The Brachial Plexus
Table of Contents
What is Brachial Plexus?
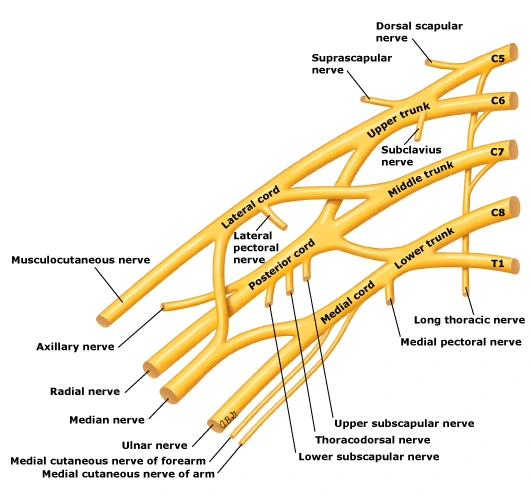
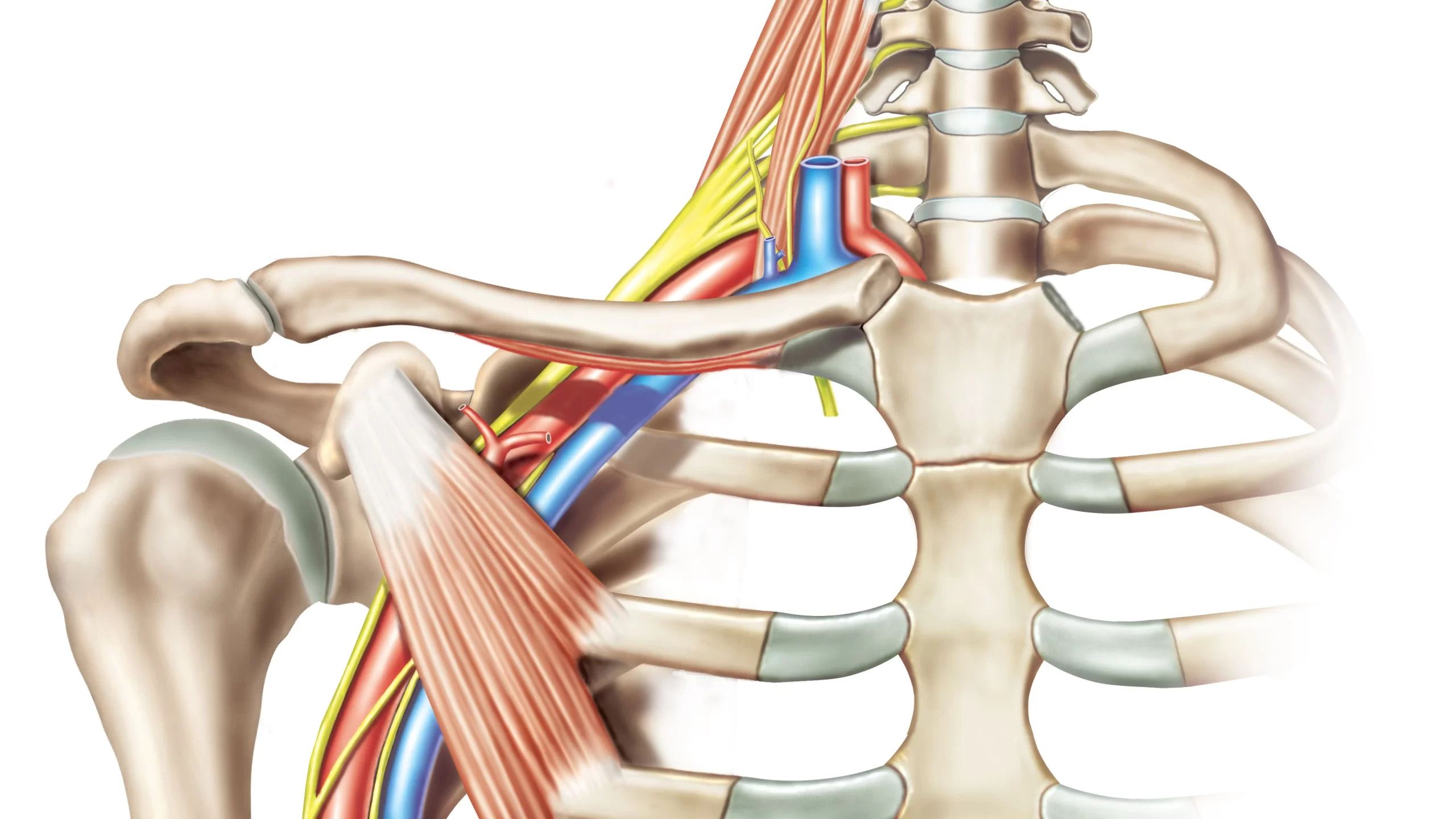
The Brachial Plexus could be a network of nerves that offers rise to all or any of the motor and sensory nerves of the upper extremity. It rises from the anterior rami of spinal nerves C5-T1 that sustain various combinations and splits into trunks and divisions until they finally create their terminal branches. These terminal branches are responsible for sensory and motor innervation of the upper limb, and they include the musculocutaneous, axillary, radial, median, and ulnar nerves.
Additionally, to terminal branches, the nerve plexus gives rise to many preterminal branches called supraclavicular branches, which leave the plexus at various points along its length.
Anatomy
The Brachial plexus originates from the anterior rami of spinal nerves C5-T1, which form the roots of the brachial plexus. The roots quickly merge to make trunks, which subsequently split into divisions. Finally, the divisions combine into cords of the brachial plexus, that give off the terminus branches of the brachial plexus.
Apart from the terminal branches of the plexus brachialis, various nerves branch far away from the former parts of the plexus. These ‘preterminal branches’ originate from the trunks and roots and are mutually called the supraclavicular branches of the plexus brachialis. The cords themselves are called the infraclavicular branches of the plexus brachialis, while the nerves that branch far from the cords are the terminal branches of the brachial plexus.
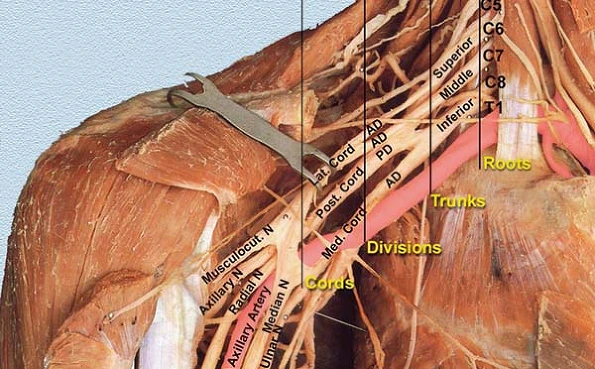
Roots
The ‘roots’ reference the anterior rami of the spinal nerves that include the brachial plexus. These are the anterior rami of spinal nerves C5, C6, C7, C8, and T1.
At each vertebral level, paired spinal nerves arise. They move the funiculus via the intervertebral foramina of the back. Each nerve then divides into two parts an anterior and a posterior ramus. The roots of the plexus brachialis are formed by the anterior rami of spinal nerves C5-T1 (the posterior divisions innervate the skin and musculature of the intrinsic back muscles).
After their formation, these nerves pass between the anterior and medial scalene muscles to enter the bottom of the neck.
Trunks
Each trunk contains a well-known scheme of origin from the roots of the brachial plexus:
- The superior trunk is created by the roots of C5 and C6.
- The middle trunk is created from the basis of C7 only.
- The inferior trunk is created by the roots of C8 and T1.
How to easily remember this: imagine that your fingers are the five anterior branches (C5-T1), where C5 is the thumb and T1 is the finger. once you connect the thumb (C5) with the index (C6), you get the superior trunk. the center finger (C7) stands alone and forms the center trunk, while the annualry (C8) and also the finger (T1) connect to form the inferior trunk.
Upon their origin, the trunks miss the bottom of the posterior triangle of the neck, traveling between the anterior and middle scalene muscles and behind the arteria. The trunks then cross over the apex of the lung and therefore the first rib and course towards the clavicle.
In this segment of the nerve plexus, the superior trunk gives rise to a different number of supraclavicular branches: the suprascapular nerve and therefore the subclavian nerve (nerve to subclavius).
Divisions
As they reach the posterior aspect of the center third of the clavicle, each of the three trunks divides into an anterior and posterior division. This yields a complete 6 divisions (3 anterior and three posteriors), which still pass inferiorly behind the clavicle to enter the axillary region.
The divisions don’t produce to any branches. Instead, they are going on to merge with each other to create the following segment of the brachial plexus: the cords.
Cords
The cords of the brachial plexus are formed by the three anterior and three posterior divisions that merge in a very specific way:
- The lateral cord is created by the merger of the anterior division of the superior trunk and the anterior division of the center trunk.
- The medial cord may be a direct continuation of the anterior division of the inferior trunk.
- The posterior cord is made by the merger of the posterior divisions of all three trunks.
- The cords are located around and called after their relationship with the second part of the arterial blood vessel. It’s easy to remember that the lateral cord is placed laterally, the medial cord lies medially, and Thus, the posterior cord lies posterior to the artery.
The lateral and medial cords innervate the muscles of the anterior (flexor) section of the forearm, whereas the posterior cord innervates the muscles of the posterior (extensor) compartment of the forearm.
Each cord provides one or more preterminal branches:
- The lateral cord provides arise to the lateral pectoral nerve.
- The posterior cord provides rise to the upper subscapular nerve, thoracodorsal nerve, and lower subscapular nerve.
- The medial cord provides rise to the medial pectoral nerve, the medial cutaneous nerve of the arm, and the medial cutaneous nerve of the forearm.
The cords terminate on the area of the inferior margin of the pecs muscle, by prolonging into their respective terminal branches:
- The lateral cord expands into the musculocutaneous nerve and therefore the lateral root of the median nerve.
- The posterior cord extends into the nervus radialis and axillary nerve.
- The medial cord extends into the cubital nerve and also the medial root of the median nerve.
Branches
Supraclavicular branches
Dorsal scapular nerve
The dorsal scapular nerve most frequently rises directly from the root of the C5 spinal nerve. sometimes, it can rise from the superior trunk of the brachial plexus. The dorsal scapular nerve gives a motor reaction to the levator scapulae, rhomboid major, and rhomboid minor muscles.
Suprascapular nerve
The suprascapular nerve appears from the superior trunk and bears fibers of the C5 and C6. The suprascapular nerve gives sensory innervation to the glenohumeral and acromioclavicular joints, and motor innervation to the supraspinatus and infraspinatus muscles.
Long thoracic nerve
The long thoracic nerve arises from the combination of the roots of C5, C6, and C7. This nerve gives motor innervation to the serratus anterior muscle.
Subclavian nerve
This nerve arises from the superior trunk of the brachial plexus and contains fibers of C5 and C6 spinal nerves. The subclavian nerve gives motor innervation to the subclavius muscle.
Branches of the lateral cord
The lateral cord provides arise to a couple of preterminal branches; the lateral pectoral nerve and the lateral root of the median nerve. It also provides one of the terminal branches of the brachial plexus, the musculocutaneous nerve.
Lateral pectoral nerves
The lateral pectoral nerves rise from the lateral cord of the brachial plexus and bring fibers of C5, C6, and C7 spinal nerves. Through the anastomotic with the medial pectoral nerves, the lateral nerves participate in the innervation of the pectoralis minor muscle.
The lateral root of the median nerve
This is a small branch that is one of the two roots of the median nerve. It directly combines with the medial root, a branch of the medial cord, to form the median nerve.
Musculocutaneous nerve
The musculocutaneous nerve is a terminal branch of the lateral cord of the brachial plexus, bringing fibers of C5-C7 spinal nerves. It is a mixed nerve that gives both motor and sensory supplies to the upper limb.
The motor fibers of the musculocutaneous nerve innervate the muscles of the anterior arm, specifically the biceps brachii, coracobrachialis, and brachialis muscle. The sensory fibers of the musculocutaneous nerve innervate the skin over the lateral surface of the forearm through the lateral cutaneous nerve of the forearm.
Branches of the medial cord
The medial cord provides the medial pectoral nerve, medial brachial cutaneous nerve, medial antebrachial cutaneous nerve, the medial root of the median nerve, as well as the ulnar nerve (another terminal branch of the brachial plexus).
Medial pectoral nerves
The medial pectoral nerves rise from the medial cord of the brachial plexus, including fibers of C8 and T1 spinal nerves. This nerve gives motor innervation to the pectoralis minor muscle and the lower sternocostal part of the pectoralis major muscle.
Medial brachial cutaneous nerve
The medial brachial cutaneous nerve, also termed the medial cutaneous nerve of the arm, rises from the medial cord and brings fibers of C8 and T1 spinal nerves. This nerve gives sensory innervation to the skin of the inferior portion of the medial side of the arm.
Medial antebrachial cutaneous nerve
The medial antebrachial cutaneous nerve, also termed the medial cutaneous nerve of the forearm, arises from the medial cord bringing fibers of the T1 spinal nerve. This nerve gives sensory innervation to the skin of the arm overlying the biceps brachii, and the skin of the medial side of the forearm.
The medial root of the median nerve
The medial root of the median nerve is the second cause of the median nerve. It combines with the above-mentioned lateral root to form the trunk of the median nerve.
Ulnar nerve
The ulnar nerve is a terminal branch of the medial cord of the brachial plexus that includes fibers of C8 and T1 spinal nerves. equally to the median nerve, the ulnar nerve is a combined nerve that supplies motor and sensory innervation to the forearm and hand.
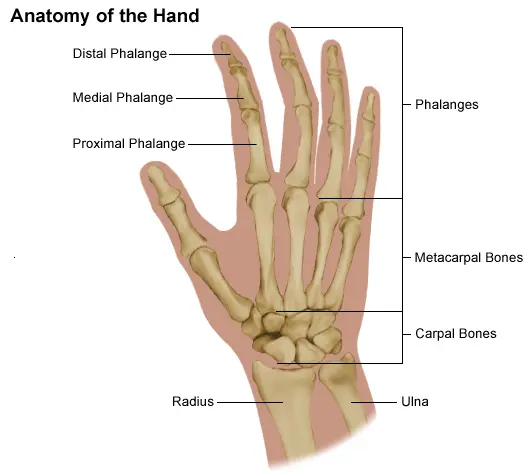
The ulnar nerves give motor supply to the following:
The unused muscles of the forearm are not delivered by the median nerve (flexor carpi ulnaris muscle, medial ½ of the flexor digitorum profundus).
All intrinsic muscles of the hand, excluding the LOAF muscles (lateral two lumbricals, opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis).
The nervus ulnaris gives sensory supply to the following:
The anterior and posterior aspects of the medial 1½ fingers on skin.
The anterior and posterior aspects of the medial ½ of the palm on the skin.
The ulnar nerve delivered the HILA muscles of the hand:
- Adductor pollicis
- Medial two Lumbricals
- Hypothenar muscles like abductor digiti minimi, flexor digiti minimi brevis, and opponens digiti minimi
- Interossei muscles such as dorsal and palmar interossei
Branches of the posterior cord
The branch of the posterior cord of the brachial plexus gives rise to the thoracodorsal and axillary nerves, subscapular, and further the musculospiral nerve.
Subscapular nerves
There are typically two of those nerves: the superior and inferior subscapular nerves. Both of these nerves arise from the posterior cord bringing the fibers of C5 nervus. The superior subscapular nerve innervates the superior part of the subscapularis muscle, though the inferior subscapular nerve innervates the remains of the subscapularis muscle, because the teres major muscle.
Thoracodorsal nerve
The thoracodorsal nerve rises from the posterior cord of the brachial plexus and produces the fibers of C7 and C8. This nerve gives motor innervation to the latissimus dorsi muscle.
Axillary nerve
The axillary nerve is the terminal branch of the posterior cord, bringing fibers of C5 and C7 spinal nerves. This nerve is a combined nerve that gives both sensory and motor innervation to the shoulder area. The axillary nerve supplies the teres and deltoid muscle, as well as the skin over the deltoid muscle.
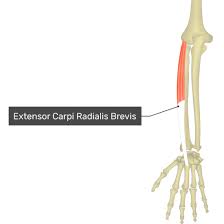
Radial nerve
The radial nerve is also the terminal branch of the posterior cord of the brachial plexus which includes fibers of spinal nerves C5-T1. This nerve is a combined nerve that gives sensory and motor innervation to the forearm and arm.
The radial nerve gives motor supply to the following:
All muscles of the posterior compartment of the forearm such as the anconeus, supinator, brachioradialis, extensor pollicis longus and brevis, extensor indices, extensor digiti minimi, abductor pollicis longus, extensor carpi radialis longus and brevis, extensor carpi ulnaris, extensor digitorum,
All muscles of the posterior compartment of the arm such as the triceps brachii muscle.
The radial nerve gives sensory supply to the following:
- The posterior surface of the arm on the skin.
- The central, posterior surface of the forearm on skin.
- The lateral surface of the dorsum of the hand on the skin.
- The posterior aspect of the lateral 2½ fingers on skin.
Median nerve
The median nerve originated from the combination of two roots which means it arises from the lateral and medial cord of the brachial plexus:
The medial root of the median nerve may be a terminal branch of the medial cord.
The lateral root of the median nerve could be a terminal branch of the lateral cord.
The median nerve courses over the whole upper limb and terminates within the hand by divided into its terminal branches. It is the combined nerve that provides sensory and motor innervation to many areas of the forearm and hand.
The median nerve gives motor supply to the following:
The anterior (flexor) compartment of the forearm’s all muscles except for the flexor carpi ulnaris and the medial ½ of the flexor digitorum profundus.
All thenar muscles such as abductor pollicis brevis, opponens pollicis, and flexor pollicis brevis, except for the adductor pollicis.
Two lateral lumbrical muscles.
The median nerve gives sensory supply to the following:
The lateral ½ of the palm of skin.
The posterior aspect of the lateral 2½ fingers of skin.
The anterior aspect of the lateral 3½ fingers of skin.
The median nerve delivered the LOAF muscles of the hand:
- Lateral two lumbricals
- Opponens pollicis
- Abductor pollicis brevis
- Flexor pollicis brevis
Clinical significance
Injury to the plexus brachialis may affect the sensation or movement of various parts of the arm. Injuries are often caused by the shoulder being pushed down and also the head being pulled up, which stretches or tears the nerves. Injuries related to malpositioning commonly affect the nerve plexus nerves, instead of other peripheral nerve groups. because the brachial plexus nerves are very sensitive to position, there are very limited ways of preventing such injuries. the foremost common victims of plexus brachialis injuries incorporate victims of automobile accidents and newborns.
Injuries are caused by stretching, diseases, and wounds to the lateral cervical region (posterior triangle) of the neck or the axilla. looking at the placement of the injury, the signs and symptoms can range from complete paralysis to anesthesia. Testing the patient’s ability to perform movements and comparing it to their normal side could be a method to assess the degree of paralysis. a standard nerve plexus injury is from a tough landing where the shoulder widely separates from the neck (such as in the case of bike accidents or falling from a tree). These stretches can cause ruptures to the superior portions of the nerve plexus or avulse the roots from the neural structure. Upper nerve plexus injuries are frequent in newborns when excessive stretching of the neck occurs during delivery. Studies have shown a relationship between a newborn’s weight and nerve plexus injuries; however, the quantity of cesarean deliveries necessary to stop one injury is high at most birth weights.
For the upper brachial plexus injuries, paralysis occurs in those muscles supplied by C5 and C6 just like the deltoid, biceps, brachialis, and brachioradialis. A loss of sensation within the lateral aspect of the upper limb is additionally common with such injuries. An inferior nerve plexus injury is much less common but can occur when someone grasps something to interrupt a fall or a baby’s upper limb is pulled excessively during delivery. during this case, the short muscles of the hand would be affected and cause the shortcoming to create a full fist position.
To differentiate between preganglionic and postganglionic injury, the clinical examination requires that the physician keep the subsequent points in mind. Preganglionic injuries cause loss of sensation above the extent of the clavicle, pain in an otherwise insensate hand, ipsilateral Horner’s syndrome, and loss of function of muscles supplied by branches arising directly from roots—i.e., long nervus spinalis palsy resulting in winging of scapula and elevation of ipsilateral diaphragm because of nervus phrenicus palsy.
Acute brachial plexus neuritis may be a disorder that’s characterized by the onset of severe pain within the shoulder region.
Sports injuries
One sports injury that’s becoming prevalent involved sports, particularly within the sport of Yankee football, is named a “stinger.” An athlete can incur this injury in an exceeding collision which will cause cervical axial compression, flexion, or extension of nerve roots or terminal branches of the brachial plexus. in an exceedingly study conducted on football players at our academy, researchers found that the foremost common mechanism of injury is, “the compression of the fixed plexus brachialis between the protective garment and therefore the superior medial scapula when the pad is pushed into the realm of Erb’s point, where the nerve plexus is most superficial.”. The results of this is often a “burning” or “stinging” pain that radiates from the region of the neck to the fingertips. Although this injury causes only a short-lived sensation, in some cases it can cause chronic symptoms.
Penetrating wounds
Most penetration wounds require immediate treatment and aren’t as easy to repair. for instance, a deep knife wound to the plexus brachialis could damage and/or sever the nerve. in step with where the cut was made, it could inhibit action potentials needed to innervate that nerve’s specific muscle or muscles.
Injuries during birth
Brachial plexus injuries can occur during the delivery of newborns when after the delivery of the pinnacle, the anterior shoulder of the infant cannot pass below the pubic symphysis without manipulation. This manipulation can cause the baby’s shoulder to stretch, which might damage the plexus brachialis to varying degrees. this sort of injury is observed as shoulder dystocia. Shoulder dystocia can cause obstetric brachial plexus palsy (OBPP), which is the actual injury to the brachial plexus. Nerve damage has been connected to birth weight with larger newborns being more vulnerable to the injury but it also has got to do with the delivery methods. Although very hard to forestall during nascency, doctors must be ready to deliver a newborn with precise and delicate movements to decrease the chances of injuring the kid.
Tumors
Tumors that will occur within the brachial plexus are schwannomas, neurofibromas, and malignant peripheral nerve sheath tumors.
Imaging
Imaging of the brachial plexus is often done effectively by employing a higher magnetic strength MRI Scanner. it’s impossible to gauge the brachial plexuses with plain Xray, CT and ultrasound scanning can manage to look at the plexuses to an extent; hence MRI has preferred in imaging nerve plexus over other imaging modalities thanks to its multiplanar capability, and therefore the tissue contrast difference between brachial plexus and adjacent vessels. The plexuses are best imaged in coronal and sagittal planes, but axial images give a thought about the nerve roots. Generally, T1 WI and T2 WI images are utilized in various planes for imaging; but new sequences like MR Myelolography, Fiesta 3D, and T2 cube are utilized in addition to the essential sequences to assemble more information to gauge the anatomy.
Specific Branches
The branches are listed below. They primarily branch from the cords, but some originate from earlier structures.
| From | Nerve | Muscles | Cutaneous | Roots |
| roots | Dorsal scapular nerve | Rhomboid muscles and Levator scapulae | – | C4, C5 |
| roots | Long thoracic nerve | Serratus anterior | – | C5, C6, C7 |
| upper trunk | Nerve to the subclavius | Subclavius muscle | – | C5, C6 |
| upper trunk | Suprascapular nerve | Supraspinatus and Infraspinatus | – | C5, C6 |
| lateral cord | Lateral pectoral nerve | Pectoralis Major and Pectoralis Minor (by communicating with the Medial pectoral nerve) | – | C5, C6, C7 |
| lateral cord | Musculocutaneous nerve | Coracobrachialis, brachialis, and Biceps brachii | becomes the Lateral cutaneous nerve of the forearm | C5, C6, C7 |
| lateral cord | the lateral root of the median nerve | fibers to the median nerve | – | C6, C7 |
| posterior cord | Upper subscapular nerve | Subscapularis (upper part) | – | C5, C6 |
| posterior cord | Thoracodorsal nerve (middle subscapular nerve) | Latissimus dorsi | – | C6, C7, C8 |
| posterior cord | Lower subscapular nerve | subscapularis (lower part ) and Teres major | – | C5, C6 |
| posterior cord | Axillary Nerve | anterior branch: deltoid and a small area of overlying skin posterior branch: Teres minor and deltoid muscle | the posterior branch becomes the Upper lateral cutaneous nerve of the arm | C5, C6 |
| posterior cord | Radial Nerve | Triceps brachii, supinator, Anconeas, the extensor muscles of the forearm, brachioradialis | the skin of the posterior arm as the Posterior cutaneous nerve of the arm | C5, C6, C7, C8, T1 |
| medial cord | Medial pectoral nerve | Pectoralis Minor and Pectoralis Major | – | C8, T1 |
| medial cord | the medial root of the Median nerve | fibers to the median nerve | portions of hand not served by ulnar or radial | C6, C7 |
| medial cord | The medial cutaneous nerve of the arm | – | front and medial skin of the Arm | C8, T1 |
| medial cord | The medial cutaneous nerve of the forearm | – | medial skin of the forearm | C8, T1 |
| medial cord | Ulnar Nerve | Flexor carpi ulnaris, the medial two bellies of Flexor digitorum profundus, the intrinsic hand muscles except for the Thenar muscles and the two most lateral lumbricals | the skin of the medial side of the hand and medial one and a half fingers on the palmar side and medial two and a half fingers on the dorsal side | C8, T1 |
Clinical relations
Brachial plexus injury
Injuries to the plexus brachialis affect both motor and sensory functions within the upper limb. Different injuries, like inflammation, stretching, and wounds within the lateral cervical region of the neck or within the axilla may cause nerve plexus injuries, and also the manifestations rely upon the part of the plexus that’s affected. In any case, injuries to the plexus brachialis are followed by paralysis and anesthesia of the respective supply area of the affected nerves.
Median nerve injury
In the case of the median nerve involvement, the injury causes a palsy that ends up in a hand deformity called an ape hand. It is evident as an inability to abduct the thumb. In addition, it is attached by a loss of sensation in the lateral 3½ fingers.
Ulnar nerve injury
An injury of the ulnar nerve causes a hand deformity called the claw hand, which is a result of the paralysis of intrinsic muscles of the hand innervated by this nerve. The claw hand deformity is distinguished by hyperextended metacarpophalangeal joints and flexed interphalangeal joints.
Radial nerve injury
Radial nerve injuries cause a wrist drop, and all the posterior compartments of the forearm muscles become paralyzed which are supplied by the radial nerve.
FAQ
What are the 5 main roots of the brachial plexus?
The five roots are the five anterior primary rami of the spinal nerves after they need to give off their segmental supply to the muscles of the neck. The plexus brachialis emerges at five different levels: C5, C6, C7, C8, and T1.
Which is the largest branch of the brachial plexus?
The musculocutaneous nerve may be a terminal branch of the lateral cord of the plexus brachialis, carrying fibers of C5-C7 spinal nerves. it’s a mixed nerve that has both motor and sensory supplies to the upper limb.
What muscles does the nerve plexus pass?
The trunks of the nerve plexus pass between the anterior and middle scalene muscles. The ventral rami of C5 and C6 unite to create the upper trunk. The suprascapular nerve and also the nerve to the subclavius arise from the upper trunk.
Can plexus brachialis cause chest pain?
For most people, intense pain is the first symptom of brachial neuritis, and it can start within the shoulder or neck. The pain may radiate down the arms and into the hands or cause pain within the chest. In about two-thirds of cases, it affects only one side of the body.
Can nerve plexus cause neck pain?
It occurs when there’s damage to the nerve plexus. this is often a district on both sides of the neck where nerve roots from the neural structure split into each arm’s nerves. Damage to those nerves leads to pain, decreased movement, or decreased sensation within the arm and shoulder.
Can nerve plexus affect legs?
The nerve plexus on both sides includes the nerves that activate muscle movement and permit sensation (feeling) within the leg. A nerve plexus avulsion occurs when these nerves are completely torn. Sometimes the nerves are only damaged or stretched.

12 Comments