Parsonage-Turner syndrome:
Table of Contents
Overview:
Parsonage-Turner syndrome (PTS) is a neurological disorder. It is characterized by the rapid onset of severe pain in the upper extremity. This syndrome’s acute phase is for a few hours to a few weeks and muscle wasting and weakness (amyotrophy) are present in the affected areas. This involves mostly the brachial plexus, the bunch of nerves that extend from the spine through the neck, into the armpit, and down the arms. These nerves control movements and sensations of the upper limb.
The exact cause of this syndrome is unknown, but it is may be caused by an abnormality of the immune system (immune-mediated disorder). The severity of the disorder can widely from one individual to another, in part of the specific nerves involved. Affected individuals may recover without treatment. However, individuals may experience recurrent episodes. Some patients may experience residual pain and significant disability.
In the Parsonage-Turner syndrome injury that comes from sports (trauma), the weakness and pain normally last for a few minutes or hours. If its duration is too long, the injury may get more serious.
What is Parsonage-Turner syndrome?
Parsonage-Turner syndrome is also known as brachial neuritis. This is a neurological condition that causes sudden and severe pain in the upper extremity. Parsonage-Turner syndrome (PTS), also known as brachial plexopathy or neuralgic amyotrophy, is a disorder that defines an inflamed nerve involving the brachial plexus. It may present with symptoms of a peripheral nerve lesion. It is a rare condition that generally involves one upper limb, most commonly affecting the axillary nerve, the upper trunk of the brachial plexus, the suprascapular nerve, and the long thoracic nerve. Weakness is present in the upper limb muscle and the pain is from days to a few weeks.
1.6 out of 100,000 people are affected by this syndrome every year. Parsonage-Turner syndrome is mostly misdiagnosed as a cervical condition like; radiculopathy or cervical spondylosis.
Parsonage-Turner syndrome is also known as:
- Brachial neuritis.
- Brachial plexus neuritis.
- Brachial plexus neuropathy.
- Idiopathic brachial plexus neuropathy.
- Neuralgic amyotrophy.
- PTS.
What is the brachial plexus?
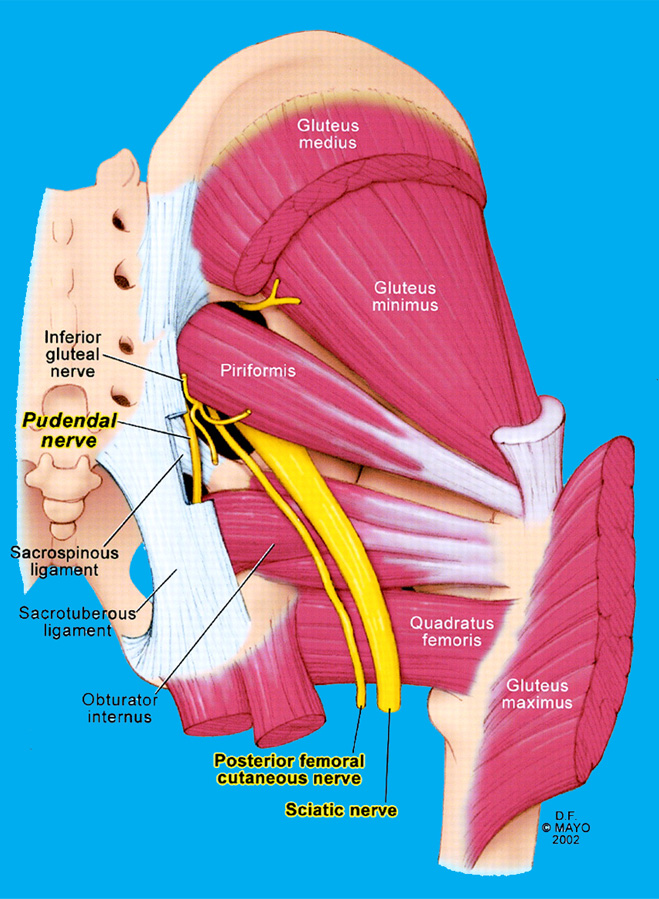
The brachial plexus is a complex of nerves. It starts at the spinal cord and extends down the side of the neck behind the clavicle bone to the axilla. It controls movement in the whole upper limb and also carries sensation from the arm to the spinal cord. this network is formed by the lower four cervical nerve roots C5-C8 and the first thoracic nerve root T1.
The affected population of the PTS:
In this syndrome, males are more affected rather than females and the ratio is 3:2. The incidence of this syndrome is based upon available population studies, and it’s approximately 1.64 to 3.00 people per every 1,00,000 individuals in the population per year.
The condition of neuralgic amyotrophy is seen in 2-3 per 100,000 persons every year. There does not see the prevalence of hand dominance. generally, the left arm is more affected compared to the right arm.
Mechanism of the PTS:
This condition affects the suprascapular nerve in 97% of cases and also involves the axillary and subscapular nerves. As the supraspinatus and infraspinatus muscles are involved, which are supplied by the suprascapular nerve. The affection of the deltoid muscle is more different as it is supplied by the axillary nerve.
Causes of the Parsonage turner syndrome:
The causes of this syndrome are undiagnosed, it is present in various clinical conditions like, post-operatively, post-infectiously, post-traumatically, and post-vaccination conditions.
The condition is often in young to middle-aged adults, but it has been reported mostly in young children and elderly people. This syndrome may be hereditary.
The following causes trigger the condition:
- Any type of infection. Mainly 25% of people had infections before they got Parsonage-Turner syndrome.
- Vaccinations. Mainly in 15% of cases syndrome occurred after vaccination.
- Trauma. A motorcycle accident or a football injury can cause trauma to the shoulder.
- Cancerous cells
- Immunizations or a defective immune system. Immune-mediated inflammatory response to an infection or environmental cause that harmed brachial plexus nerves.
- Lumbar puncture.
- recurrent surgery, childbirth, or radiation treatment.
- Parasitic infection.
- Rheumatologic disorders and autoimmune disorders.
- Drugs use, like heroin.
- Polyarteritis nodosa or temporal arteritis.
A person who is genetically or hereditary predisposed to a disorder carries a gene (or genes) for the disease, but it may not be triggered or “activated” under a certain environment.
How does Parsonage-Turner syndrome develop?
In most cases, the pain starts suddenly, at the midnight, in the shoulder or arm. It’s sharp shooting-like pain. The pain can present for hours up to four weeks. The muscles of the arm on the affected side will get weaken within 24 hours of when the pain started.
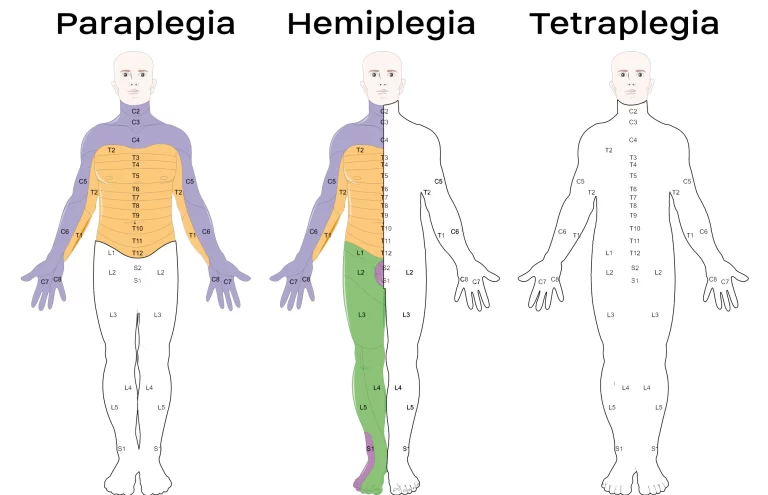
Weakness is present in the whole upper extremity, and sometimes chest wall muscles or the diaphragm can also be affected. Rarely, often the leg and cranial (head) muscles are also involved. When the muscles get weak, muscle tissue can be lost over time and it is called atrophy.
What are the symptoms of Parsonage-Turner syndrome?
Every people are different, the severity of pain, location of pain, duration of pain, and weakness won’t be the same. Symptoms of Parsonage-Turner syndrome may following:
- Pain is present in the neck, shoulder, arm, and hand. it is a sharp, aching, burning, stabbing, or throbbing type of pain. The Pain duration is remain 1 to 2 weeks but in rare condition it can seen for longer periods of time. Pain is worse in the evening or during the night.
- Muscle weakness in the shoulder. It may be mild, severe, or almost paralyzing.
- Reflexes are altered.
- Loss of sensation or numbness. Feeling tickling, prickling, or burning.
- Partial dislocation of the shoulder joint.
- Shortening of the muscles or tendons.
- Shortness of breath or excessive sweating.
- Red, purple, or spotted hands, swelling.
- Sensory deficits in rare cases.
- Scapular winging may be seen when there is the involvement of the scapulothoracic nerve supplying the serratus anterior muscle.
Phases of Parsonage turner syndrome:
There are two phases of Parsonage-Turner syndrome. The first phase is the acute phase. In this, the pain is most severe. The pain is reduced in the second period, known as the chronic phase. In some cases, Parsonage-Turner syndrome is caused by genetic factors (hereditary neuralgic amyotrophy).
Differential diagnosis of the parsonage Turner syndrome?
The pain is present around the shoulder girdle. It can present similarly to other shoulder problems, like:
- Rotator cuff tears
- Adhesive capsulitis
- Calcific tendonitis
- Arthritis.
Weakness of distal muscles of the shoulder can also present similar to other shoulder conditions, like:
- Discogenic nerve root compression
- Tumors of the spinal cord
- Thoracic outlet syndrome (TOS)
- Cervical artery dissection.
Differential diagnosis on MRI findings includes:
- Disuse atrophy of shoulder girdle muscles
- Quadrilateral space syndrome
- Trauma.
- Idiopathic hypertrophic brachial neuritis.
Examination of the PTS:
First, dr takes the whole history of the patient.
Phase I: Patient having a sudden onset of severe, unrelenting shoulder pain:
- The primary symptom in 90% of cases
- The pain extends to the proximal arm and neck.
- Awakens people from sleep
- It present lasts days to weeks.
- Seen commonly in males (45 days vs. 23 days in females).
Phase II: painless flaccid paralysis phase:
- After the onset of pain, a weakness of muscle begins within 24 hours (33%) to 4 weeks (80%).
- most commonly involves the upper brachial plexus and usually, more than one nerve branch deltoid, supraspinatus, infraspinatus, serratus anterior and the biceps brachii muscles include.
Phase III: slow recovery
- Slow and steady return of motor function or normal movement over 6-18 months
- It directly depends on the duration of the pain phase at the onset of the disease.
Physical examination:
The doctor will observe symptoms. They will check the muscle strength, muscle reflexes, and sensation in your arm.
- Muscle bulk/tone: See the atrophy of supraspinatus, infraspinatus, deltoid, biceps, trapezius, serratus anterior, pronator teres, and teres minor muscles.
- Muscle strength:
- Present the weakness of supraspinatus, infraspinatus, biceps, brachioradialis, pronator teres, trapezius, serratus anterior, pronator teres, and teres minor muscles.
- Another muscle strength is normal like rhomboids, triceps, wrist, and hand muscles.
- Sensation: Numbness present over the lateral arm, forearm, and anatomic snuffbox
- Reflexes: Biceps and brachioradialis muscle reflexes are absent.
- Trophic skin changes.
- Temperature dysregulation.
- Increased sweating.
- Altered nail/hair growth.
- Winging of the scapula is also present.
After the physical examination, dr will check the other special test to rule out the confirmed diagnosis:
Special test or Radiological examination:
EMG test:
- If the dr thinks the patient has Parsonage-Turner syndrome, they advise the EMG test:
- This test consists of two parts:
- In the first part, nerves are shocked in a controlled manner, and responses are measured.
- In the second part, small needles are inserted in various muscles of the arm to check the electrical activity of particular muscles at rest and during movement. The EMG can help check the exact nerve location, nature, and severity of nerve damage.
- This test takes one to two hours.
MRI test:
An MRI can be used to rule out other possible causes of shoulder pain, show atrophy of affected muscles, and investigate signal alterations caused by a loss of nerve supply (denervation).
Nerve conduction velocity (NCV test):
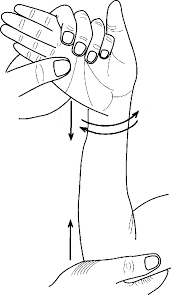
Nerve conduction studies check the ability of specific nerves in the peripheral nervous system to relay nerve impulses to the brain. Electrodes are put over specific nerves, such as those in the shoulders and arms, during a nerve conduction examination. This stimulates the nerves and records the conduction of the signal. This test can help to rule out the site of disease or injury to the nerve.
X-ray :
An x-ray (radiograph) of the shoulder may rule out damage or breaking the shoulder in specific conditions.
Treatment of Parsonage turner syndrome:
Medical treatment:
- The doctor has given the painkillers to reduce the pain. The pain is worse when the problem starts.
- Pain-relieving drugs such as tricyclic antidepressants, duloxetine, or gabapentin may be used.
- Steroid medications such as prednisone may be advised in the early phase.
- Physicians are given oral corticosteroids such as prednisone in the acute phase, which has reduced the duration of pain and initiated the healing process in some cases.
After that doctor suggests to the patient do physical and occupational therapy for three to eight weeks. It can help to achieve the full range of motion and increase strength.
TENS (transcutaneous electrical nerve stimulation) modality may help to decrease the pain.
Surgical treatment:
Surgical treatment is considered after conservative treatments fail. In this nerve grafting, tendon transfer or neurolysis surgery was done.
Nerve grafting:
In nerve grafting surgery the surgeon takes a small part of nerve tissue from another part of the body and uses it to repair injured nerves. This surgery is done within 12 months of injury.
Tendon transfer:
Tendon transfer surgery is necessary when muscle function is lost because of nerve injury.
In tendon transfer surgery a normal tendon is removed from another part of the body to replace an injured tendon.
These both surgeries restore the muscles and joint functions.
Neurolysis:
- long thoracic nerve micro neurolysis
- ulnar nerve transposition, Guyon canal release
- radial tunnel release
- carpal tunnel release
Physiotherapy treatment for Parsonage-Turner Syndrome:
Physical therapy treatment plays an important role in this condition. In physical therapy treatment, the therapist focuses on patient education, upper-extremity Range Of Motion, strengthening exercises to maintain periscapular movement, and given the modalities for pain relief.
Modalities for pain relief like TENS.
The recovery period depends on the patient’s muscle weakness and activity.
Active and passive exercise:
Active and passive range of motion exercises helps to prevent muscle atrophy and contractures.
The Range of motion exercises helps to improve the patient’s shoulder and hand activity. It is important in starting stage depending on the involved muscle weakness.
Strengthening exercise:
Strengthening exercises are important after the patient does the limb activity without any support or assistance. Once the whole range of motion of the particular limb achieves the therapist goes for the strengthening exercise.
It is done with the use of a weight cuff, resistance belt, or theraband. Strengthening exercises are not used during the acute phase because they increase pain.
Electrical stimulation:
The electrical stimulation (ES) is considered when the denervated muscle is prolonged, i.e., greater than 4 months. It is useful for restoring the normal properties of the denervated muscles if the correct stimulation pattern is selected. ES starts in optimal time as soon as possible after muscle nerve injury.
Pain relieving modalities:
Heat or cold and transcutaneous electrical nerve stimulation (TENS) use the reducing the pain. In this procedure, the electrical impulses are sent through the skin to help to control pain by blocking nerve transmissions or pain sensations.
Generally, therapists recommend intensive exercise therapy to stimulate nerve function and restore muscle activity. Normally, people do exercises to achieve movement of the shoulder and arm. After that, strengthening exercises help to restore muscle bulk.
Prognosis of PTS:
The prognosis for PTS is different. According to old medical reports, persons who are most affected will recover up to 70-90% of their normal strength and functional level.
There is approximately a 5-26% risk that PTS patients will recover after initial recovery or being effectively treated. 35% of patients have recovered in 1 year. 90% of patients have fully recovered in 3 years. The patient had full muscle strength and function with no residual pain.
Most people (70% to 90%) have a good recovery of strength and arm use over two to three years. Occupational therapy may help patients return to their work.
FAQ:
What is the cause of Parsonage-Turner syndrome?
The Brachial plexus nerves control movements and sensations in the whole upper limb and lower limb. The exact cause of Parsonage-Turner syndrome is not known, but it is occurs mostly due to an abnormality of the immune system.
What are the symptoms of nerve damage in the shoulder?
The main symptoms of nerve damage are the following:
Sharp, shooting pain in the shoulder, arm, and/or hand.
Numbness, tingling sensation, anywhere along the shoulder or arm but most commonly in the outer, rounded part of the shoulder.
Weakness in the shoulder or upper arm (i.e., you can’t move your arm).What is the treatment for Parsonage-Turner?
The medical treatment for this condition is to take a painkiller to reduce the pain. Then other treatments are physiotherapy and occupational therapy to achieve the functional activity.
Physical therapy can relieve pain in muscles and joints. Apply the hot and cold packs, and a TENS machine, which sends electrical impulses to the muscle, can help. For longer-lasting pain. Active and passive exercise to achieve the range of motion for affected joints. Strengthening exercise to improve the strength of the affected muscles.
If the condition is worse, surgery of the nerve is required.What age does Parsonage-Turner Syndrome occur?
Patients affected by this condition range from 3 months of age to 75 years. However, the highest incidence of this condition seen in individuals between the 30th to 70th ge group.
What are the three symptoms of Turner?
Features of Turner syndrome may include a short neck with a webbed appearance, a low hairline at the back of the neck, low-set ears, hands, and feet that are swollen or puffy at birth, and soft nails that turn upward.
Girls’s symptoms progress more gradually than other male children.