Trochanteric Bursitis
Table of Contents
Introduction
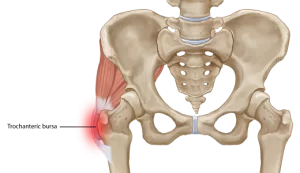
Trochanteric bursitis is a condition that causes pain and inflammation in the bursa sac located near the greater trochanter, which is the bony protrusion on the upper part of the femur or thigh bone. The bursa sac is a small, fluid-filled sac that acts as a cushion between the muscles, tendons, and bones around the hip joint. When it becomes inflamed or irritated, it can cause discomfort and pain in the hip area.
What are the Causes of Trochanteric Bursitis?
Trochanteric bursitis is a condition that is caused by inflammation of the bursa sac located near the greater trochanter of the hip bone. The bursa sac is a fluid-filled sac that helps to cushion and reduce friction between the muscles, tendons, and bones around the hip joint. There are several factors that can contribute to the development of trochanteric bursitis, including:
- Overuse or repetitive stress: Overuse of the hip joint or engaging in activities that require repetitive hip movements, such as running, cycling, or standing for long periods, can irritate the bursa sac and cause inflammation.
- Trauma or injury: A direct blow to the hip or a fall can cause trauma or injury to the bursa sac, leading to inflammation and pain.
- Muscle imbalances: Muscle imbalances around the hip joint, such as weakness in the hip abductor muscles or tightness in the hip flexor muscles, can lead to increased stress and friction on the bursa sac, resulting in inflammation.
- Arthritis: Osteoarthritis or rheumatoid arthritis can cause inflammation in the joints, including the hip joint, which can lead to trochanteric bursitis.
- Incorrect posture: Poor posture, such as sitting or standing for long periods in a position that places undue stress on the hips, can contribute to the development of trochanteric bursitis.
- Obesity: Being overweight can put additional stress on the hips, leading to increased friction and inflammation of the bursa sac.
- Previous hip surgery: Surgery on the hip joint, such as a hip replacement or repair of a hip fracture, can cause irritation and inflammation of the bursa sac.
It is important to note that not everyone who engages in activities that place stress on the hips will develop trochanteric bursitis. However, individuals who have any of the above risk factors may be more prone to developing this condition. If you are experiencing hip pain, it is important to seek medical attention to determine the underlying cause and appropriate treatment.
Symptoms of Trochanteric Bursitis
The symptoms of trochanteric bursitis can vary depending on the severity of the condition, but some common symptoms include:
- Pain on the outside of the hip: The most common symptom of trochanteric bursitis is pain on the outer part of the hip, over the greater trochanter. This pain may be sharp or dull and can be aggravated by activities that involve hip movement, such as walking, running, or climbing stairs.
- Tenderness: The area around the inflamed bursa sac may be tender to the touch, and pressure on the hip may exacerbate the pain.
- Swelling: In some cases, trochanteric bursitis can cause swelling in the hip area, which may be accompanied by redness or warmth.
- Stiffness: Trochanteric bursitis can cause stiffness in the hip joint, which may make it difficult to move the hip or perform certain activities.
- Difficulty sleeping: The pain and discomfort associated with trochanteric bursitis may make it difficult to find a comfortable position to sleep in, particularly when lying on the affected hip.
- Hip weakness: In some cases, trochanteric bursitis can cause weakness in the hip muscles, which may make it difficult to perform certain activities or movements.
It is important to seek medical attention if you are experiencing any of these symptoms, as untreated trochanteric bursitis can lead to chronic pain and disability.
Diagnosis
The diagnosis of trochanteric bursitis typically involves a combination of medical history, a physical examination, and imaging tests. Here are some of the steps that may be involved in diagnosing trochanteric bursitis:
- Medical history: Your healthcare provider will ask you questions about your symptoms, medical history, and any activities or events that may have contributed to your hip pain.
- Physical examination: Your healthcare provider will perform a physical examination to assess your hip joint for signs of inflammation or tenderness. They may also check your range of motion and hip strength.
- Imaging tests: Imaging tests, such as X-rays, MRIs, or ultrasounds, may be ordered to help confirm the diagnosis of trochanteric bursitis and rule out other conditions that may be causing your symptoms, such as a hip fracture or arthritis.
- Injection test: In some cases, your healthcare provider may perform an injection test, in which a local anesthetic and corticosteroid are injected into the bursa sac to see if it provides pain relief. If the injection provides significant relief, it may confirm the diagnosis of trochanteric bursitis.
It is important to see a healthcare provider if you are experiencing hip pain or other symptoms, as early diagnosis and treatment can help prevent the condition from becoming chronic and causing long-term disability.
Treatment of Trochanteric Bursitis
The treatment for trochanteric bursitis typically involves a combination of conservative measures and medication. In more severe cases, surgery may be necessary to remove the inflamed bursa sac. Here are some of the treatment options for trochanteric bursitis:
- Rest and activity modification: Resting the affected hip and avoiding activities that aggravate the pain can help reduce inflammation and promote healing. Your healthcare provider may also recommend modifications to your daily activities to reduce pressure on the hip joint.
- Ice therapy: Applying ice to the affected hip can help reduce pain and swelling. Ice can be applied for 10-20 minutes at a time, several times a day.
- Physical therapy: A physical therapist can develop an exercise program to strengthen the hip muscles and improve flexibility, which can help reduce pain and prevent future flare-ups.
- Medication: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help reduce pain and inflammation. In more severe cases, corticosteroid injections may be recommended to provide more immediate pain relief.
- Surgery: In rare cases, surgery may be necessary to remove the inflamed bursa sac. This is typically only recommended if conservative measures have failed to provide relief and the pain and disability are severe.
It is important to follow the recommended treatment plan for trochanteric bursitis to reduce pain and prevent future flare-ups. Your healthcare provider can recommend the most appropriate treatment plan based on the severity of your condition and your overall health.
Physiotherapy Treatment in Trochanteric bursitis
The conservative physiotherapy management of trochanteric bursitis involves a variety of treatments to reduce pain and inflammation and to restore mobility and function to the hip joint. Here are some of the conservative physiotherapy management techniques for trochanteric bursitis:
- Rest and activity modification: Resting the affected hip and avoiding activities that aggravate the pain can help reduce inflammation and promote healing. Your physiotherapist may also recommend modifications to your daily activities to reduce pressure on the hip joint.
- Ice therapy: Applying ice to the affected hip can help reduce pain and swelling. Ice can be applied for 20 minutes at a time, several times a day.
- Manual therapy: Manual therapy techniques, such as massage, joint mobilization, and stretching, can help reduce pain and restore mobility to the hip joint.
- Exercise therapy: Your physiotherapist can develop an exercise program to strengthen the hip muscles and improve flexibility, which can help reduce pain and prevent future flare-ups. Exercises may include hip abductor and adductor strengthening exercises, hip flexor and extensor stretching exercises, and balance and proprioception exercises.
- Education and self-management: Your physiotherapist can provide education on proper posture, body mechanics, and ergonomics, as well as self-management strategies to help manage pain and prevent future flare-ups.
Post-operative physiotherapy management:
Post-operative physiotherapy management of trochanteric bursitis typically involves a progressive rehabilitation program to restore strength, mobility, and function to the hip joint. Here are some of the post-operative physiotherapy management techniques for trochanteric bursitis:
- Pain management: Your physiotherapist can provide modalities, such as ice, heat, and electrical stimulation, to help manage pain and reduce inflammation.
- Range-of-motion exercises: range-of-motion exercises can help restore mobility to the hip joint and prevent stiffness.
- Strengthening exercises: Strengthening exercises can help restore strength to the hip muscles and improve overall function.
- Gait training: Your physiotherapist can provide gait training to help you walk properly and without pain.
- Gradual return to activity: Your physiotherapist can develop a gradual return to activity program to help you safely return to your pre-injury level of activity.
It is important to work closely with your physiotherapist to develop an individualized treatment plan that meets your specific needs and goals. Following the recommended, conservative or post-operative physiotherapy management plan can help you recover from trochanteric bursitis and prevent future flare-ups.
Precaution
There are some precautions that individuals with trochanteric bursitis can take to prevent or reduce the risk of flare-ups. Here are some common precautions:
- Avoid repetitive activities that put pressure on the hip joint, such as running, jumping, or climbing stairs.
- Maintain a healthy weight, as excess weight can put extra strain on the hip joint.
- Wear supportive shoes with good cushioning to reduce the impact on the hip joint during daily activities.
- Use proper form and technique when performing exercises or sports activities to avoid putting unnecessary strain on the hip joint.
- Warm up before exercise or physical activity to prepare the muscles and joints for activity.
- Stretch regularly to improve flexibility and reduce muscle tension in the hip joint.
- Use proper body mechanics and posture when sitting, standing, or lifting to avoid putting strain on the hip joint.
It is important to speak with a healthcare provider or physical therapist before beginning any new exercise or activity program to ensure that it is safe and appropriate for your individual needs and condition.
Conclusion
Trochanteric bursitis is a common condition that can cause pain and discomfort in the hip area. However, with proper diagnosis and treatment, most patients can achieve relief from their symptoms and return to their normal activities. If you are experiencing hip pain, it is important to seek medical attention to determine the underlying cause and appropriate treatment.
FAQs
Does trochanteric bursitis go away?
In many cases, trochanteric bursitis can go away with proper treatment and self-care. The time it takes for the condition to resolve can vary depending on the severity of the inflammation, the underlying cause, and the effectiveness of the treatment. Mild cases of trochanteric bursitis may resolve within a few weeks of treatment, while more severe cases may take several weeks or even months to heal completely.
It is important to note that while trochanteric bursitis may go away with treatment, it can recur in some cases, particularly if the underlying cause is not addressed. Maintaining good hip mechanics, stretching regularly, and avoiding activities that aggravate the condition can help prevent a recurrence. It is recommended to seek medical advice for a proper diagnosis and treatment of trochanteric bursitis.What are the three symptoms of bursitis?
Bursitis is a condition that occurs when the bursae, small fluid-filled sacs that cushion and lubricate the joints, become inflamed. The common symptoms of bursitis include:
Pain: The affected joint may be painful, especially with movement or pressure on the area.
Swelling: Inflamed bursae can become swollen, making the affected joint feel tender and warm to the touch.
Limited range of motion: The inflammation and pain associated with bursitis can make it difficult to move the affected joint fully, leading to stiffness and a reduced range of motion.At what age do you usually get bursitis?
Bursitis can occur at any age, but it is more common in adults over the age of 40. As people age, their joints can become less flexible, and the bursae can lose some of their protective fluid, making them more susceptible to inflammation and injury. However, bursitis can also occur in younger adults and even children, particularly if they engage in activities that put repetitive stress on the joints, such as sports, manual labor, or playing a musical instrument. Other factors that can increase the risk of developing bursitis include obesity, certain medical conditions, and previous joint injuries.
Does bursitis show up on an x-ray?
Bursitis itself does not show up on an x-ray because it is an inflammation of the bursa, which is a small fluid-filled sac near the joint. However, an x-ray can be useful in ruling out other conditions that may be causing the symptoms, such as arthritis or a fracture. An x-ray can also show changes in the bones or joints that may be related to bursitides, such as bone spurs or degenerative joint disease. In some cases, an MRI or ultrasound may be needed to confirm the diagnosis of bursitis and evaluate the extent of the inflammation.
Is bursitis permanent?
In many cases, bursitis is not permanent and can be treated effectively with rest, physical therapy, and other conservative measures. With proper treatment, the symptoms of bursitis, such as pain and inflammation, can be reduced or eliminated, and the affected joint can regain normal function. However, if the underlying cause of bursitis, such as joint damage or repetitive stress, is not addressed, the condition can recur or become chronic, leading to long-term inflammation and pain. In some cases, surgery may be necessary to remove the inflamed bursa or repair damaged tissues. It’s important to seek medical advice for proper diagnosis and treatment of bursitis and to follow a comprehensive treatment plan to prevent a recurrence of the condition.