Cervical Radiculopathy
Table of Contents
What Is Cervical Radiculopathy?
Cervical radiculopathy is often termed a pinched nerve. It is the most ordinary condition of the neck.
Cervical radiculopathy is the damage or a change in the way nerve functions resulting from one of the nerve roots near the cervical vertebrae is compressed.
Cervical radiculopathy is a neck condition that results in neurological dysfunction. It is caused by compression and inflammation of any nerve roots of the cervical spine (neck). Neurological dysfunction can include radiating pain in the arm, muscle weakness, altered reflexes, and/or numbness.
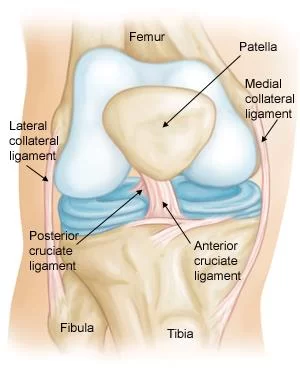
Cervical radiculopathy occurs with pathologies that cause symptoms to the nerve roots. Those can be compression, irritation, traction, and an injury to the nerve root. It is caused by a herniated disc, narrowing in the foramen, or degenerative spondylitic change (that includes osteoarthritic change or degeneration) leading to stenosis or narrowing of the intervertebral foramen.
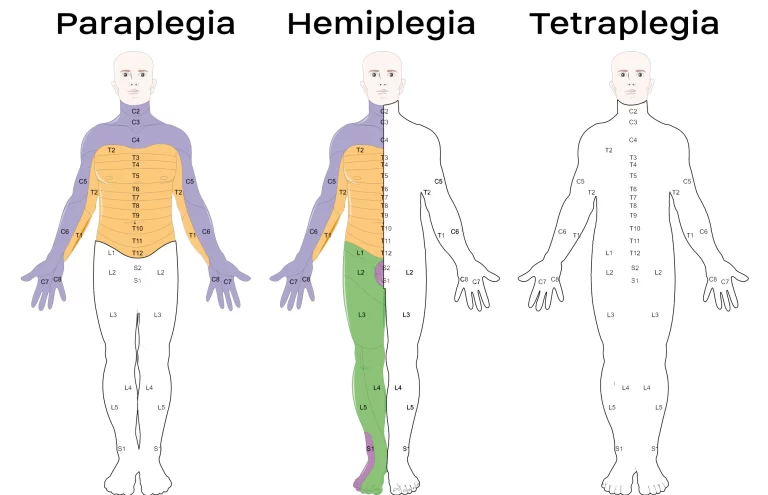
Most of the time cervical radiculopathy appears unilaterally(on one side of the neck), however, it is possible for bilateral( both sides of the neck) symptoms to be present if large bony spurs are present at one level that may impinge/irritating the nerve root on both sides. If there is peripheral radiation of pain, weakness, or pins and needle sensations are present, the location of the pain will follow back to the concerned affected nerve root.
Anatomy of Cervical Spine:
The spine is made up of 24 bones, called vertebrae, that are placed on top of one another. These bones connect to each other creating a canal that protects the spinal cord.
There are seven cervical vertebrae that begin at the base of the skull and form the neck comprising the cervical spine.
Other parts of your spine include:
Spinal cord and nerve: These spinal nerves travel through the spinal canal carrying messages between your brain and muscles. Nerve roots divide into branches out from the spinal cord through openings in the vertebrae (foramen).
Intervertebral discs: Present in between the vertebrae are flexible intervertebral disks. Disc act as shock absorbers when a person walks or runs. The disks are flat and round and about a half-inch thick.
Intervertebral discs consist of two components:
- Annulus fibrosus: Annulus fibrosus is the hard, flexible outer ring of the disk.
- Nucleus pulposus: The nucleus pulposus is the soft, jelly-like center of the disk.
Spinal Cord: Spinal cord works like a highway that connects the nerves located all over your body to the brain so that the brain can send signals and communicate with the rest of the body.
Nerve Roots: A nerve root is the initial part of a nerve that exits the spinal cord. The nerve root is the root of the nerves that extend out to other parts of your body.
When a nerve root becomes pinched or compressed, it can affect the nerves that are attached to it. This is why a pinched nerve in a neck called cervical radiculopathy can cause pain that radiates down to the arm and may be in the forearm.
These seven small vertebrae form the cervical spine, or neck, and start at the base of your skull. Cervical radiculopathy occurs in this area.
The nerves that run through the cervical spine send messages back and forth between the muscles and the brain. The roots of these nerves branch come out through openings in your vertebrae called foramen. Damage to these nerve roots can cause pain and the loss of sensation along the nerve’s pathway into the arm and hand, depending on where the damaged roots are discovered.
What are the Causes of Cervical Radiculopathy?
Cervical radiculopathy is defined as a dysfunction of a nerve root in the cervical spine. It is a broad disorder with several mechanisms of pathology and it can affect people of any age from a young age to old age, with peak prominence between the ages of 40-50.
Any condition of the spine that causes compression or irritation of a spinal nerve root can result in radicular symptoms. In younger patients, typically between 30 and 40 years of age, disc trauma and herniation are the most frequent causes of impingement. With increasing age, the causation becomes mainly degenerative. At 50 and 60 years of age, disc degeneration becomes the most common cause. At 70 years of age, causation tends to stem from foraminal narrowing as a result of arthritic change.
Damage in the spine can occur as a result of pressure from material from a ruptured disc, degenerative changes in vertebrae, arthritis, or other injuries that placed pressure on the nerve roots.
The most common cause of cervical radiculopathy include:
- Degenerative Changes
- Herniated disc
- Cervical spondylosis
Degenerative changes:
As the disks in the spine in older age, they lose height and begin to bulge or come out. They may also lose the water content of the disc. It begins to dry out and become stiffer. This problem causes the settling, or fusion of the disk spaces and loss of disk space height.
As the disks lose their height, the space between the vertebrae decreases, and the vertebrae move closer together. The body responds to the collapsed disk by forming an extra bone called a bone spur, which forms around the disk to strengthen it. These bone spurs donate to the stiffening of the spine. A bone spur may also narrow the foramen, which is the small openings on each side of the spinal column where the nerve roots exit and pinch the nerve root.
Degenerative changes in the discs are often called arthritis or spondylosis. These changes in discs are normal and are in every person and they occur in everyone. In actuality, nearly half of all middle-aged people and older have worn disks and compressed nerves that may not cause painful symptoms.
In middle-aged people, normal degenerative changes in the discs can induce pressure on nerve roots. Cervical foraminal stenosis, for example, happens when these changes occur, it narrows the openings in your vertebrae, which causes them to pinch nerve roots.
Injury: In younger people, cervical radiculopathy occurs to be the result of a ruptured disc, maybe as a result of trauma. Discs often herniate or come out with activity, such as when you do movements such as bend, lift, twist, or pull. When the disc herniates from its place, its material then compresses or inflames the nerve root, causing pain.
Cervical spondylosis:
Cervical spondylosis refers to slow wear and tear or age-related changes in the cervical spine. Such changes in the cervical spine may include:
Narrowing of the disc space
Bulging of the contour of the disc
Calcification of the disc and vertebral margins that result in bone spurs
These changes in the discs can be diagnosed or identified using conventional X-rays and other radiographic imaging examinations, including magnetic resonance imaging (MRI) or computed tomography (CT scan).
Disc herniation:
A disk herniates when its jelly-like material called a nucleus pushes against its outer ring called an annulus. If the disk is very worn or injured, the nucleus may compress all the way through. When the disc protrudes out toward the spinal canal, it places pressure on the sensitive nerve root, causing pain and weakness in the area where the nerve supplies.
Disc herniation and cervical spondylosis conditions are both called “degenerative” processes. It is age-related changes of the spine that occur with aging, wear, and tear. They become more dominant with age, and they are known to occur in people who experience no neck pain at all.
Since a herniated disc is a more delicate (pimple-like) projection than spondylosis, It is more likely to become smaller or settle completely on its own over time. Spondylosis, on the other hand, generally directs to harder and more dense tissue changes.
Sometimes it is called a bone “spur” in the aging spine.
A herniated disk occurs with lifting, pulling, bending, or twisting movements in the body.
Factors can contribute to a cervical herniated disk, including:
- Aging.
- Repetitive motions in the neck.
- Lack of regular or daily exercise.
- Bad posture.
- The incorrect way to lift or twisting, causing additional stress on your neck.
- Injury to the neck.
Less often, cervical radiculopathy is caused by:
- Infections in the spine
- Tumors in the spine caused by cancer
- Benign, or noncancerous, growths in the spine
- Sarcoidosis, the growth of inflammatory cells
Risk factors of Cervical Radiculopathy
Some factors can increase your risk for cervical radiculopathy. Your risk may be increased if you:
- Age: Between 40 to 50 years person have the risk of this
- Smoking cigarettes
- Had a history of radiculopathy
- Strenuous activity or repeated movement
- Lift heavy objects
- Oftentimes dive into a pool from a diving board
- Drive equipment that continuously vibrates
- Playing golf
Level of compression:
Level Of Compression
The most common level of root compression in cervical radiculopathy is:
- Compression in C7 (46.3–69%),
- Followed by C6 (19%–17.6%)
- Compression of roots C8 (10%– 6.2%)
- Compression of roots C5 (2%–6.6%).
One possible cause is that intervertebral foramina are the largest in the upper cervical region and progressively decrease in size in the middle and lower cervical areas, with an exception of the C7-T1 foramen (C8).
Symptoms of Cervical Radiculopathy:
The nerves that connect to the cervical spine (neck) extend out to the following body parts:
- Shoulders.
- Arms.
- Chest.
- Upper back.
Because of this, the neurological symptoms that result from cervical radiculopathy can radiate down from the neck to any one or a combination of these body parts, depending on which nerve root is affected. Cervical radiculopathy generally affects only one side of the body.
The main symptom of cervical radiculopathy are as follows:
Pain: Pain spreads into the arm, neck, chest, upper back, and shoulders. Often, this affects just one side of the body.
The pain of cervical radiculopathy starts at the neck and radiates down the arm in the area served by the damaged nerve. The pain is usually described as burning or sharp. Certain neck movements like extending or straining the neck or turning the head may increase the pain.
Sensory problems:
- Numbness in the fingers or hands.
- Tingling or a “pins and needles” like feeling in fingers and hands.
Motor problems:
- Muscle weakness.
- Weakened or loss of reflexes in arms and legs.
How to Diagnose Cervical Radiculopathy?
To diagnose cervical radiculopathy. the doctor will ask you about symptoms and medical history,
The doctor will do some physical examination to diagnose.
Physical examination includes a check of your neck, shoulders, arms, and hands for muscle weakness and problems with sensation or reflexes. The doctor may ask you to move your arms or neck to see if doing certain movements, a person may cause or ease pain or other symptoms.
Spurling Test:
The Spurling test compresses the foramina when doing the movement. It is useful in diagnosing likely radiculopathy. With the head extended, the head should be rotated. The test is positive if the pain radiates down to the upper limb of the ipsilateral side of the rotation.
They may perform other imaging tests:
- X-rays: X-rays for evaluating the narrowing of vertebral openings or disk injury or disc space narrowing. Also, evaluate neck and upper extremity pain
- CT scans: CT scan shows inside a structure to get more detailed pictures of your cervical spine
- Magnetic resonance imaging(MRI): MRI to check for damage to nerve roots or soft tissue abnormalities including herniated discs and compressed nerves.
- Electromyography(EMG): to see how your muscles work when they are at rest and contracted. EMG measures muscle response or electrical activity in response to nerve stimulation of the muscle.
Treatment of Cervical Radiculopathy:
Fortunately, over 85% of cervical radiculopathy cases resolve (get better) without any precise treatments within 8 to 12 weeks.
If your symptoms continue, cervical radiculopathy has several other treatment options. As the condition affects every person differently, the treatment plan will be unique according to the person’s situation.
Treatment options include:
- Immobilization.
- Medication.
- Cervical epidural steroid injection.
- Physical therapy.
- Surgery
Doctors almost always start with nonsurgical treatments to treat cervical radiculopathy. More than half percent of people with cervical radiculopathy have good to excellent results with nonsurgical therapy.
If nonsurgical treatment is not working, your doctor may recommend surgery.
Non-surgical Treatment:
Immobilization for cervical radiculopathy:
The doctor may immobilize the neck for short-term management and to relieve symptoms, The doctor may recommend wearing a soft cervical collar (neck brace) to decrease neck movement and reduce nerve root irritation. A soft cervical collar is a padded collar in a ring shape that wraps around the neck and is held in place with Velcro.
A doctor typically does not recommend wearing a cervical collar for more than 1-2 weeks because, for a long time, it can lead to muscle atrophy (muscle loss) in the neck.
Rest:
In the acute phase, it may be important to refrain from repetitive movements of the neck, as well as forceful or heavy-lifting movements. A soft cervical collar is often helpful for limiting neck motion and providing splinting for a position of comfort when at rest. With rest, a person can treat conservatively. Applying an ice pack or hot pack may reduce inflammation and reduce pain in the neck.
Medical treatment:
Medication for cervical radiculopathy
In some cases, particular medications can help reduce (relieve) symptoms of cervical radiculopathy, including:
Medicines include corticosteroids (anti-inflammatory drugs) or nonsteroidal pain medication like ibuprofen or naproxen. Steroids may be prescribed either orally by mouth or injected epidurally into the space surrounding the dura, which is the membrane that surrounds the spinal cord.
Anti-inflammatory drugs: NSAIDs (non-steroidal anti-inflammatory drugs), such as aspirin, ibuprofen, and naproxen, can provide both pain ease and anti-inflammatory effects for cervical radiculopathy. They provide relief by decreasing the inflammation at the affected nerve root(s).
Oral corticosteroids: A short course of corticosteroids taken orally by mouth may help relieve pain by reducing swelling and inflammation around the pinched nerve.
Cervical epidural steroid injections for cervical radiculopathy:
A cervical epidural steroid injection (cervical ESI) is an injection of anti-inflammatory drugs. A steroid or corticosteroid is injected into the epidural space around the spinal nerves in the neck to treat. The main goal of cervical epidural steroid injections for cervical radiculopathy is to help control pain caused by irritation and inflammation of the spinal nerve roots in the neck.
Although steroid doesn’t relieve the pressure on the nerve caused by a narrow foramen or by a bulging or herniated disk, they may reduce the swelling and relieve the pain long enough to allow the affected nerve to recover faster.
Some patients may get relief partially or some may not get relief at all.
Cervical ESIs have potentially severe side effects and complications. Be sure to ask your doctor about the benefits and risks of getting a cervical ESI.
Surgical Treatment:
Surgical treatment for cervical radiculopathy.
A doctor may recommend surgery if the person experiencing severe and persistent pain despite trying nonsurgical therapy for at least 6 to 12 weeks or if a person experiencing severe neurological issues due to cervical radiculopathy.
Several different surgical procedures can treat cervical radiculopathy. The procedure that the doctor recommends will depend on many factors, including what symptoms a person has, overall health, and the location of the affected nerve root.
There are three surgical methods commonly performed to treat cervical radiculopathy. They are:
- Anterior Cervical Diskectomy and Fusion (ACDF)
- Artificial Disk Replacement (ADR)
- Posterior Cervical Laminoforaminotomy
The procedure that which doctor recommends will depend on a number of factors—most importantly, the type and location of the problem. Other factors include:
- Patient preference for a procedure
- A doctor’s preference and experience
- An overall health and medical history (including whether you have had prior neck surgery)
Anterior Cervical Diskectomy and Fusion (ACDF)
ACDF is the most commonly performed operation to treat cervical radiculopathy. The procedure involves removing the damaged disc or bone spurs and then stabilizing the spine by fusing the spine
The goals of ACDF are to:
Restore alignment of the spine
Maintain the joint space available for the nerve roots to leave the spine
Limit motion across the degenerated segment of the cervical spine
Artificial Disk Replacement (ADR)
ADR procedure involves removing the degenerated disc and replacing the disc with artificial parts, as is done in hip or knee replacement. The aim of disc replacement is to allow the spinal segment to maintain some flexibility and maintain more normal motion.
Similar to ACDF, a doctor will use an “anterior” approach for the surgery—making a 1 to 2-inch incision along the neck crease. The exact location and length of the incision may vary depending on the specific condition.
Posterior Cervical Laminoforaminotomy
The “Posterior” part refers to the back part of the body. In this procedure, the doctor will make a 1 to 2-inch incision along the midline of the back of the neck. The exact location and size of the scar may vary depending on the person’s condition.
The doctor removes the bone, bone spurs, and tissues that are compressing the nerve root that causes radiculopathy. If compression is due to a herniated disk, a doctor will remove the portion of the disc that is compressing the nerve, as well.
Physical Therapy Treatment:
Physical therapy and specific exercises focused on strength training and stretching your neck muscles can help in treating cervical radiculopathy. Physical therapy regimen will be unique to patients and depends on several factors, such as which area of your neck is affected and overall physical health and abilities.
In general, a physical therapy regimen for cervical radiculopathy will progress through different stages as pain improves. Treatment begins with gentle range-of-motion exercises, The physical therapist can add intermittent traction to help relieve pain. and as pain decreases, therapists start adding strengthening and conditioning activities once the acute (severe and sudden) symptoms decrease.
A physical therapist may also include learning ways to have good posture and perform the job safely and comfortably.
When pain is decreased, range of motion(ROM) and strengthening exercises can help to slowly restore areas in the neck and shoulder that have been weakened by disuse and pain.
Treatment Options:
- Education and advice
- Manual Therapy
- Exercise Therapy – AROM, stretching and strengthening
- Postural re-education
Education and Advice
Education is the important key to getting the patient on the side and working co-operatively with physiotherapy. If patient understands the condition and the reason for the neck and arm pain then they are more likely to be compliant with any rehabilitation plan.
In cases of a prolapsed disc, tobacco smoking causes constriction of the vascular network surrounding the intervertebral disc (IVD), reducing the indirect exchange of nutrients and anabolic agents from the blood vessels to the disc.
Manual Therapy
There are some contradictions in using manual therapy techniques and their efficacy is questioned. Mobilization and manipulation when combined with exercise were beneficial for pain relief and improvement of function for continuous mechanical neck disorders with or without headache, but as a stand-alone treatment manipulation and/or mobilization were not beneficial. At best manipulations, it may also only provide short-term pain relief
Furthermore, cervical spine manipulation brings a risk of complications like vertebral dissection and spinal cord compression because of huge disc herniation. Therefore, this intervention should be prevented cervical radiculopathy, especially if imaging of the spine has not yet been conducted. Being aware of any potential risk factors such as arterial insufficiency, Hypertension, Craniovertebral ligament insufficiency, and upper motor neuron disorders is also essential

The efficacy of cervical traction in addition to manual exercise in patients with cervical radiculopathy. Adding mechanical traction to exercise for patients with cervical radiculopathy resulted in decreased disability and pain, particularly at long-term follow-ups.
Manual therapy consisting of thrust mobilizations of the cervical or thoracic spine and cervical non-thrust mobilizations (PA glides/Lateral Glides in ULTT1 position/Rotations/Retractions) was shown to be effective at reducing pain levels, improving function, and increasing joint ROM. When manual therapy was combined with exercise therapy it was more effective than single manual therapy or exercise therapy however both control groups were effective at reducing signs and symptoms.
Muscle Energy Techniques (MET)
Neurodynamics – Gliding and Sliding/Tensioning
The neurodynamics sliding and tensioning techniques, whilst having the patient in an upper limb tension position. It is conducted in a slow and oscillatory manner. With improvement in symptoms, the technique progressed to a ‘tension’ technique, Again, positive outcomes were observed in regard to pain and function, although treatment duration was not recorded.
Exercise Therapy
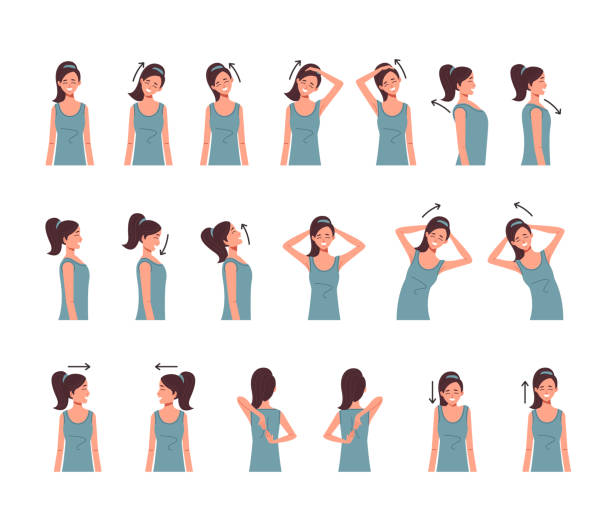
Exercise therapy has the most positive and enduring effects on the condition. Exercises such as contralateral rotation and side flexion are amongst the simplest forms of exercises which are effective against signs and symptoms in the neck, given in the form of active ROM. Due to the complex and close relationship of muscles with the intervertebral foramen. In the likely presence of reduced ROM, stretching is also an efficacious form of treatment to regain ROM
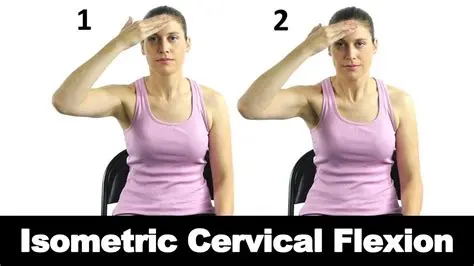
Once ROM increases strengthening exercises can be conducted to develop stability and decrease the risk of developing nerve root irritation in the future, as long as it is not caused by a structure that cannot be affected by physical therapy. During the initial stages of treatment, strengthening should be confined to isometric exercises in the affected upper limb. Once the radicular symptoms have been settled, progressive isotonic strengthening can start. Initially, it involves low weight and high repetitions (15-20 repetitions). Closed kinetic chain activities can be very useful in rehabilitating weak shoulder girdle muscles.
Patients should be instructed to stay as active as possible and perform exercises daily on the days between the therapy sessions. Written exercise instructions should therefore be given to the patient.
Scapula strengthening and cervical strengthening can be included.
Cervical strengthening exercises should include supine craniocervical flexion to stimulate contraction of the deep neck flexor muscles without contraction of superficial neck muscles. Feedback using an air-filled pressure sensor or tactile signals can be useful. The patient should perform three sets of 10 contractions for 10-12 seconds with proper muscle activation. Craniocervical flexion contractions were also performed with the patient seated, with the goal of 30 repetitions of 10-12 second contractions.
Scapular strengthening exercise: Retraction of the scapula against resistance with elastic, theraband.Retraction of the scapula against resistance using elastic bands or pulleys can be added. Scapular strengthening exercises included prone horizontal abduction, side-lying forward flexion, a prone extension of each shoulder, as well as prone push-ups with an emphasis on shoulder protraction. The goal was 3 sets of 10 repetitions at a time, with resistance added as the person tolerated.
Stretching exercise:
- Side stretch
- Chin tuck
- Diagonal stretch
- Chest and shoulder stretch
Strengthening exercise:
- Isometric
- Prone head lift
- Supine head lift
- Scapular retraction
- Shrug
Prevention:
Prevention:
While you can not always prevent cervical radiculopathy, there are certain things a person can do to reduce risk, including:
Maintaining a healthy weight or carrying weight is not more.
Staying physically fit by doing exercises.
Practicing good posture regularly and doing work in a comfortable position.
Doing stretching exercises to keep your muscles strong and flexible to avoid tightness
Summary:
Cervical radiculopathy is defined as a disorder by compression, traction, irritation, or herniated disc that affects a spinal nerve root in the cervical spine. Cervical radiculopathy generally produces neck and radiating arm pain, numbness, sensory deficits, or motor dysfunction in the neck and upper extremities. It is important to have knowledge of cervical anatomy because it is the essential key to effective physiotherapy practice and treatment.
Because there are other pathologies that have the same signs and symptoms of radiculopathy, it’s recommended to do a good examination physically or radiologically. Doctors can use imaging studies (MRI) or electro-physiologic studies(EMG + Nerve Conduction Studies). There are 4 clinical tests that help to diagnose radiculopathy: Spurlings Test, Upper limb tension-1, Distraction test, and Cervical Flexion Rotation Test. When all 4 of these clinical tests are positive, the post-test probability of cervical radiculopathy is 90%.
The main aim of physical therapy or medical management of cervical radiculopathy is decreasing pain and disability.
FAQs:
What is the most common cause of cervical radiculopathy?
Cervical foraminal stenosis is a considerably common cause of cervical radiculopathy. A cervical herniated disc is the other common cause. If the inner material of the cervical disc leaks or comes out and inflames or impinges the surrounding nerve, it can cause cervical radiculopathy.
How serious is cervical radiculopathy?
In some rare cases, cervical radiculopathy may continue to progress with numbness and weakness getting more threatening despite treatments. The longer that numbness and/or weakness lasts in the shoulder, arm, or hand, the more likely that these deficiencies will become permanent or lead to paralysis.
What should you not do with cervical radiculopathy?
In cervical radiculopathy, a person skips high-impact activities, such as running, if you have neck pain. A person may do exercises to maintain neck strength, flexibility, and range of motion(ROM).
What makes cervical radiculopathy worse?
Axial compression of the spine and rotation to the ipsilateral or same side of symptoms reproduces or worsens cervical radiculopathy.
Does cervical radiculopathy ever go away?
Fortunately, over 85% of cervical radiculopathy cases settle (get better) without any specific treatments within 8 to 12 weeks. If your symptoms persist, cervical radiculopathy has several other treatment options




14 Comments