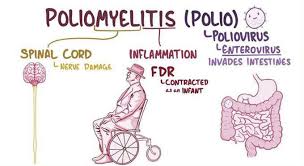
Poliomyelitis
Table of Contents
Definition
Poliomyelitis or Polio is a virus infection of cranial nerve nuclei inside the brain stem or spinal cord that leads to temporary or permanent paralysis of muscles that they activate. The virus most usually affects children under 5 years of age.
Way of transmission
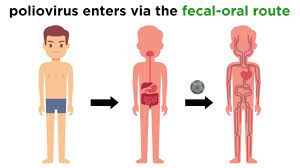
- The spread is mainly by fecal contamination way and by droplet infection.
- Poliovirus is an Enterovirus that colonizes the GIT.
Epidemiology of poliovirus
Polio is mainly caused by a virus of 3 types:
- Type-1-Brunhilde,
- Type-2-Lanchi,
- Type-3-Leon.
- At the time of the launch of the Global Poliomyelitis Eradication Initiative in 1988, there is a considerable increment in the spread of the virus.
Prevalence
- Because of vaccination, The prevalence is so minimum.
- Thirty-three cases were identified in 2018.
Pathology
Alimentary Stage-
- After obtaining access to the body through the nasopharynx on the GIT, the virus multiplies in the epithelial cells of the intestinal mucosa.
Viremic Stage-
- The virus escalates through the bloodstream and after a sort of conflict between the virus and the antibodies, in case the virus turns victorious then it majors to the 3rd stage.
Neural Stage-
- The virus finds its route to the anterior horn cells of the spinal cord and nerve cells in the brain stem..-
Symptoms of Poliomyelitis
The course of the disease is spreading into four stages:
Prodromal Stage or Pre-Paralytic Stage-
- It lasts for a few hours to a few days and one to three days is the usual duration.
Signs and Symptoms of the prodromal stage
- Headache.
- Sore throat.
- Malaise.
- Slight Cough.
- Diarrhea or constipation.
- Backache.
- Joint pains.
- Pyrexia of variable duration and severity.
- Mild neck stiffness.
- Irritability.
Treatment of prodromal stage
- The only practical measures which may be taken are to stop playing games and other some manual work if possible.
- The nasopharyngeal secretions and feces or greatly effective at this stage of illness. In addition, a booster dose can be given.
Acute Stage-
- It last up to three to six weeks from the onset of Poliomyelitis.
Signs and Symptoms for acute stage
- Muscle tenderness is the most crucial sign seen in this stage.
- To test this just press the calf muscles when a child is sleeping.
- If the child cries, he has tenderness.
Treatment of acute stage
- Rest-The child should not be over-handled.
- Isolation
- Booster dose
- Nutrition-Diet rich in” Protein”.
Sister Kenny’s Bath:
- This is a type of moist heat. This helps to decrease inflammation to some extent.
- Massage should not be given as it can cause more damage because of which the patient can not be able to walk later on.
Convalescent Stage-
- Duration three months.
Signs and Symptoms of the convalescent stage
Spinal Type-
- The” lower limb muscles are more often involved”.
- Flexion contractures of the hip, and knee and equinus deformity of the ankle are normal.
Bulbar Type-
- The most crucial sign of Bulbar paralysis is- the ” inability to swallow” because of pharyngeal paralysis.
- The patient needs quick ventilatory support for respiration and Ryle’s tube for feeding to save a person’s life as both respiratory and swallowing muscles are affected.
- The “early signs” of respiratory involvement involve breathing, the feeling of suffocation, slight cyanosis, use of sternomastoid, alae nasal, and other accessory muscles of respiration.
Spinobulbar-
- This kind has a combination of both spinal and bulbar types.
Postencephalic-
- Mental disturbance, coma, paralysis of facial muscles, and symptoms similar to meningitis such as headache, vomiting, and neck stiffness can happen.
Treatment of Convalescent Stage
- Muscle Charting.
- Positioning.
- Changing the position-Turning the patient every two to four hours and night prevents bed sores and keeps up the skin dry.
Stage of Recovery-
- This stage extends for almost two years.
- Thus muscles in the polio patient may be strengthened to their maximum capacity for up to two years.
Stage of Residual Paralysis- Post-Polio Syndrome
Treatment for Stage of Residual Paralysis
- The patient is given a combination of stretching, strengthening, and calliperization.
- Tailor-made calipers may prevent the deformity from aggravating.
- Tendon transfers can be done for compromising the balance on that side.
Surgical treatment
- Arthrodesis
- Arthrodesis
- Usual Problems Encountered by Polio Patients
Muscle weakness
- Bony Changes-Most usual changes are-Shortening, Ostoporesis, and Deformities.
Poliomyelitis Treatment
If a person has polio, the doctor will focus on making sure that the person is comfortable and try to prevent any other health issues. Some treatments and tools for support involve:
- Pain relievers (like ibuprofen)
- A ventilator (a device that helps a person breathe)
- Physical therapy may help keep the muscles working
- Bed rest and fluids for flu-like symptoms
- Antispasmodic medications to relax muscles
- Antibiotics for urinary tract infections
- A heating machine for muscle aches and spasms
- Corrective braces
- Pulmonary rehabilitation to help with lung complications
- A mobility aid like a cane, wheelchair, or electric scooter
Physiotherapy Treatment for Poliomyelitis
Exercise programs for polio patients are specifically designed to the individual’s functional status and requirements. The exercises should not overly fatigue the patient as these may reduce the patient’s functional level. Physiotherapy treatment of post-polio muscular pain may incorporate activity declination, pacing (rest periods during activity), thermotherapy, cryotherapy, transcutaneous electrical stimulations (TENS) and stretch use of assistive devices, and lifestyle modifications.
Inspiratory Muscle Training:
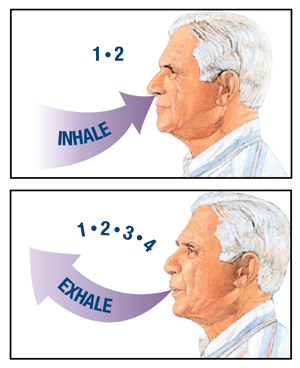
- Inspiratory muscle training can be done at home by using a spirometer or Deep breathing exercises.
- The patient performs training for twenty minutes with one minute of exercise, one-minute rest, and repeat ten times, done every day for a period of ten to fourteen weeks.
Active and Passive Movements of Joints:
- Joint movement exercises are not suggested when the muscles are in spasm or are very tender.
- Without reducing the pain simple activities are done for hips, ankles, and other joints to keep them mobile through a full range each day.
- In the cases of paralyzed joints, active movements can have to be replaced by passive movements.
Posture Splinting and Support:
- Correct posture of the patient in bed is maintained to put a stop to deformities.
- Detachable supports like above-knee calipers, support knees, and ankles, keep up the knee at the level and also help to stop any hip flexion deformities.
- Spinal supports for people with a flail spine help to support the back.
Mobilization:
- Slowly mobilizing the patient in the essence of progressing from support in bed, to support in a chair, from sitting to standing and walking.
- Continuous mobilization of the paralyzed person out of bed, from a wheelchair utilized in too many disabled patients to a walking machine, parallel bars, crutches, and calipers are utilized in less severely disabled patients.
- Individuals with weak knee extensors are capable of walking without any type of calipers by supporting the knee with a hand or by forcing back their knee.
- This can be performed in persons with strong hip extensors and moderate plantar.
Strength Training:
- Be in charge of a progressive resistance training regime with voluntary contractions and rest intervals are given to permit recovery from fatigue.
- To safeguard against the possible risk of overuse, the first training load is less and eventually improved gradually.
- Usual warm-up exercises are done by low-resistance, high-repetition exercises for all greater muscle groups, both for the upper extremities, lower extremities, and also the trunk.
- More importance is laid on training the quadriceps muscle.
Cardiovascular Fitness Exercises:
- A perfect level of exercise must be suggested to gain maximal cardiovascular fitness without worsening levels of chronic fatigue.
- Too much cardiovascular exercise has proved to improve levels of chronic fatigue, though some amount of exercise is important for improving cardiovascular fitness.
- Therefore a moderate intensity, short session, often rests with adequate recovery time between session days is preferred.
Stretching of Muscles and Joints:
- Stretching of Muscles and Joints helps in the reduction of contractures.
- Joints must be stretched perfectly in the direction opposite to that of the contracture and should be performed once a day at least three times.
- For flexion contracture of the hip, backward pressure should be applied in the upper 3rd of the thigh, the other hip must be totally flexed to reduce lumbar lordosis, and the leg is taken down in normal adduction to stretch out the abductors which are usually tight.
- The patient is lye on his face in bed, with a pillow underneath the lower thigh.
- The hips may also be extended while the person is in this position.
- Flexion contracture of the Knee is manipulated by exerting pressure around the joint.
Manipulation of Ankle and Foot Deformities:
- The most crucial deformity to correct is equinus.
- The ankle is normally supported as the foot is dorsiflexed, in the case of varus of the foot or adduction of the forefoot then it is important to be firm but slow and not do too forceful manipulation.
- Firm pressure for 5 to 7 minutes in the other direction to the deformity, and is repeated and followed by a surgical correction to prevent a recurrence.
Orthosis:

- Children with weak limbs and with the possibility of deformity are motivated to wear calipers till the growth period is completed.
- They may walk without any kind of support but the caliper must fit properly.
Crutches:

- Crutches are needed in patients with bilateral calipers or a caliper on 1 leg with weakness of the opposite leg or spine, also required in patients with weakness of the hip on the side with a severely involved lower leg.
- Crutches must be correct both in length and in the position of the handgrip.
- In case of weakness of the trunk or arms, the top of the crutch should be perfectly padded to avoid any kind of pressure in the axilla and radial nerve palsy.
Hydrotherapy:

- Training sessions may be held in the hydrotherapy pool, designed to train general physical fitness involving resistance and endurance activities, balance, stretching, and relaxation.
- The patient exercises at the intensity level where muscle fatigue is not present at the time of or after the training session.
Aerobic training:
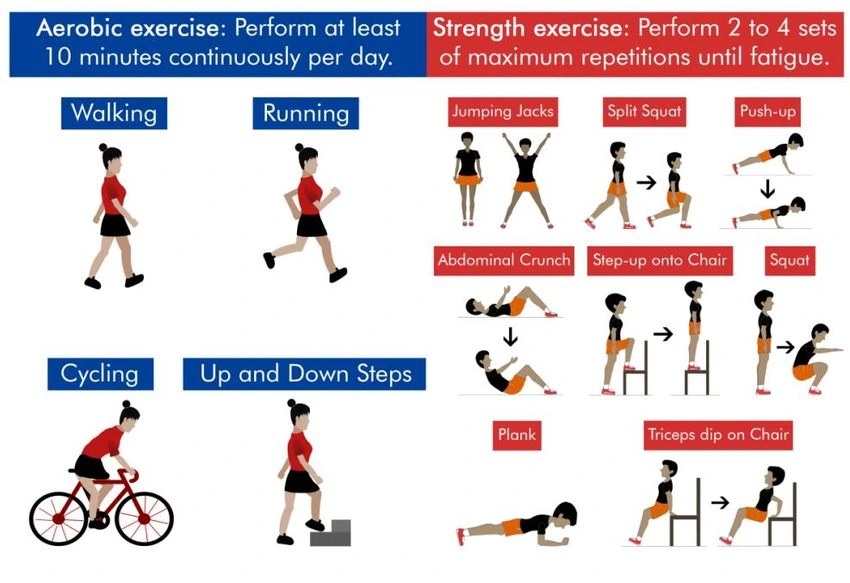
- The patient exercises at seventy percent of maximal heart rate in an aerobic exercise program are ruled to be beneficial.
- For example, training on the treadmill three times a week for twenty minutes per session in an aerobic exercise program.
- The patient should follow these exercises on daily basis or as suggested by the physiotherapist.
- There is no specific cure for poliomyelitis, as it has paralyzed thousands of individuals all over the world.
- Thus treatment mainly focuses is on improving comfort, speeding recovery, and preventing complications.
Polio Prevention
- There is no particular cure for polio, but a vaccine allows the body to fight off the virus.
- Before the vaccine became available in the 1950s, the virus paralyzed thousands of individuals each year.
- By the 1970s, because many individuals had the vaccine, there were fewer than ten cases of polio in the U.S.
There are two types of the vaccine:
- Inactivated poliovirus vaccine (IPV). A person gets this as a shot in either the leg or the arm.
- Oral poliovirus vaccine (OPV). This is an older form of the vaccine that is still used around the world.
Today, kids frequently get doses of the IPV vaccine, 1 dose each at ages:
- 2 months
- 4 months
- Between 6 and 18 months
- Between 4 and 6 years
FAQ
The word poliomyelitis arrives from the Greek word “polio” meaning “grey” and “myelon” meaning “marrow.” It is an infectious disease caused by the poliovirus, a part of the genus Enterovirus, belonging to the Picornaviridae family.
No, there is no cure for polio. The Polio vaccine is a great route to protect against polio. Safe and effective vaccines available: the oral polio vaccine (OPV) and the inactivated polio vaccine (IPV), are the only vaccine utilized in the United States since 2000.
Polio ( medically known as poliomyelitis) is a serious disease caused by infection with any of the three strains of poliovirus. The virus is live for six weeks. It is spread through water, food, or hands contaminated with the feces (poo) or throat secretions of someone who is infected with the virus.
A polio infection frequently damages or destroys many of these motor neurons. Because there are some motor neurons, the remaining neurons sprout new fibers and grow bigger. This promotes recovery of the use of the muscles, but it also can stress the nerve cell body to nourish the additional fibers.
Sometimes poliovirus is spread via saliva from an infected person or droplets expelled when an infected person sneezes or coughs. Individuals become infected when they inhale airborne droplets or touch something contaminated with the infected saliva or droplets.





One Comment