Phrenic Nerve
Table of Contents
What Is the Phrenic Nerve?
The phrenic nerve is a crucial component of the human nervous system, playing a vital role in facilitating respiration. It is one of the most important nerves in the body, originating from the cervical (neck) region of the spinal cord and providing motor and sensory innervation to the diaphragm, the primary muscle responsible for breathing.
The phrenic nerve is primarily composed of nerve fibers from the C3, C4, and C5 spinal nerve roots, which are collectively referred to as the “C3-C5 roots.” These nerve fibers merge together to form the phrenic nerve on the anterior (front) side of the scalenus anterior muscle in the neck. From there, the nerve travels inferiorly (downward) into the thoracic cavity.
The main function of the phrenic nerve is to control the diaphragm, a dome-shaped muscle that separates the chest (thoracic) cavity from the abdominal cavity. The contraction and relaxation of the diaphragm play a pivotal role in the process of breathing.
The right and left phrenic nerves are the two that you truly have. They both originate from the neck’s spinal nerves. They allow the diaphragm, which is the main breathing muscle, to move and feel. The right phrenic nerve controls the diaphragm’s right side, whereas the left phrenic nerve controls the diaphragm’s left side.
The phrenic nerve regulates your diaphragm, a large dome-shaped muscle located between your chest and abdomen. Breathing depends on it. Your nerve sends signals that force your diaphragm to contract, becoming thinner and flatter. This motion will give your lungs more room to expand and take in air. Following this, your lungs muscle(diaphragm) contract and you expel air when your diaphragm relaxes as a result of less phrenic nerve stimulation.
The act of breathing is unconscious. In most circumstances, you don’t need to consider or exert any control over it.
Where Is the Phrenic Nerve Located?
The third, fourth, and fifth spinal nerves’ nerve fibers come out of the spinal cord in the neck. The fourth cervical nerve, which is the main contributor, joins them to form the phrenic nerve in the neck.
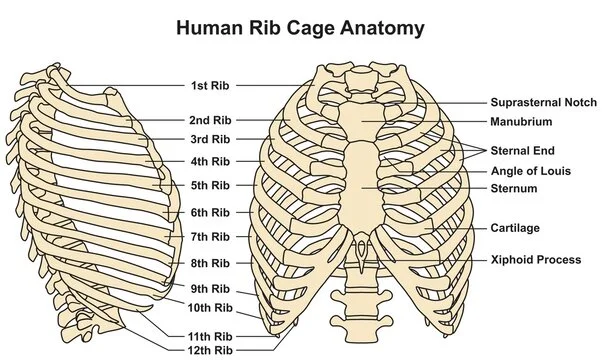
To get to the diaphragm, the newly created nerve must travel a considerable distance through the chest. The mediastinum, a chamber between the lungs that houses the heart, blood arteries, oesophagus (the food pipe), and other nerves, is where it goes through the chest.
When the phrenic nerves get there, they go via the diaphragm. From the bottom surface, they penetrate the muscle and innervate it.
Fortunately, respiration is unaffected by spinal cord damage to the lower neck or chest. This is due to the location high in the neck where the phrenic nerve exits the spinal cord.
Function:
The phrenic nerve plays a major role in your respiratory system’s ability to help you breathe. It is the sole nerve in your neural system that gives your diaphragm motor (movement) function. The impulses it transmits force your diaphragm to contract and expand. You can breathe in and out thanks to these motions.
It is frequently stimulated to contract by the phrenic nerve. It flattens as a result of this contraction, which decreases chest pressure. The lungs enlarge as a result, sucking air into them.
The pleura, which covers the lungs, and the diaphragm also send feelings through the phrenic nerves. They attach to the heart’s pericardium in a similar way. Disorders of the pericardium and pleura really generate pain in the shoulder and side of the neck because sensations from these structures are conveyed to the brain but misinterpreted as originating from the area supplied by the third, fourth, and fifth cervical nerves.
Additionally, your phrenic nerve conveys touch and pain sensory data to your:
- Diaphragm and the thin tissue that covers the top portion of your diaphragm, the diaphragmatic pleura.
- The mediastinal pleura is a thin layer of tissue that covers your chest between your lungs.
- The pericardium (sac that surrounds your heart).
- The thin tissue that protects the abdominal organs is called the peritoneum.
Anatomy of Phrenic Nerve
Origin:
The phrenic nerve, which in humans is primarily derived from the fourth cervical nerve, is also developed in part by the third and fifth cervical nerves (C3-C5). The phrenic nerve is therefore partially innervated by the cervical plexus and partially by the brachial plexus.
Course:
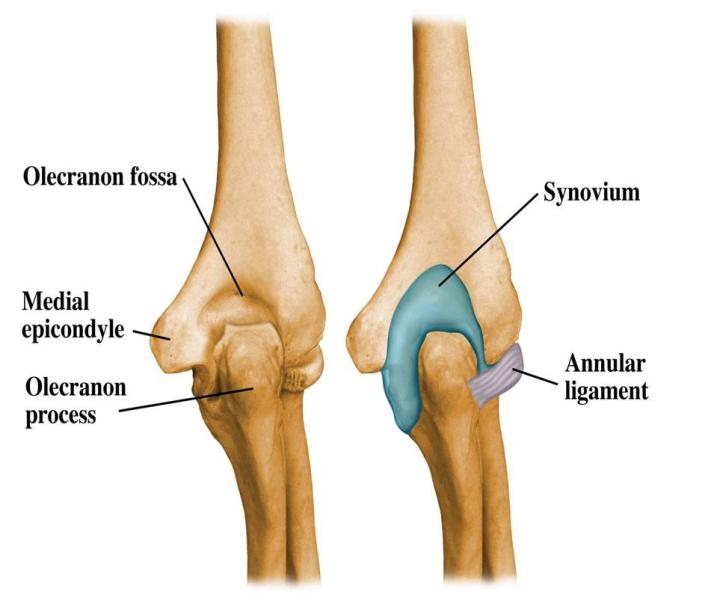
The phrenic nerve in the neck is located on the front of the anterior scalene muscle, crosses the pleura’s dome, and enters the thorax posterior to the subclavian vein.
The C3, C4, and C5 cervical spinal roots are the source of the phrenic nerve. The rhyme “C3, 4, and 5 keep the diaphragm alive” might help you remember this. The largest contribution comes from spinal root C4, with smaller contributions coming from C3 and C5, as well as some connecting fibres from the cervical plexus.
The anterior scalene muscle’s lateral edge is where the nerve emerges. The cervical fascia’s prevertebral layer is then reached by passing inferiorly along the anterior surface of the anterior scalene. On both sides, the nerve proceeds posteriorly to the subclavian vein. From here, the left and right phrenic nerves follow different courses:
In the thorax, the right and left phrenic nerves follow various paths, but in general, they descend as laterally as they can while maintaining touch with the mediastinal pleura. Both move in front of their respective hilum and bronchi.
Along the right side of the right brachiocephalic vein and the superior vena cava, the right Phrenic nerve descends in the thorax. It goes along the right side of the pericardium, which divides the nerve from the right atrium and passes in front of the right lung’s root. It subsequently makes its way to the diaphragm by descending on the right side of the inferior vena cava. Its terminal branches supply the core region of the peritoneum on its underside through the caval orifice in the diaphragm.
Phrenic nerves on the right and left supply the ipsilateral dome of the diaphragm.
Along the left side of the left subclavian artery, the left Phrenic nerve descends in the thorax. Here, it crosses the left side of the left Vagus nerve as well as the left side of the aortic arch. It travels in front of the left lung’s root before descending across the pericardium’s left surface, which divides the nerve from the left ventricle. The terminal branches puncture the muscle of the diaphragm as they approach it and feed the underside of the central region of the peritoneum.
Supply:
Each hemidiaphragm receives all of its motor supply from the phrenic nerve. Additionally, it supplies sensory data to:
- Diaphragm (apart from the diaphragm that is most proximally supplied by intercostal nerves)
- Internal pleura
- Pericardium, peritoneum, and diaphragmatic pleura in their core regions.
Motor Function:
The primary respiratory muscle, the diaphragm, receives motor innervation from the phrenic nerve.
Each phrenic nerve serves the ipsilateral side of the diaphragm (the hemidiaphragm on the same side as itself), as the phrenic nerve is a bilateral structure.
Sensory Function:
The core region of the diaphragm, as well as the peritoneum and pleura around it, are supplied by sensory fibres from the phrenic nerve. The nerve also transmits sensation to the pericardium and mediastinal pleura.
What diseases and circumstances impact the phrenic nerve?
A phrenic nerve injury can cause diaphragm paralysis or weakening. Your capacity to exchange air with your lungs is impacted by a paralyzed diaphragm.
Depending on where the phrenic nerve damage is, both sides of your diaphragm may become paralyzed. Bilateral diaphragm paralysis that is severe requires artificial ventilation in order to breathe.
Why does the diaphragm become paralyzed?
Diaphragm paralysis can be brought on by:
- Disorders that are autoimmune and inflammatory, such as neuralgic amyotrophy (Parsonage-Turner syndrome) and Guillain-Barré syndrome.
- Birth abnormalities or injuries sustained by a baby during delivery.
- Cervical spondylosis, which affects the neck’s spinal tissues and bones.
- Complications after procedures on the neck or the chest, including coronary artery bypass surgery.
- Other neurological conditions include multiple sclerosis and amyotrophic lateral sclerosis (Lou Gehrig’s disease).
- Spinal cord trauma, among other injuries.
- Lung cancer, metastatic malignancies, and spinal tumours.
What symptoms might indicate a paralyzed diaphragm?
Although some causes, such as neuralgic amyotrophy, may result in shoulder discomfort and arm weakness on the afflicted side, a person with unilateral diaphragm paralysis may not exhibit any noticeable symptoms. Bilateral paralysis of the diaphragm can be detected by:
- Breathlessness, especially while laying down or when submerged (as in a pool).
- Ongoing pneumonia.
- Sleep apnea, trouble falling asleep, or extreme daytime weariness.
- (In a newborn or youngster) Weak cries.
Phrenic Nerve Palsy
Injury to the phrenic nerve, which travels from the neck to penetrate the diaphragm next to the pericardium, results in phrenic nerve palsy, also known as phrenic nerve paresis or paralysis.
Surgery, particularly thoracic and heart surgery, is a significant cause of phrenic nerve damage. While dissecting close to an internal thoracic artery, the left phrenic nerve can be damaged since it descends anteriorly between the pericardium and mediastinal pleura.
Additional causes of phrenic nerve loss include harsh or penetrating trauma, metabolic conditions like diabetes, viral disorders like Lyme disease and herpes zoster, direct tumour invasion, neurological conditions including cervical spondylosis and multiple sclerosis, myopathy, and immunological conditions.(e.g., Guillain-Barre syndrome)
One further reason is damage to the spinal cord. Nerve impulses may be obstructed depending on which vertebrae are hurt. If the damage occurs above the third vertebrae, it is more likely. Breathing is often unaffected if the damage is to a lower portion of the spine.
Due to nonspecific signs and symptoms such as unexplained shortness of breath, recurrent pneumonia, anxiety, insomnia, morning headache, excessive daytime somnolence, orthopnea, fatigue, and difficulty weaning from mechanical ventilation, the diagnosis of phrenic nerve injury requires a high degree of suspicion.
Physical exams may reveal changes in the afflicted side’s breath sounds, dullness to chest percussion, and inward displacement of the epigastrium during inspiration.
If you experience breathing difficulties at any moment, you should see a doctor. A chest x-ray taken by your doctor may reveal that the diaphragm on the paralyzed side is locked in a higher position. It may be determined whether one side of the diaphragm is immobile by fluoroscopy or ultrasound.
Most people with unilateral diaphragmatic paralysis that is asymptomatic do not need to be treated.
A highly helpful therapy approach that enables weaning from artificial breathing is the plication of the afflicted location. In non-morbidly obese individuals with unilateral diaphragmatic paralysis, plication is preferred. In order to stop the lungs from expanding outward during exhaling (breathing out), a surgical plication stabilizes the diaphragm.
Fortunately, even with one-sided diaphragmatic paralysis, you can typically lead a normal life. But breathing is severely hampered if both phrenic nerves are injured. It may therefore be necessary to do procedures like intercostal nerve transfer or phrenic nerve stimulation in order to regain diaphragmatic mobility. You could require mechanical ventilation for the remainder of your life if these are unsuccessful.
Pacing using diaphragms: This is a technique to get the phrenic nerve working again. An electronic pacemaker can be inserted into the body and connected to the phrenic nerve if it is present but not functioning. This causes breathing and diaphragmatic action by periodically stimulating the phrenic nerve.
Now, laparoscopy can be used to do this procedure. It allows for speech, removes the need for a mechanical ventilator, and enhances quality of life.
Stimulation of the phrenic nerve. When the phrenic nerve is healthy and there are no signs of myopathy, phrenic nerve stimulation is conducted. Patients with bilateral diaphragmatic paralysis and cervical spine injuries may undergo this procedure.
Microsurgery: Microsurgery is a possible treatment if the phrenic nerve has been compromised. The phrenic nerve will be joined at both ends by a skilled surgeon. To prevent stretching, a nerve transplant can be required.
When possible, phrenic nerve restoration may be the best initial line of therapy in an effort to recover the function of the paralyzed hemidiaphragm.
Summary:
Breathing relies heavily on the phrenic nerves. They make your diaphragm contract or expand to allow your lungs to take in and expel air. The diaphragm may become paralyzed if a phrenic nerve is injured. You may experience respiratory problems in addition to sleep problems. People who suffer from severe phrenic nerve injury could require a mechanical ventilator to breathe.
FAQs:
The neck is where the phrenic nerve starts. It is made up of C3, C4, and C5 nerve fibers and descends down the scalenus anterior muscle’s anterior surface before entering the thorax to provide the diaphragm with motor and sensory input. The nerve in the neck is sensitive to acute damage because of its anatomical placement.
The C3, C4, and C5 cervical spinal roots are the source of the phrenic nerve. The rhyme “C3, 4 and 5 keep the diaphragm alive” might help you remember this. The largest contribution comes from spinal root C4, with smaller contributions coming from C3 and C5, as well as some connecting fibers from the cervical plexus.
Damage to or irritation of the phrenic or vagus nerves is a factor in chronic hiccups. The diaphragm muscle is supplied by these nerves.
Although the capacity to breathe freely is more likely to be linked to a C5 damage level, diaphragmatic weakness may also be present. There are signs of weakened inspiration, a weak cough, and immobility in the hands, trunk, and lower limbs.
While certain aspects of an injury—like its degree and severity—cannot be modified, others—like involvement in rehabilitation treatment, nutrition, and motivation—can have a big impact on recovery. After a spinal cord injury, many people may walk again with persistence and a good outlook.