A Pinched nerve in the neck
Table of Contents
Introduction
- A Pinched nerve in the neck (also known as “Cervical Radiculopathy”) is a condition that outcomes in radiating pain, weakness, and/or numbness started by constriction of any of the nerve roots in your neck. Most cases of cervical radiculopathy go away with nonsurgical management.
What is the Pinches nerve?
- A Pinched nerve in the neck (also known as “Cervical Radiculopathy”) is a condition that outcomes in neurological dysfunction caused by compression and inflammation of any of the nerve roots of your cervical spine (neck). Neurological dysfunction can involve radiating pain, muscle weakness, and/or numbness.
- “Cervical” arrives through the Latin term “cervix,” which means “neck.” In the case of cervical radiculopathy (pinched nerve in the neck), the problem is in your neck, not your cervix. (The cervix, the small passage forming the lower end of the uterus, is called so because it is a neck-like passage.)
What is the cervical spine?
- Your spine (backbone) is the long, flexible column of bones that preserves your spinal cord. It starts at the base of your skull and ends in your tailbone at your pelvis. Your cervical spine is the neck part of your spine. It involves seven bones (C1-C7 vertebrae).
- Vertebrae assist protect your spinal cord from injury. Between the vertebrae in your spine are round cushions known as disks. They have soft, gel-such centers and a firmer outer layer, such as a jelly doughnut. These disks produce cushioning for your vertebrae and flexibility for you.
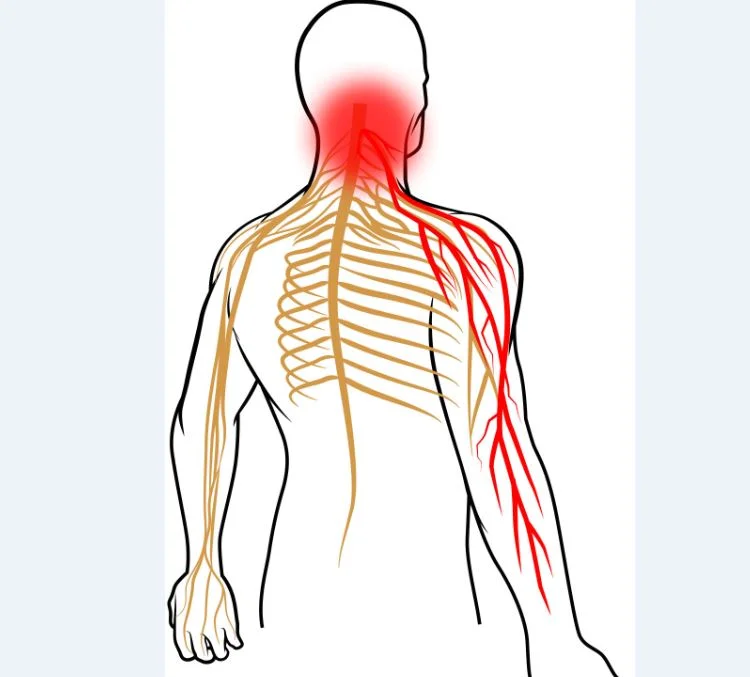
- Your spinal cord acts as a highway that connects the nerves located all over your body to your brain so that your brain can send signals & communicate with the rest of your body. A nerve root is the early segment of a nerve that leaves your spinal cord. It is the root of the nerves that extend out to other parts of your body. Different nerve roots along your spine extend to different areas of your body.
- When a nerve root becomes pinched, it can harm the nerves that are attached to it. This is why a pinched nerve (cervical radiculopathy) in your neck can create pain that radiates down your arm.
Whom does a Pinched nerve in the neck affect?
- Anyone can get cervical radiculopathy, but it is more usual in adults.
- A Pinched nerve in the neck caused by a herniated disk is more usual in people up to 50 years old. And cervical radiculopathy caused by disk degeneration is more usual in people in their 50s and 60s.
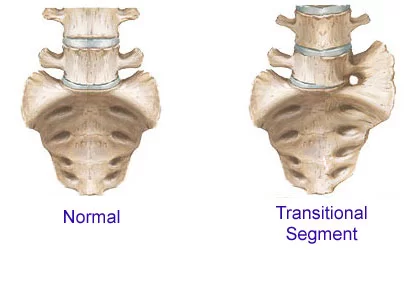
- People in their 70s or older are conducive to acquiring cervical radiculopathy from foraminal narrowing as an outcome of arthritis. The foramen is the bony hollow opening middle vertebrae through which spinal nerve roots travel.
How common is a Pinched nerve in the neck?
- A Pinched nerve in the neck is somewhat usual. Cervical radiculopathy harms approximately 85 out of 100,000 people. In over half (1/2) of cervical radiculopathy (pinched nerve in neck) cases, the C7 nerve root is damaged. Approximately a quarter of cases harm the C6 nerve root.
What are the signs and symptoms of a Pinched nerve in the neck (cervical radiculopathy)?
The nerves that connect to your cervical spine (neck) extend out to the following body areas:
- Shoulders
- Arms
- Chest
- Upper back.
- Because of this, the neurological symptoms that outcome from cervical radiculopathy can radiate down from your neck to any one or a combination of these body parts, depending on which nerve root is harmed. Cervical radiculopathy typically only harms one side of your body — for example, your right arm, not both arms.
Neurological symptoms from cervical radiculopathy that can radiate down from your neck involve:
- Pain
- Numbness
- Tingling or a “pins and needles” feeling,
- Muscle weakness
- Weakened reflexes.
- A Pinched nerve in the neck harms people differently. You may have any combination of the over neurological symptoms or only one.
What does a Pinched nerve in neck pain feel like?
- People with cervical radiculopathy commonly describe the pain as sharp or burning. Moving your neck in certain ways, such as extending or straining it, may increase the pain.
- Some people with cervical radiculopathy notice that their pain reduces when they locate their hands on over all their heads. This may transient relieve pressure on the harmed nerve root.
What causes the Pinched nerve in the neck?
- A Pinched nerve in the neck occurs when a nerve root in your neck (cervical spine) creates compressed (pinched) and inflamed.
This compression has 2 main causes:
- Degenerative changes that occur in your spine as you age (cervical spondylosis),
- A herniated (bulging) disk in your neck.
Cervical spondylosis and pinched nerve in the neck
- The greatest cases of cervical radiculopathy are due to cervical spondylosis.
- Cervical spondylosis is a common word for age-related wear and tear and gash and incision and gash (degenerative exchanges) in your cervical chine (neck) that can lead to neck pain, neck stiffness, and other symptoms. Sometimes, this condition is known as arthritis or osteoarthritis of the neck.
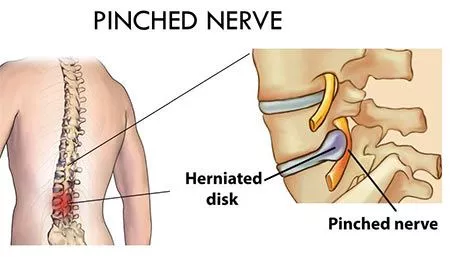
- As you age, the disks in your spine and the middle of your vertebrae lose height and begin to bulge. They also become less jelly- such as and become stiffer. This problem causes the collapse of the disk spaces and a decrease in disk space height.
- As the disks decrease in height, your vertebrae move closer together. Your body answers to the collapsed disk by forming more bone — known as bone spurs (osteophytes) — around the disk to strengthen it. These bone spurs can narrow the foramen — the little openings on each side of your spinal column where the nerve roots exit — and pinch the nerve root. This is known as foraminal stenosis. The pinched nerve root starts with cervical radiculopathy.
Herniated disks and pinched nerve in the neck
- Between aging or harm, the outside layer of a vertebra disk can weaken and crack. A herniated disk occurs when the inner “jelly” substance of the disk pushes through the crack.
- A herniated disk starts cervical radiculopathy when the connected material from a disk in your neck presses on nearby spinal whim-whams.
Several factors can contribute to a cervical herniated disk, involving:
- Aging
- Repetitive neck motions
- Lack of regular exercise
- Poor posture
- Wrong lifting and twisting, cause additional stress on your neck
- Injury to your neck.
- A Pinched nerve in the neck caused by a herniated disk is more usual in people up to 50 years old.
Diagnosis
- You will want to appointment with your healthcare provider regarding your pinched whim-whams if it is not answering to conservative treatment at home.
Your healthcare provider (doctor) will ask about your:
- Medical history
- General Health
- History of injuries or accidents
- Symptoms.
- They will then inspect your neck, shoulder, arms, and hands. They will see for muscle weakness, check for exchanges in reflexes and ask about the various sensations you are feeling. From this time cervical radiculopathy almost every time harms one side of your body (is unilateral), your healthcare provider (doctor) will equal the sensations you feel on one side of your body to your other side.
- Your healthcare provider (doctor) may tell you to perform certain neck and arm movements in an effort to recreate and/or relieve your symptoms.
- A Pinched nerve in the neck can be hard to diagnose, as numerous other neurological conditions, like neuropathy, can cause pain and numbness. Because of this, you may require to undergo certain imaging tests so your healthcare provider (doctor) can confirm a cervical radiculopathy diagnosis.
Tests to diagnose a Pinched nerve
Aside from a physical exam, healthcare providers (doctors) utilize the following tests to diagnose cervical radiculopathy or to rule out other possible causes of your symptoms:
- Spine X-rays: X-rays of your cervical spine are the most usual imaging tests for evaluating neck and upper part pain. Different views or angles can reveal various issues, such as disk space narrowing and foraminal narrowing (stenosis).
- Magnetic resonance imaging (MRI): Magnetic resonance imaging (MRI) utilizes a big magnet, radio swells, and a computer to produce detailed images of the inner of your body. An MRI scan is the imaging method of option for evaluating radiculopathy. MRI allows your healthcare provider (doctor) to see soft tissue abnormalities, including herniated disks and compressed nerves.
- Computed tomography (CT) scan: A CT scan looks at structures inside of your body by using X-rays and computers to produce images. Healthcare providers (doctors) typically utilize the Computed tomography (CT) scan for the identification of traumatic damage that outcome in cervical radiculopathy symptoms.
- Electromyography (EMG): An electromyography (EMG) test calculates muscle feedback or electrical activity in feedback to a nerve’s stimulation of the muscle. This test can assist determine if a nerve is working normally.
How is the Pinched nerve in the neck treated?
- Excellently, over 85% of cervical radiculopathy cases resolve (get better) without any particular management within eight to 12 weeks.
- If your symptoms persist, cervical radiculopathy has so many treatment options. As the condition harms everyone differently, your treatment plan will be unique to your situation.
Treatment options involve:
- Immobilization
- Medication
- Physical therapy
- Cervical epidural steroid injection
- Surgery.
- Healthcare providers (doctors) nearly always start with nonsurgical therapies to manage cervical radiculopathy. Concern with 90% (ninety%) of people with cervical radiculopathy have good to excellent issues and join nonsurgical remedies.
- If nonsurgical treatment is not working, your healthcare provider may recommend surgery.
Immobilization (drug) for a pinched nerve (whim-wham) in the neck
- For short-term management and to lessen symptoms, your healthcare provider (doctor) may suggest carrying a soft cervical collar (neck brace) to minimize neck movement and decrease nerve root irritation. A soft cervical collar is a padded ring (collar) that wraps around your neck & is grasped in place with Velcro.
- Healthcare providers (doctors) typically do not recommend wearing a cervical collar for more than one to two weeks because it can conduct in muscle atrophy (muscle loss) in your neck.
Medical Treatment
In some cases, certain specifics can help palliate (relieve) symptoms of cervical radiculopathy, including:
- Nonsteroidal anti-inflammatory medicines (NSAIDs): NSAIDs, similar to aspirin, ibuprofen, and naproxen, can give both pain relief and anti-inflammatory goods for cervical radiculopathy. They provide relief by selecting the inflammation at the harmed nerve root(s). You can purchase these medications without a prescription at a pharmacy.
- Oral corticosteroids: A brief course of oral (taken by mouth) corticosteroids may assist in the release of pangs by reducing swelling and inflammation all over the pinched whim-whams. You will need a prescription from your healthcare provider (doctor) for these medications.
Physical therapy for a pinched nerve in the neck
- Physical therapy and personal exercises focused on strength training and stretching your neck muscles can assist manage cervical radiculopathy. Again, your physical therapy regimen will be unique to you and turn on several factors, such as which area of your neck is affected and your overall physical health and abilities.
- In common, a physical therapy regimen for cervical radiculopathy will progress you through various stages as your pain improves, beginning with gentle range-of-motion exercises and adding strengthening and conditioning activities once the acute (severe and sudden) symptoms dim.
- Your physical therapy may also involve learning ways to have good posture and perform your job safely and comfortably.
- Furthermore, a definitive treatment progression for managing cervical radiculopathy has not been created, a general consensus occurs within the literature that utilizing manual therapy tricks in co-occurrence with therapeutic exercise is effective in considering increasing function, as well as active range of movement (AROM), focusing on decreasing levels of pain and disability will most such as be the main focus of the patient. Leteast high-level research confirms the positive outcomes of exercise therapy.
- If the patient has had long-term pain, an element of pain sensitization may have developed and chronic pain behaves variously to acute pain. Therefore education about pain and reconceptualization may be required.
Treatment options:
- Education and advice
- Manual remedy – PAIVMs (Passive Accessory Intervertebral Movements) or PPIVMs (Passive Physiological Intervertebral Movements) or NAGs (Natural Apophyseal Glides) or SNAGs (Sustained Natural Apophyseal Glides)
- Exercise Therapy – AROM, stretching and strengthening
- Postural re-education
Education and Advice
- Education is key to acquiring the patient side and working cooperatively with physiotherapy. If the patient understands the condition and the reason for the neck and arm pain then they are more such as to be compliant with any rehabilitation plan.
- In cases of a prolapsed disc, tobacco smoking causes condensation of the vascular network girding the intervertebral disc (IVD), decreasing the circular exchange of nutrients and anabolic agents from the blood vessels to the disc. Nicotine down-regulates the proliferation rate & glycosaminoglycan (monkeyshine) biosynthesis of slice cells.
- Nicotine mainly affects glycosaminoglycan (monkeyshine) attention at the cartilage endplate, dwindling it up to 65% of the value attained in normal physiological conditions. Tabacco mostly harms the nucleus pulposus, whose cell density and glycosaminoglycan (GAG) levels reduce up to 50% of their normal physiological levels.
- The effectiveness of quitting smoking on the rejuvenescence of a regressed intervertebral disc (IVD) looks limited benefit on the health of the disc. Cell-grounded remedies in confluence with bank conclusion should supply significant advancements in slice health, suggesting that, besides quitting smoking, fresh treatments should be enforced in the attempt to recover the health of an intervertebral slice( IVD) regressed by tobacco smoking.
Manual Therapy
- There are some contradictions in utilizing manual therapy techniques and their efficacy is questioned. Gross AR et al reported mobilization and/or manipulation when combined with exercise was salutary for pain relaxation and improvement of function for persistent mechanical neck disorders with or without headache, yet as a stand-alone treatment manipulation and/or mobilization was not beneficial. This is echoed in the latest literature. In a multimodal treatment model, the addition of manual therapy techniques (thought to improve the size of the intervertebral foramen of the affected nerve root) has no significant additional benefits compared to one another, neither was superior either. At best manipulations may only give short-term pain relief.
- Furthermore, cervical spine manipulation carries a risk of complications such as vertebral dissection and spinal cord compression because of massive disc herniation. Therefore, this intervention should be discouraged in cervical radiculopathy (pinched nerve in the neck), especially if imaging of the spine has not yet been performed.
- Fritz JM et al examined the effectiveness of cervical traction in addition to exercise in cases with cervical radiculopathy (pinched nerve in whim-wham). Joining mechanical traction to exercise for cases with cervical radiculopathy outgrowth in lower disability and pain, by oneself at long-term follow-ups.
- Boyles et al (2011) however found that manual remedy continuing thrust mobilizations of the cervical or thoracic spine and cervical non-thrust rellies (PA slides/Lateral Glides in ULTT1 position/Rotations/Retractions) were shown to be effective at reducing pain levels, increasing function and increasing joint ROM. When combined with exercise remedy it was more effective than the control group of manual remedy or exercise remedy still both control groups were effectively decreasing signs and symptoms.
- Persson et al highlighted that there was no significant variance between outcome measures of patients who had had surgery, physiotherapy, or cervical collar explaining that physiotherapy is at least as effective as surgery.
Muscle Energy Techniques
- Cleland et al used muscle energy techniques (MET) in 28 patients, with 46% entering positive outcomes. However, details of the techniques utilized were inadequate and a variety of techniques were used as it was down to the practitioner to decide which technique would be employed.
- The quality of research related to testing the effectiveness of muscle energy techniques (MET) is poor. Studies are generally little and at high risk of bias due to methodological deficiencies.
Neurodynamics – Gliding and Sliding/Tensioning
- Ragonese (2009) carried out the neurodynamics sliding and attaching ways, outlined by Butler, whilst having the case in an upper arm pressure position described by Magee led in a slow and oscillatory manner.
- With the enhancement in symptoms, the technique progressed to a ‘tension’ technique, described by Butler. Again, positive issues were observed in consideration of pain and function, although treatment duration was not recorded.
Exercise Therapy
- Exercise therapy has the most positive and lasting results for the condition. Exercises targeted at opening the intervertebral foramen are the best option for decreasing the impact of radiculopathy. Exercises such as contralateral rotation and side flexion are amongst the simplest forms of exercises which are effective against signs and symptoms, given in the form of active range of motion (ROM). Due to the intricate and close relationship of muscles on the intervertebral foramen and the likely presentation of reduced range of motion (ROM), stretching is also an effective form of treatment to regain range of motion (ROM).
- Once the range of motion (ROM) increases strengthening exercises can be performed to develop stability and reduce the threat of developing nerve root irritation in the future, as long as it is not caused by a structure that cannot be influenced by physical therapy. During the original stages of treatment, strengthening should be limited to isometric exercises in the included upper limb. One time the radicular symptoms have been resolved, increasing isotonic strengthening can start. This should initially include low-weight and high repetitions (15-20 repetitions). Closed kinetic chain activities can very assist in rehabilitating weak shoulder girdle muscles. However, Griffiths et al found no significant variance with the addition of specific neck stabilization exercises to a program of common neck advice and exercise.
- The patient should be instructed to same as active as possible and perform exercises daily on the days between therapy sessions. Written exercise instructions should then be available. We suggest a two-component program, as suggested by Fritz JM et al. 2 components: scapula strengthening & cervical strengthening.
- Cervical strengthening exercises should involve supine craniocervical flexion to evoke compression of the deep neck flexor muscles without compression of superficial neck muscles. Feedback utilizing an air-filled pressure detector or tactile cues can be useful. The patient should perform three sets of ten contractions for ten seconds with proper muscle activation. Craniocervical flexion contractions were executed with the case seated, with the thing of 30 repetitions of 10-second contractions.
- Scapular retraction against resistance utilizing elastic bands or pulleys can be added. Scapular-strengthening exercises involved prone horizontal abduction, side-lying forward flexion, a prone extension of each shoulder, as well as prone push-ups with emphasis on shoulder protraction. The goal was three sets of ten repetitions, with resistance added as tolerated.
Cervical epidural steroid injections for a pinched nerve (whim-wham) in the neck
- A cervical epidural steroid injection (cervical ESI) is an injection of anti-inflammatory medicine — a steroid or corticosteroid — into the epidural duration all over the spinal nerves in your neck. The important thing about cervical epidural steroid injections for cervical radiculopathy is to assist manage pain caused by irritation and inflammation of the spinal nerve roots in your neck.
- Although cervical epidural steroid injections (cervical ESIs) do not relax the pressure on the whim-wham caused by a narrow foramen or by a bulging or herniated disk, they may lessen the lump and relieve the pain long enough to allow the harmed whim-whams to recover.
- Around 40% to 84% of people who get a cervical epidural steroid injection experience at least incomplete pain relaxation. But some people do not experience any pain relief.
- Cervical epidural steroid injections (Cervical ESIs) have potentially serious side effects and complications. Be sure to ask your healthcare provider (doctor) about the benefits & risks of getting a cervical epidural steroid injection (cervical ESI).
Surgery for a Pinched nerve (whim-wham) in the neck
- Your healthcare provider may recommend surgery if you are passing severe and persistent pain despite trying nonsurgical remedies for at least 6 to 12 weeks or if you are passing serious or worsening neurological issues due to cervical radiculopathy.
- Several various surgical procedures can treat cervical radiculopathy. The procedure your healthcare provider( croaker ) recommends will depend on numerous factors, involving what symptoms you have, your overall health, and the position of the affected whim-whams root.
Is the Pinched nerve in the neck curable?
- While non-surgical treatment options generally successfully manage the symptoms of cervical radiculopathy, there is no cure for the degenerative differences (age-related wear and tear and gash) in your cervical spine that can cause cervical radiculopathy (pinched whim-wham in the neck).
How can I prevent a Pinched nerve in my neck?
While you can not always help cervical radiculopathy, there are certain effects you can do to drop your trouble, involving:
- Maintaining a healthy weight
- Staying physically fit
- Practicing good posture
- Doing stretching exercises to retain your muscles strong and flexible.
Specific risk factors for creating cervical radiculopathy involve:
- Manual labor that includes heavy lifting and/or operating vibrating equipment,
- History of chronic smoking,
- Prior lumbar (lower back) radiculopathy,
- Playing golf.
- If any of these risk factors apply to you, it is important to talk to your healthcare provider (doctor) about specific effects you can do to try to prevent cervical radiculopathy.
What is the prognosis (outlook) for the Pinched nerve in the neck?
The prognosis (outlook) for cervical radiculopathy turns on several factors, involving:
- Which spinal nerve is affected,
- The cause of cervical radiculopathy,
- How severe your symptoms are,
- Your overall health.
- In utmost cases, people who go through nonsurgical treatment have the stylish prognostic and their symptoms vanish. In fact, multitudinous people who have pinched whim-whams in the neck can treat it at the place with time and rest.
- Still, symptoms of cervical radiculopathy recur (come back) in over one-third (1/3) of people with latterly quick improvement.
- If your symptoms come back, it is important to talk to your healthcare provider (doctor).
When should I look to my healthcare provider about a Pinched nerve in nerve?
- If you have symptoms of cervical radiculopathy, such as pain that radiates down your neck, that does not go away after a week or more of rest, contact your healthcare provider (doctor). If you have more severe symptoms, such as muscle weakness or weakened reflexes in your arm, communicate with your healthcare provider (doctor) as soon as possible.
- If you are experiencing neck pain later in an accident, such as a fall, communicate with your healthcare provider (doctor) or go to the nearest hospital.
Summary
- Having A Pinched nerve in the neck (cervical radiculopathy) can be uncomfortable and annoying. The best news is that utmost cases of this condition go away with at-home rest over time. If your symptoms persist for further than a week, talk to your healthcare provider (croaker). Several nonsurgical curatives can treat cervical radiculopathy (pinched nerve in the neck). To help pinched nerve in the neck, ask your healthcare provider (doctor) about ways to retain your chine happy and healthy.
FAQs
Anterior Cervical Diskectomy and Fusion (ACDF) is the most commonly performed procedure to treat cervical radiculopathy. The procedure includes removing the problematic disk or bone spurs and then stabilizing the spine through spinal fusion.
In the utmost cases, the pain of a pinched nerve in the neck begins at the neck and moves down the arm in the section served by the damaged vagrancy-wham. This pain is commonly described as burning or sharp. Certain neck movements—similar to extending or straining the neck or turning the head—may ameliorate the pain.
Once properly diagnosed, cervical radiculopathy can be managed in a variety of ways. It may take from one to twelve weeks for your nerves to whole heal once the pressure on the cervical nerve has been relieved. If this condition is left untreated, then there is the potential for very severe outcomes.
Cervical radiculopathy can be diagnosed with a thorough history and physical examination in many cases, yet MRI should be used to confirm the diagnosis. The affected dermatomes can both overlap and differ for a certain nerve root in cervical radiculopathy.
Commonly improving your posture, over-the-untoward medicine or at-home physical therapy exercises are the only treatments you will need to relieve radiculopathy symptoms. In fact, certain cases of radiculopathy increase with no treatment at all.
It can be accompanied by motor, sensory, or reflex poverties and is most frequent in persons 50 to 54 years of age. Cervical radiculopathy most sometimes stems from degenerative disease in the cervical spine.
Risk Factors: Men are affected slightly more sometimes than women. Risk factors for this condition involve weighty manual labor taking lifting, driving, operating a wobbling outfit, neck trauma (from sports or a motor vehicle accident), & previous spinal nerve injury.
Cervical foraminal stenosis is the most usual cause of cervical radiculopathy. Cervical herniated disc. If the inside substance of the cervical disc discharges out and inflames the conterminous vagrancy-whams, it can cause cervical radiculopathy.