Navicular Bone
Table of Contents
Introduction
The Navicular bone is one of the tarsal bones located in the foot. It is a small, boat-shaped bone that sits on the inner side of the foot, between the talus bone (ankle bone) and the cuneiform bones (located closer to the toes). The navicular bone plays a crucial role in maintaining the arch of the foot and providing stability during walking and running.
The navicular bone is a small but crucial bone in the foot that supports the arch and provides stability during walking and running. Understanding its anatomy and function is essential for diagnosing and treating various injuries and conditions that can affect this bone.
Anatomy of navicular bone
The navicular bone is situated on the medial side of the foot, between the talus bone (which is connected to the tibia) and the three cuneiform bones (which are connected to the metatarsals). It is roughly triangular in shape, with a concave superior surface and a convex inferior surface.
The superior surface of the navicular bone articulates with the talus bone, forming the talonavicular joint. This joint allows for inversion and eversion movements of the foot. On the superior surface, there is also a groove called the tibialis posterior groove, which serves as a passage for the tendon of the tibialis posterior muscle.
The inferior surface of the navicular bone has two facets that articulate with the cuneiform bones. These articulations form the cuneonavicular joints, which contribute to the stability and flexibility of the midfoot.
The medial side of the navicular bone is known as the tuberosity, which serves as an attachment site for various ligaments and tendons. The posterior aspect of the tuberosity has a roughened area called the groove for the flexor hallucis longus tendon, which is responsible for flexing the big toe.
Articulation of Navicular bone
The navicular bone articulates with several other bones in the foot, forming important joints that contribute to the overall function and stability of the foot.
- Talonavicular Joint: The superior surface of the navicular bone articulates with the talus bone, forming the talonavicular joint. This joint allows for inversion and eversion movements of the foot. The articular surface of the navicular bone is concave, while the talus bone has a convex surface, allowing for smooth gliding and rotation of the foot.
- Cuneonavicular Joints: The inferior surface of the navicular bone has two facets that articulate with the three cuneiform bones. These articulations form the cuneonavicular joints. There are three cuneiform bones which are medial cuneiform, intermediate cuneiform, and lateral cuneiform. These joints contribute to the stability and flexibility of the midfoot.
- Medial Cuneonavicular Joint: The medial facet of the navicular bone articulates with the medial cuneiform bone.
- Intermediate Cuneonavicular Joint: The intermediate facet of the navicular bone articulates with the intermediate cuneiform bone.
- Lateral Cuneonavicular Joint: The lateral facet of the navicular bone articulates with the lateral cuneiform bone.
These articulations allow for movements such as plantarflexion, dorsiflexion, and pronation and supination of the foot.
Functions of the Navicular Bone
The navicular bone in the foot serves several important functions:
- Weight-bearing: The navicular bone plays a crucial role in distributing the weight and forces generated during walking, running, and other weight-bearing activities. It helps to transfer the load from the talus bone (which connects the foot to the leg) to the cuneiform bones and metatarsals (long bones of the foot).
- Arch support: The navicular bone is an integral part of the medial longitudinal arch of the foot, which is responsible for maintaining the foot’s overall shape and providing shock absorption. The arch helps to distribute forces evenly across the foot and provides stability during movement. The navicular bone, along with other bones and ligaments in the arch, helps to maintain its height and prevent excessive flattening (pronation) or elevation (supination) of the arch.
- Joint mobility: The articulations between the navicular bone and other bones in the foot allow for various movements that are essential for normal foot function. The talonavicular joint enables inversion (turning the sole of the foot inward) and eversion (turning the sole of the foot outward) movements, which are important for balance and adaptability on uneven surfaces. The cuneonavicular joints contribute to plantarflexion (pointing the toes downward), dorsiflexion (pulling the toes upward), pronation (rolling the foot inward), and supination (rolling the foot outward) of the foot.
- Stability: The navicular bone, along with its ligamentous attachments, provides stability to the foot by acting as a connection point for various muscles, tendons, and ligaments. The plantar calcaneonavicular ligament (Spring ligament) helps to support the medial longitudinal arch and prevents excessive flattening of the arch during weight-bearing activities. The tibialis posterior tendon, which passes through the tibialis posterior groove on the navicular bone, provides stability and support to the foot during walking and running.
Overall, the navicular bone plays a crucial role in weight-bearing, arch support, joint mobility, and stability of the foot. Its articulations with other bones and ligamentous attachments contribute to the overall function and stability of the foot during various activities.
Muscle attachment
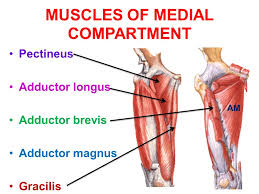
The navicular bone serves as an attachment site for several muscles, ligaments, and tendons in the foot. These attachments play a crucial role in maintaining the stability and movement of the foot. Here are the main muscle attachments of the navicular bone:
- Tibialis Posterior: This muscle is located in the back of the calf and runs down the inner side of the leg. It attaches to the medial surface of the navicular bone. The tibialis posterior muscle helps support the arch of the foot and controls its inward rolling motion (pronation) during walking and running.
- Flexor Digitorum Longus: This muscle is also located in the back of the calf and runs down the inner side of the leg, parallel to the tibialis posterior muscle. It attaches to the medial surface of the navicular bone, just below the attachment of the tibialis posterior muscle. The flexor digitorum longus muscle flexes the toes and helps maintain balance during walking and running.
- Tibialis Anterior: This muscle is located in the front of the lower leg and runs down the outer side of the leg. It attaches to the lateral surface of the navicular bone. The tibialis anterior muscle helps control the upward movement of the foot (dorsiflexion) and supports the arch during weight-bearing activities.
- Plantar Calcaneonavicular Ligament (Spring Ligament): This ligament connects the calcaneus bone (heel bone) to the navicular bone on its plantar (bottom) surface. It provides support to the arch of the foot and helps maintain its shape during weight-bearing activities.
- Dorsal Radiocarpal Ligament: This ligament connects the navicular bone to the cuneiform bones on its dorsal (upper) surface. It helps stabilize and support the midfoot during movement.
- Plantar Tarsal Ligaments: These ligaments attach to the plantar surface of the navicular bone and connect it to the other tarsal bones, including the cuneiform bones and the talus bone. They provide stability and support to the arch of the foot.
These muscle attachments and ligaments work together to support the arch of the foot, maintain proper alignment of the midfoot, and provide stability during walking and running. Any disruption or injury to these attachments can result in pain, instability, and altered foot mechanics.
Blood and lymph supply
The blood supply to the navicular bone is primarily provided by branches of the posterior tibial artery, which is a major artery in the lower leg. These branches include the medial plantar artery and the lateral plantar artery. The medial plantar artery gives off small branches that supply blood to the medial surface of the navicular bone, while the lateral plantar artery gives off branches that supply blood to the lateral surface of the navicular bone.
In addition to these branches, the navicular bone also receives blood supply from the dorsal pedal artery, which is a branch of the anterior tibial artery. This artery supplies blood to the dorsal (upper) surface of the navicular bone.
The lymphatic drainage of the navicular bone follows a similar pattern to its blood supply. Lymphatic vessels accompany the arteries and drain lymph fluid from the bone. The lymph fluid then passes through lymph nodes located in the foot and lower leg before eventually draining into larger lymphatic vessels and returning to the bloodstream.
It is important to note that the blood and lymph supply of the navicular bone can vary among individuals, and there may be additional sources of blood supply from other arteries in the foot.
Overall, a healthy blood and lymph supply is essential for maintaining proper bone health and healing potential in the navicular bone. Any disruption or impairment in these supplies can potentially lead to compromised bone health, delayed healing, or increased risk of complications following injuries or surgeries involving the navicular bone.
Conditions that affect navicular bone
The navicular bone is a small bone located in the midfoot, between the talus bone and the cuneiform bones. It plays an important role in maintaining the arch of the foot and facilitating smooth movement during walking and running. However, the navicular bone is susceptible to various conditions that can cause pain and dysfunction. Some of the associated conditions of the navicular bone include:
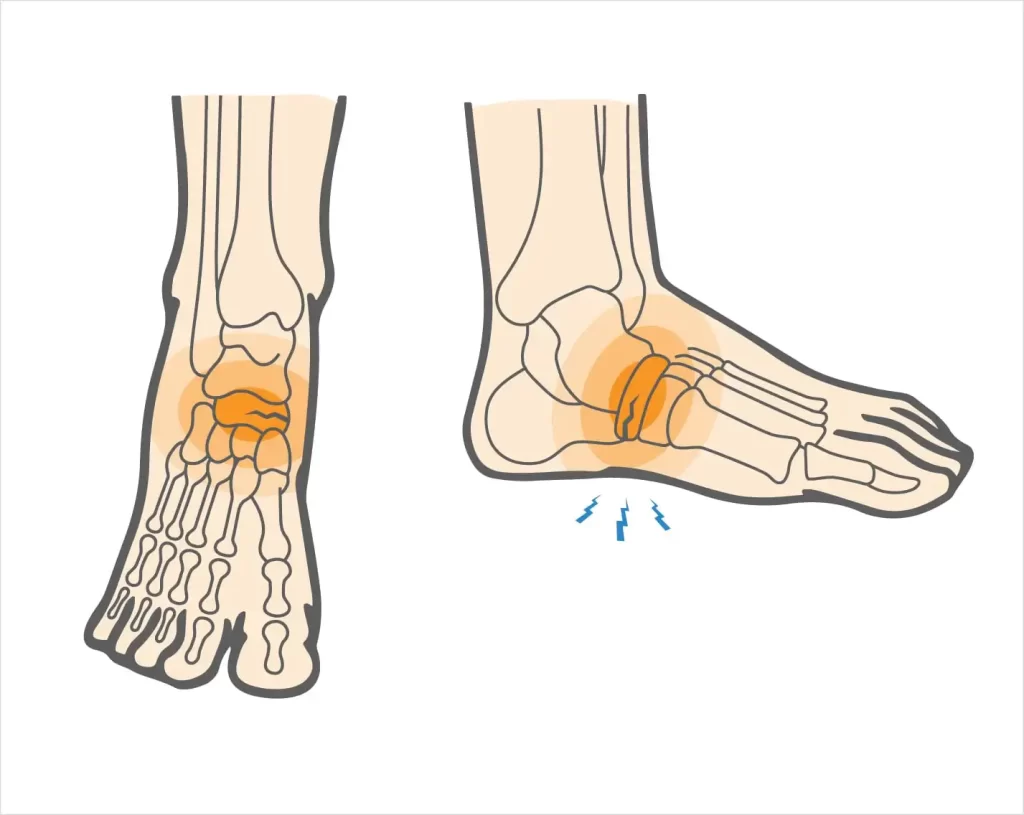
Navicular Stress Fracture: This is a common injury among athletes, particularly those involved in activities that involve repetitive stress on the foot, such as running or jumping. Stress fractures occur when there is repeated microtrauma to the bone, leading to small cracks or fractures. Navicular stress fractures can cause pain in the midfoot area that worsens with activity and improves with rest.
Accessory Navicular Syndrome: Some individuals may have an extra piece of bone called an accessory navicular, which is located on the inner side of the foot, near the navicular bone. This condition can cause pain and discomfort, especially during physical activity or when wearing tight shoes. Treatment options may include rest, orthotics, physical therapy, or in some cases, surgical removal of the accessory navicular.
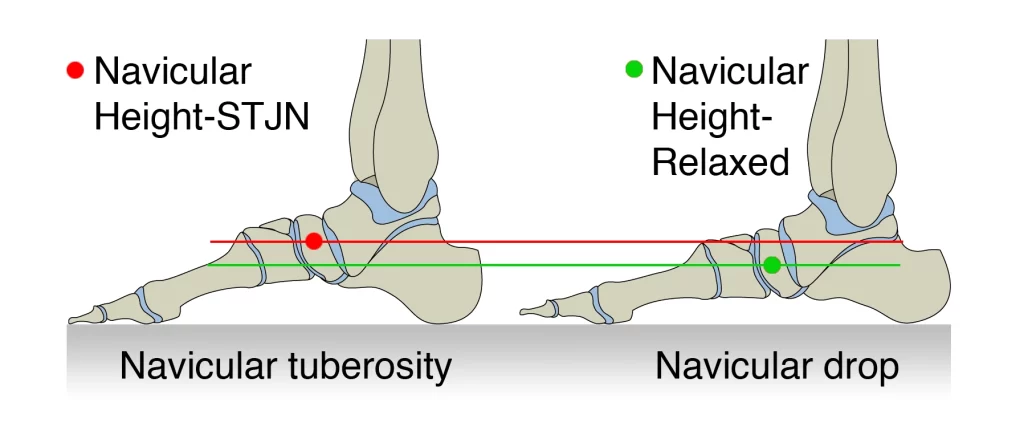
Navicular Drop: This condition refers to a collapse or sinking of the navicular bone, leading to a flattened arch of the foot. Navicular drop can be caused by various factors, including ligamentous laxity, muscle imbalances, or excessive pronation (inward rolling) of the foot. It can result in foot pain, instability, and altered biomechanics during walking or running.
Osteonecrosis: Also known as avascular necrosis, this condition occurs when there is a loss of blood supply to the navicular bone, leading to bone cell death and potential collapse of the bone. Osteonecrosis of the navicular bone is relatively rare but can cause chronic foot pain and disability. It can be caused by trauma, prolonged use of corticosteroids, or certain medical conditions such as sickle cell disease or systemic lupus erythematosus.
Tarsal Coalition: A tarsal coalition refers to an abnormal connection or fusion between two or more bones in the foot. In some cases, the navicular bone may be involved in this coalition, leading to restricted movement and pain in the midfoot area. Tarsal coalition can be congenital (present at birth) or acquired due to injury or inflammation.
Navicular Dislocation: Dislocation of the navicular bone is a rare condition that usually occurs as a result of severe trauma, such as a high-energy fracture or dislocation. It can cause significant pain, deformity, and instability of the foot. Prompt medical attention is required to reduce the dislocation and stabilize the foot.
Treatment for navicular bone conditions depends on the specific condition and its severity. It may include rest, immobilization with a cast or boot, physical therapy, orthotics, anti-inflammatory medications, and in some cases, surgery to repair or remove damaged tissues or correct structural abnormalities. Early diagnosis and appropriate management are crucial for preventing long-term complications and promoting optimal healing and function of the navicular bone.
Rehabilitation of navicular bone
Rehabilitation of the navicular bone depends on the specific condition and its severity. Here is a general overview of the rehabilitation process for some common navicular bone conditions:
- Navicular Stress Fracture:
- Rest: The first step in rehabilitating a navicular stress fracture is to rest and protect the foot from further stress. This may involve using crutches or a walking boot to offload weight from the affected foot.
- Immobilization: In some cases, a cast or walking boot may be used to immobilize the foot and promote healing of the fractured bone.
- Gradual Return to Activity: Once the pain subsides and healing progresses, a gradual return to activity is initiated. This may involve a progressive increase in weight-bearing activities, such as walking or jogging, under the guidance of a healthcare professional.
- Strengthening and Conditioning: As healing progresses, specific exercises to strengthen the foot and lower leg muscles may be prescribed. These exercises help improve stability, prevent future injuries, and promote optimal function of the navicular bone.
- Accessory Navicular Syndrome:
- Rest and Modification of Activities: Resting the foot and avoiding activities that exacerbate symptoms are typically the initial steps in managing accessory navicular syndrome. Modifying footwear to accommodate the extra bone may also be recommended.
- Orthotics: Custom orthotic devices can provide support and reduce stress on the accessory navicular bone. These devices are designed to correct any biomechanical abnormalities and promote proper foot alignment.
- Physical Therapy: Physical therapy may be recommended to strengthen the surrounding muscles, improve flexibility, and address any imbalances or abnormalities in foot mechanics.
- Surgical Intervention: In cases where conservative measures fail to alleviate symptoms, surgical removal of the accessory navicular bone may be considered.
- Navicular Drop:
- Orthotics: Custom orthotic devices are often prescribed to support the arch of the foot and prevent excessive pronation. These devices help redistribute forces and reduce stress on the navicular bone.
- Strengthening Exercises: Specific exercises targeting the muscles of the foot, ankle, and lower leg can help improve stability and support the arch. These exercises may include toe curls, calf raises, and balance training.
- Gait Analysis and Biomechanical Correction: A gait analysis may be conducted to assess any abnormalities in walking or running mechanics. Based on the findings, corrective measures such as modifying footwear or altering running techniques may be recommended.
- Non-Weight Bearing: In cases of severe osteonecrosis, non-weight bearing or limited weight-bearing with crutches may be necessary to protect the bone and allow for healing.
- Medications: Medications to manage pain and reduce inflammation may be prescribed.
- Physical Therapy: Once the bone begins to heal, physical therapy may be initiated to restore range of motion, strengthen surrounding muscles, and improve overall foot function.
- Tarsal Coalition:
- Immobilization: Immobilization with a cast or walking boot may be necessary initially to allow for healing.
- Physical Therapy: Once the immobilization period is over, physical therapy may be recommended to restore range of motion, improve strength and flexibility, and address any gait abnormalities.
- Surgical Intervention: In some cases, surgical intervention may be required to remove the abnormal connection between bones and restore normal foot mechanics.
- Navicular Dislocation:
- Emergency Treatment: Navicular dislocations require immediate medical attention. The dislocated bone needs to be reduced (put back into place) as soon as possible to prevent further damage.
- Immobilization: After reduction, the foot is typically immobilized with a cast or splint to allow for healing and stabilization.
- Physical Therapy: Once the bone has healed sufficiently, physical therapy is initiated to restore the range of motion, strength, and stability of the foot.
It is important to note that the rehabilitation process for each individual may vary depending on factors such as the severity of the condition, individual goals, and response to treatment. A healthcare professional, such as a physical therapist or orthopedic specialist, should be consulted to develop an individualized rehabilitation plan for navicular bone conditions.
FAQs
One common condition related to the navicular bone is navicular stress fracture, which occurs due to repetitive stress on the bone. Other conditions include navicular drop, where the arch of the foot collapses, and navicular syndrome, which involves inflammation of the surrounding tendons.
In some cases, a navicular stress fracture can heal on its own with proper rest and immobilization. However, it is important to seek medical attention for an accurate diagnosis and appropriate treatment plan.
The healing time for a navicular stress fracture can vary depending on the severity of the injury and individual factors. It typically takes several weeks to several months for complete healing.
Yes, orthotics or shoe inserts can help provide support and relieve pressure on the navicular bone, reducing pain and discomfort. Custom-made orthotics are often recommended for optimal results.


One Comment