Dislocation of Atlanto-occipital joint
Table of Contents
What is Atlanto-occipital dislocation?
The atlantooccipital dislocation, orthopedic decapitation, or internal beheading describes the ligamentous detachment of the spinal column from the skull base. A human can survive such an injury: however, 70% of patients result in immediate death. The joint dislocation defines the ligamentous detachment between the 1st & 2nd cervical vertebrae.
Mechanism atlantooccipital dislocation
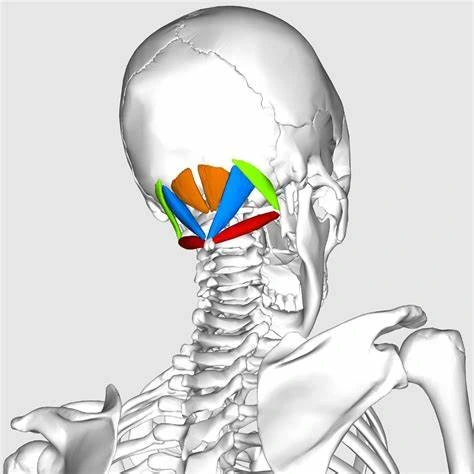
This damage is a development of a disruption of the stabilized ligaments between the C1 vertebral body, the skull base, and the occiput, this is known as the atlas. The diagnosis is generally supposed by history & physical exam but confirmed by imaging, generally by CT due to its more immediate speed in the acute trauma setting, although MRI can also assist with assessment in equivocal cases.
The treatment is starting stabilization with a cervical spine collar, & then surgical intervention in cases in which deterioration of paralysis is possible. The most typical mechanism of harm is high-speed motor vehicle accidents. This injury is more common in juveniles due to the immense size of their heads comparable to their bodies, and the more horizontal exposure of the occipital condyles. It describes <1% of all cervical spine injuries.
Many subtypes of atlantooccipital dislocation are known. One proposed categorization scheme contains the anterior, vertical, and posterior of the head relative to the spine. Other variants with lateral and rotatory displacement have been related, as well as mixed types. A common etiology for such damages is sudden & intense deceleration causes a whiplash-like mechanism.
Cause of Atlanto-occipital dislocation
Trauma is the main cause of Atlanto-occipital instability, however, connective tissue diseases can also cause hypermobility & injury.
What are the types of Atlanto-occipital dislocation?
Occipitoatlantal subluxation is categorized into 3 main types (Trayneli’s Classification), however, they can arise in combination as well.
- Anterior dislocation of occiput over the atlas
- Traction or Longitudinal Dislocation
- Posterior Dislocation
Symptoms of atlantooccipital dislocation
The atlantooccipital dislocation can be asymptomatic or can present with signs and symptoms of constriction to the brainstem or cervical cord. The symptoms can involve motor or sensory neurological deficiencies, cranial nerve deficiencies, and cervical-medullary syndrome.
Diagnosis Atlanto-occipital dislocation
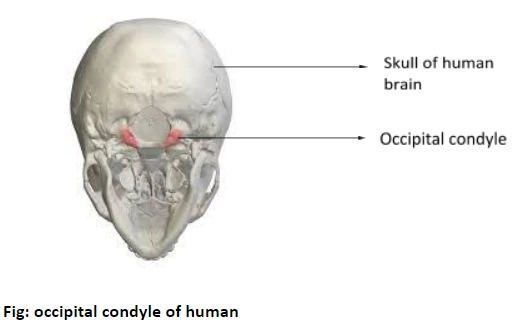
The distances between the dens & covering structures are also key features that can recommend the diagnosis, with the normal distance between the dens & basion (BDI) measuring less than 9 mm on CT, & the distance between the dens & atlas (ADI) measuring less than 3 mm on CT, although this can be raised in cases of rheumatoid arthritis due to pannus formation.
Several indirect measures on CT can be used to evaluate ligamentous integrity at the craniocervical junction. The Wackenheim line, a straight line stretching along the posterior margin of the clivus via the dens, should not cross the dens on plain film, with violation of this relationship increasing concern for basilar invagination. The basion to axion interval is also used, which is defined by calculating the distance between an imaginary perpendicular line at the anterior skull base, or basion, at the foramen magnum, & the axis of the cervical spine along its posterior margin, which should measure 12 mm, an estimate more dependable on radiograph than CT. The gap between the atlas & the occipital condyles should be less than 4 mm, & is better evaluated on coronal images.
The administration ratio was previously used, which was the end of the basion to the spinolaminar line, and it was divided by the space from the tip of the opisthion to the midpoint of the posterior part of the anterior arch of C1. It is no longer advised due to low sensitivity & difficulty acknowledging landmarks. It is also the vertical or posterior displacement of the cervical spine.
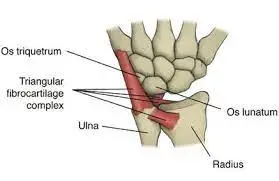
Other dimensions involve occiput-atlas distance, the angle between the anterior arch of the atlas & the axis, the vertical distance between the posterior arch of the atlas & spinous process of the axis, the vertical Atlanta-dens interval, & joint space between C1 & C2.
Prognosis
The damage is instantly fatal in 70% of cases, with an additional 15% enduring in the emergency room but dying during the subsequent hospital stay. A basion dental gap of 16 mm and greater is associated with mortality. In those with neurologic deficiencies, survival is unlikely.
Most deaths result from mechanical injury to the spinal cord and lower brainstem, going from a localized contusion to diffuse axonal injury to a complete transaction. Vascular difficulties are also frequent & may contribute immensely to delayed mortality. Combined dissections of the vertebral & carotid arteries can cause extreme cerebral ischemia, whereas rupture of the vertebral artery or PICA junction results in subarachnoid hemorrhage compressing the brainstem.
Hydrocephalus may also create & cause a dangerous increase in intracranial pressure. Further possible difficulties involve damage to prevertebral structures (pharynx, lower cranial nerves) & the cerebellum. Therefore, starting survivors of atlantooccipital dislocation may show severe & variable neurologic deficits, involving reversible or irreversible tetraplegia, multiple cranial nerve deficiencies, loss of consciousness, & recurrent respiratory or cardiac arrests. Isolated cases of near-complete healing after life-threatening symptoms are known.
In the case of posterior removal of the head, a simultaneous fracture of the atlas with backward migration of the posterior arch is associated with an improved chance of survival, as this allows the spinal cord & medulla to migrate backward without obtaining crushed.
Proximal cervical fractures associated with injury
Jefferson fracture can be connected with Proximal cervical fractures, with the C1 ring/ atlas, being fractured in many areas, allowing the spine to shift forward comparable to the skull base. The Hangman’s fracture which is a fracture of the C2 vertebral body and dens of the cervical spine upon which the skull base poses to permit the head to rotate can also be associated with an atlantooccipital dislocation. The fracture is not generally associated with a hanging mechanism of damage.
Treatment
Conservative & surgical treatments
Primary treatment involves cervical spine immobilization using a halo cervical collar. Although halo immobilization & traction are contraindicated in the management of AOD because of the threat of displacement of the damaged occipital-cervical joint.
Cervical traction is never used, but again, others state to use of cervical traction.
Surgical fusion is later done when suggested. Postoperative hydrocephalus is frequent & should be inferred when the neurologic deterioration occurs after fixation. Those who endure AOD will likely have residual neurologic deficiencies.
Physiotherapy Treatment
Medication, massage therapy & steroid injections are common forms of treatment for atlantooccipital dislocation pain. Specific exercises may also offer to relieve pain. Consult the doctor before trying these exercises. Do the following exercise after some time of surgery.
Simple Exercises Can Reduce Symptoms
Simple exercises can help relieve pain in the C1 to C2 neck region. If the pain is only in the neck, executing these exercises regularly could help eliminate the pain.
- Supine Neutral Head Position
- Supine Cervical Retraction
- Upright Neck Retraction
- Savasana
- Neck Extension and Flexion
- Sub-Occipital Neck Stretch
- Neck Rotation
Supine Neutral Head Position
The patient’s position is to lie on the back either with your head directly on the ground or a very thin pillow or folded blanket. Then, let your head fall back so it aligns with the shoulders & hips as much as comfortable. Remain in this exercise position for 5 to 10 minutes. Do this every couple of hours while you are undergoing neck pain.

Supine Cervical Retraction
The patient’s position is to lie down on your back with your head in a neutral position. Then, tuck the chin as if you’re trying to make a dual chin. Keep your head on the ground. After, then feel a stretch in the back of the neck & compression in the front of the neck. Maintain this position for two seconds, and then release & repeat the exercise for a total of 8 – 10 repetitions.
Upright Neck Retraction
The patient’s position is sitting or standing with good posture, then push gently on your chin with the fingers & move your head backward as far as is comfortable. Keep the face pointing forward, and feel the stretch in the back of the neck & compression in the front of the neck. Maintain the exercise position for a few seconds, after then release. Repeat this exercise for of 8 – 10 repetitions.

Savasana
Relaxation is usually recommended for people with atlantooccipital. Savasana is a yoga posture that can lead to deep relaxation, and relieve neck pain, and headaches, especially when acted with appropriate head support, such as a folded blanket and low pillow. The patient’s position is to lie on the back & put the pillow or folded blanket under the head. After, then use an eye bag over the eyes for additional relaxation. Then, allow your legs to rest in a natural position & rest your arms by your sides, palms facing up. Then, relax in this pose for up to 15-30 minutes, and back to the starting position.
Neck Extension and Flexion
The patient’s position is to sit in a chair with the hands resting on the knee. Then neck extension movements alleviate tension in the back, front, and sides of the neck & can loosen tight muscles at the base of the head. Look forward & keep the head & neck in line with your spine. After then slowly bend your head back to look at the roof. Bring the head back to the center. Tilt the head forward, dropping your chin to your chest. And then back to the starting position. Do this exercise with 5 to 10 repetitions.
Sub-Occipital Neck Stretch
The patient’s position is to sit in a straight-backed chair with the head & neck in line with the spine. Then place the pointer & middle finger of the right hand on the chin. After then push the chin back gently, as though are trying to make a double chin. Hold the mouth closed, and try to move just the head back towards the back of the wall behind you. They should feel a stretch along the back & sides of your neck & the base of the skull. Maintain the stretch for a few seconds, and then release.
Neck Rotation
The patient’s position is to sit in a chair or stand with the neck & head in line with the spine. After then slowly rotate the head to the right, keeping your head straight, stretching as far as you can without pain or strain. Look over the right shoulder & maintain the stretch for a few seconds. Bring the head back to the center & rotate the head to the left, looking over the left shoulder. Maintain the stretch for a few seconds & back the head to the center. Repeat this stretch many times every.

Perform Regular Strengthening Exercises
Pain often overlaps with weakness in the muscles of not only the neck but also the upper back and core. Including both strengthening & stretching exercises can stimulate blood flow to the site to speed healing. These exercises will also enhance your ability to function in daily life & make maintaining good posture easier. It can even control further injury to the neck.
- Isometric Strengthening
- Prone Head Lifts
- Supine Head Lifts
- Scapular Retractions
- Neck Rotations
Isometric Strengthening exercise
The patient’s position is up straight in a chair with the back supported, and place your head in neutral. Put the hand on your forehead & apply pressure, while at the same time pressing your head forward with the power of your neck. after, then try to hold your head in a neutral position. Then, push your forehead against your hand & your hand against your forehead for 5 to 10 seconds, and relax. Repeat this exercise 3 – 4 times. Do the exact thing with your hand on the back of your head, trying to press your head back into the hand while holding a neutral head position. Press as hard as you can for 5 to 10 seconds, and then relax. Repeat this exercise 3- 4 times. Place the hand on one side of the head & push against it, maintaining the head in a neutral position. Hold for 5 to 10 seconds & switch sides, repeat 3 to 4 times on both sides.
Prone Head Lifts
The patient’s position is to lie face down on the ground or on a mat. Maintain yourself up on the forearms & allow the head to hang heavy in front of you. Raise the head to the neutral position as you retract the chin. Then, continue to lift your head & look upward, feeling a stretch along the front of your neck. Hold for 4 to 8 seconds, return to a neutral chin-tucked position, and then back to the starting position with the head hanging. Repeat this exercise 4-5 five times, and 2 times every day.

Supine Head Lifts
The patient’s position is to lie on the back of a mat with the knees bent & feet flat on the ground, then arms extended alongside you. After, then lift your head off the ground, and bring your chin to the chest. Maintain this exercise for 4 to 5 seconds, and then release. And, then repeat this exercise 8 to 10 times and 2 times every day.
Scapular Retractions
The patient’s position is to stand with the arms extended at your sides & head and neck in a neutral position. Then, lift your chest & pull the shoulders back & down, squeezing the shoulder blades together. Maintain this position for 8 to 10 seconds to start, and work up to 30 seconds. Do this exercise for 4 to 5 repetitions, and 2 times every day.
Simple active range-of-motion [ ROM ] exercises can also help heal & relieve pain. Simply moving the head in directions that don’t cause you pain can provide nutrition & lubrication to sore places & movement of joints & muscles can send signals to the nervous system to block pain.
FAQ
Atlantooccipital dislocation, orthopedic beheading, or internal decapitation describes the ligamentous detachment of the spinal column from the skull base. A human can survive such an injury: however, 70% of patients result in rapid death.
Atlanto-occipital dissociation deteriorations are many & contain both atlanto-occipital dislocations & atlanto-occipital subluxations. The tectorial membrane & alar ligaments supply most of the stability to the atlanto-occipital joint, & injury to these ligaments results in instability due to lower inherent skeletal stability.
Activities are an ellipsoid joint, and the atlantooccipital joint permits motion in 2 degrees of freedom. These are flexion-extension & lateral flexion. However, the main activity unrestricted at the atlantooccipital joint is that of flexion–extension.
The space between the atlas & the occipital condyles, the atlanto-occipital interval (AOI), should estimate at less than 4 mm & is better evaluated on coronal illustrations.