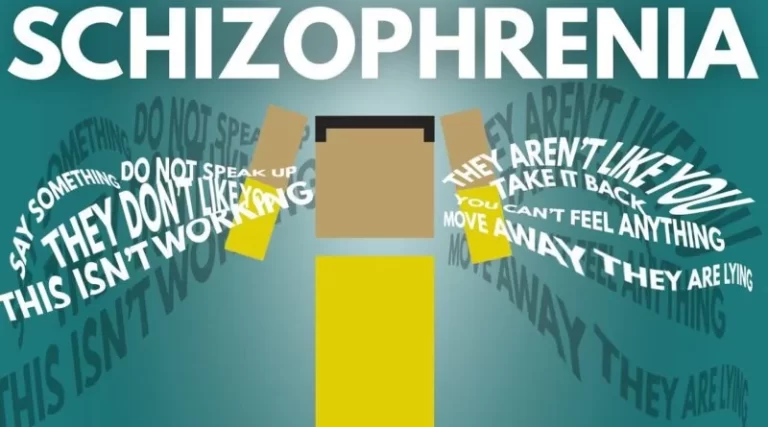
- Swan-Neck Deformity may be caused by different types of conditions like rheumatoid arthritis, non-treated mallet finger, and other disorders like cerebral palsy, stroke, Parkinson’s disease, traumatic brain injury, psoriatic arthritis, scleroderma, and hand trauma.
Symptoms of Swan Neck Deformity
- A person with Swan-Neck Deformity can present with a history of inflammatory diseases like rheumatoid arthritis or trauma to the extensor mechanism of the finger.
- On examination, the person can come up with inflammation of the joints, stiffness in the fingers, and a slow difficulty in flexion at the PIP.
- A snapping sensation can also happen during flexion.
Staging
- The Nalebuff classification system is most frequently used to classify the severity of a Swan-Neck Deformity.
- This classification of the system is based on the PIP joint stiffness with connected MCP joint positions.
Type 1: PIP joint is flexible in every position of the MCP joint.
Type 2: PIP joint flexion is restricted in some positions of the MCP joint.
Type 3: PIP joint flexion is restricted irrespective of the position of the MCP joint.
Type 4: PIP joints are stiff and have a faulty radiographic appearance.
Evaluation
- Active and passive Range of Motion should be checked at the MCP, PIP, and DIP independently.
- In the prime stages, it is possible for the PIP joint to maintain flexibility, although will return to deformity when the full digital extension is take place.
- In the expired stages, the PIP will present with improved stiffness and possibly be fixed into hyperextension.
- Along with manual testing, a person should be screened for rheumatoid arthritis and x-rays should be managed to diagnose articular disruption, severe arthritis in the later stages, or even carpal collapse.
- In order to determine whether a person is coming up with a capsular restriction or intrinsic tightness, a Bunnell-Littler Test (Finochietto-Bunnell test) is taken place.
- The Bunnell-Littler test is done by holding the MCP in an extended position while passively flexing the PIP, noting the present ROM.
- The motion is then repeated again with the MCP flexed.
- If there is no substitute in motion between the two tests, then capsular restriction at the PIP joint is suggested.
- If the motion improves when the MCP is flexed, then intrinsic muscle tightness is suggested.
How is SND diagnosed?
- The person should see the doctor if they notice a substitute in the bending of the finger joints.
- It is possible that the doctor can be permitted to identify the condition just by checking the hands during a physical exam.
- The doctor can validate the diagnosis after an X-ray.
- This procedure also permits the doctor to look out the bones and joints in the fingers for abnormalities or injuries.
What treatment options are available for Swan Neck Deformity?
- The treatment for SND may be different, based on the condition’s severity.
- Noninvasive treatments involve physical therapy (PT), occupational therapy (OT), and splints.
- More invasive procedures involve surgery.
- These may range from minor soft tissue repair to more drastic measures like replacing or fusing the finger joint.
- The doctor will aim to correct SND and regain the function of the fingers using the best method for the specific case.
Treatments for swan neck deformity include:
- Physiotherapy exercises: Massages and stretches are used to improve the strength and mobility of the fingers and hands.
Splints:

- Extension block splints help to accurately the hyperextension at the PIP joint.
- A progressive extension splint can help increase flexion deformity.
- A ring splint, also known as a figure eight splint, is situated around the PIP joint to accurately deformity in the primary stages for a few weeks.
- The superiority of a ring splint is that the finger may be bent down free.
Stretching Exercises:
- Hand treatment for passive stretching may be merged with splinting.
- This combination of treatments can improve flexibility and mobility at both the DIP and the PIP joints.
- Slowly straighten the involved finger and hold for five secs at the apex of this finger extension.
- Do1 a set of 10 repetitions three to five times per day to create flexibility in the finger joints.
Strengthening Exercises:

- Strengthening exercises help to maintain the range of motion, strengthen weak muscles, and increase function in the fingers and hands.
- It can be done by using a ball.
Range of motion Exercises:
- Digits’ passive range of motion is suggested to maintain flexibility and range of motion in the fingertips.
Finger Flexion:
- Put the involved hand’s elbow on a flat surface, like a table, and lift the forearm straight up.
- Gently bend the fingers to the middle of the palm, one at a time.
- Hold for five secs at the apex of each finger flexion.
- To improve flexion and range of motion in the fingers, do 1 set of 10 repetitions three times a day.
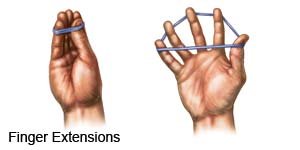
Finger Extension:
- Stand in front of the table, and put the involved hand on the table’s surface with the palm flat and the fingers extended.
- Lift up each finger as far off the table as possible, one at a time, hold for five secs at the apex of the finger extension, and then relax.
- Do 1 set of 10 repetitions three times per day.
- Pick up tiny objects like coins and marbles with the affected finger and thumb gives the joint health and flexibility in addition to finger extension, squeezing a rubber ball, and holding each squeeze for five secs will help the involved hand’s range of motion and flexibility.
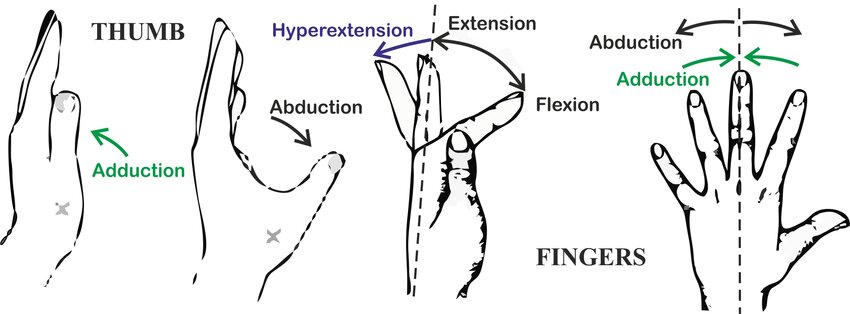
Finger Adduction and Abduction:
- Stand tall and bend the elbow to a 90° angle.
- Spread the fingers as apart as possible by taking the arm of the injured finger to the side of the body.
- Hold for five seconds before reuniting the fingers.
- Perform 1 set of 10 repetitions three times a day to improve the circulation of oxygenated blood to the fingers and increase joint health.
Medical rings:
- These include a special ring that is worn on the finger joint to help accurately its position and escape it from bending.
- In most cases, the finger with swan neck deformity may be treated nonsurgically with specially designed splints that immobilize the finger while giving natural healing.
Surgery:
- Surgery is the only option in more severe cases, and it is used to reposition the tissues in the finger joint, or the joint is replaced or fused to regain movement.
- Any one of the given surgeries can be performed:
Splinting
- The doctor can advise a splint to try to accurately and stabilize the SND.
- This can be done in tandem with PT or OT. Splints can involve the entire finger or the joint specifically, like with a ring splint.
- This is a figure-eight splint that the patient wears around the PIP joint all the time for several weeks.
- The patient can still bend their joint downward with this type of splint.
- Some other splints can be worn around the clock, or possibly only during some parts of the day.
- Splints can restrict all movement of the finger or permit some use of it.
Soft tissue repair
- Soft tissue repair is a type of surgery that mainly focuses on the skin, tendons, and ligaments (soft tissues) near the middle joint of the digits.
- It is a type of surgery the doctor can suggest for moderate-level SND, as the surgery can not help more serious cases.
- One type of soft tissue repair is the superficial sling.
- This targets the volar plate to help it better restrain the middle joint of the finger from hyperextension while permitting downward movement in the joint.
PIP joint arthroplasty
- Correcting SND can need the replacement of a joint in the finger.
- PIP joint arthroplasty is when the doctor replaces the middle joint in the finger.
- The doctor may suggest this type of surgery if the middle joint is stiff.
- The doctor will also balance the soft tissues around the new joint to regain movement in the finger.
- The patient will find after a joint arthroplasty that it is much easier to move the fingers, and the patient may feel less pain. Keep in mind that joint replacements can wear down over time.
Finger joint fusion
- Finger joint fusion is when the doctor fuses the joint in the finger so it may no longer move.
- It is most frequently done in the DIP joint. The doctor will suggest this if this joint is not working exactly.
- After the surgery, the person will not able to move the joint and it will stay straight.
- The doctor may suggest a joint fusion in the PIP joint instead.
- This procedure outcomes in the doctor fusing the joint in a bent position.
- This surgery should decrease the pain in the injured finger joint.
Recovery after surgery
- Recovery from surgery on the finger will take too many weeks, if not months.
- The doctor will give the postoperative plan for the daily care of the surgically repaired finger.
- They will likely suggest that the patient should wear a splint while the finger heals.
- The patient will need to see the doctor a few weeks after the surgery and possibly another time or two thereafter.
- It is also likely that the patient will attend weekly PT or OT sessions to decrease swelling and pain and improve strength and mobility in the digit.
FAQ
Hand therapy, Extension block splints can accurately the excessive movement of the middle joint. Progressive extension splinting can help with the flexibility of the distal interphalangeal joint (DIP), the joint closest to the fingertip.
If left without treatment, the swan’s neck deformity may indeed be permanent.
Those with Ehlers-Danlos Syndrome (EDS), a genetic condition that affects the connective tissue, experience Swan Neck
Deformity in their digits due to the hyper-flexibility generally in the disease.
Swan neck deformity is a normal complication of rheumatoid arthritis. This may affect hand function to a greater degree than other rheumatoid arthritis-related deformities.
It is left untreated, and the DIP joint droops and won’t straighten out. This condition is identified as a mallet finger. The extensor tendon can become imbalanced and start to pull the PIP joint into hyperextension, forming a swan neck deformity. Chronic inflammation from RA may also disrupt the very end of the extensor tendon.


One Comment