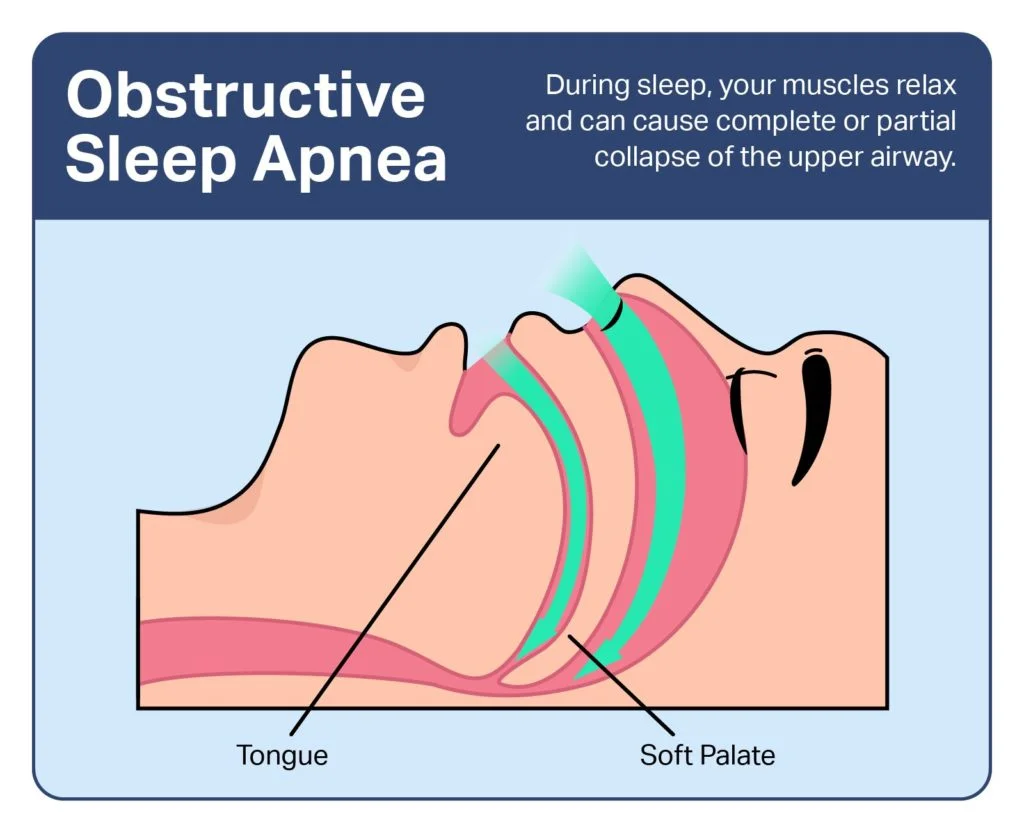
Obstructive sleep apnea
- Obstructive sleep apnea is a disorder that causes you to end breathing while asleep. Your brain tries to cure you by waking you up enough to breathe, but this prevents restful, healthy sleep. Over time, this condition can cause severe complications. However, this condition is sometimes very manageable, especially with close adherence to prescribed treatments.
Table of Contents
What is obstructive sleep apnea?
- Obstructive sleep apnea is a condition that causes you to stop breathing while you are sleeping. The word “apnea” comes from the Greek word for “breathless.” Sleep apnea occurs because you stop breathing in your sleep. This occurs either because of blockage of your airway (obstructive sleep apnea) or because your brain does not correctly control your breathing (central apnea).
- The resulting loss of oxygen activates a survival reflex that wakes you up just enough to resume breathing. While that reflex keeps you alive, it interrupts your sleep cycle. That cures restful sleep and can have other effects, including putting stress on your heart that can have potentially deadly consequences.
Whom does obstructive sleep apnea affect?
- Obstructive sleep apnea can happen to anyone, ranging from infants and children to older adults.
Obstructive sleep apnea is more usual in certain circumstances and groups of people:
- Before age 50, it is more usual in men and people assigned male at birth (AMAB). Later age 50, it affects women and people assigned female at birth (AFAB) at the same rate.
- People are more likely to create it as they get older.
- Having excess weight or obesity strongly improves the risk of developing it.
- It is more common in people who are Black, Hispanic, or of Asian descent.
Central sleep apnea is most usual in certain groups of people:
- People who grab opioid pain medications,
- Adults over 60 (sixty) years old,
- People with heart conditions such as atrial fibrillation or congestive heart failure (CHF).
- For certain people using CPAP or who have obstructive sleep apnea, this can trigger the development of central events knowns as treatment-emergent central sleep apnea.
- When people live at high altitudes, this can cause central apneas to happen.
How common is obstructive sleep apnea?
- Sleep apnea is uncommon yet widespread. Experts estimate it harms about 5% to 10% of people worldwide.
How does sleep apnea affect my body?
- To understand how obstructive sleep apnea works, it helps to know a little bit about the human sleep cycle.
Sleep occurs in multiple stages:
- Stage 1: Light sleep. This is a short stage that begins right later you fall asleep. It accounts for about 5% of your full sleep time.
- Stage 2: Deeper sleep. This stage is deeper and creates up about 45% to 50% of all the time you spend sleeping (this number goes up as you get older).
- Stage 3: Slow wave sleep. This is the deepest sleep stage, creating up about 25% of the time you spend sleeping (this number goes down with age). It is very hard to wake someone up in stage three sleep, and waking up directly from it usually causes “sleep inertia,” a state of “mental fog” and slowed thinking. Parasomnias such as sleepwalking and sleeptalking happen in this stage.
- REM sleep: REM called for “rapid eye movement.” This stage is when you dream. When a person is in REM (rapid eye movement) sleep, you can see their eyes moving beneath their eyelids.
- When you fall asleep, you typically enter Stage one and then move into and cycle between Stages 2 and 3. Later cycling between those stages, you will ultimately go into REM sleep and start dreaming. Later the first REM cycle, you start a new cycle and go back into Stage 1 or 2. One cycle normally takes about 90 to 110 minutes previous another begins. Most people go through 4 or 5 cycles per night (assuming they get a full eight hours of sleep).
How sleep apnea disrupts your sleep cycle?
- Your brain continuously monitors your body’s status and adjusts your heart rate, blood pressure (BP), breathing, etc. Your blood oxygen levels can drop when you end breathing because of either apnea or hypopnea.
- Apnea: This is when you end up breathing while asleep or have almost no airflow. It combines the Greek roots “a,” which means “not” and “pnea,” which mentions breathing. Combined, it means “breathless.”
- Hypopnea: This combines the Greek word roots “hypo” and “pnea.” The root “hypo” means “low” or “under.” Combining these root words means “under-breathing” or “low breathing,” which means you are not breathing enough to maintain oxygen levels in your blood.
- Your brain reacts to blood oxygen decreases — from either apnea or hypopnea — by triggering a failsafe-such as a reflex, waking you up enough for you to breathe again. Once you restart breathing, your brain automatically tries to resume your sleep cycle.
- The more severe your sleep apnea is, the more often you will these interruptions happen. The apnea/hypopnea index (AHI) is the average hourly number of apnea or hypopnea events — times when a person ends up breathing. The apnea/hypopnea index (AHI) is the main factor determining the severity of sleep apnea.
The severity is as follows:
- Mild sleep apnea: This level means a person has an apnea/hypopnea index (AHI) between 5 and 15. That means they have between five and 15 apnea or hypopnea events per hour. However, healthcare providers (doctors) also consider symptoms at this level. If you do not have other symptoms, they may not consider it severe enough to treat.
- Moderate sleep apnea: People with moderate sleep apnea have middle 15 and 29 events per hour. That means a person who sleeps 8 hours stops breathing and/or wakes up between 120 and 239 times.
- Severe sleep apnea: People with serious sleep apnea wake up 30 or more times in an hour. That means they stop breathing and/or wake up 240 times or more during a whole eight hours of sleep.
- Obstructive events, which are very short-lived, can harm any stage of sleep. They are most common in Stage 1, Stage 2, and REM sleep. That is why it is common for people to not remember apnea events, which means they may not know they have a problem until the symptoms are noticeable. Central events are most usual in Stages 1 and 2 of sleep but can occur during any stage.
What are the symptoms of sleep apnea?
- Sleep apnea has many symptoms, certain of which are easier to spot than others.
The symptoms involve:
- Feeling drowsy or even exhausted when waking up: Even later a full night’s sleep, people with sleep apnea commonly feel extremely tired.
- Daytime sleepiness: In more serious cases, this can cause drowsiness during driving, working, or other activities.
- Snoring: This is a common feature with sleep apnea (but it is not something that happens in all cases). You can have obstructive sleep apnea without snoring at all.
- Mood changes: Depression and anxiety are usual symptoms of sleep apnea.
- Disruptions in brain function: These can involve memory loss, trouble concentrating, or other brain-related issues.
- Waking up frequently in the middle of the night: This symptom might be harder to notice because people usually do not remember waking up or why they woke up. People who do this often remember waking up for another reason, such as heartburn or needing to go to the bathroom.
- Pauses in breathing while asleep that others witness: A spouse, partner or other loved one may notice these symptoms while you are asleep.
- Uncommon breathing patterns: Cheyne-Stokes breathing (CSB) is a distinctive breathing pattern that can occur with central sleep apnea. Cheyne-Stokes breathing (CSB) causes fast breathing that gets deeper and then shallower again until breathing stops altogether. Later not breathing for several seconds, they will start breathing again, then, start the pattern all over again.
- Insomnia.
- Night sweats & feeling restless at night.
- Sexual dysfunction.
- Waking up feeling short of breath or as you are choking.
- Headaches, especially when waking up.
Sleep apnea in children
- Sleep apnea in children can occur in slightly different ways.
The symptoms of sleep apnea in children involve:
- Hyperactivity or difficulty focusing or performing poorly in school. This can look such as symptoms of attention-deficit/hyperactivity disorder (ADHD).
- Loud snoring.
- Bedwetting.
- Repeat arm or leg movements while asleep.
- Sleeping in uncommon positions or sleeping with their neck extended.
- Reflux (heartburn) or night sweats.
What causes sleep apnea?
- Sleep apnea usually has specific causes, and there is evidence that it may run in families. Overall, there are 3 main forms of sleep apnea, with some differences in how and why they happen.
The types are:
- Obstructive sleep apnea (OSA),
- Central sleep apnea (CSA),
- Mixed/complex sleep apnea.
Obstructive sleep apnea (OSA)
- This is the more usual form. Obstructive sleep apnea happens when muscles in your head and neck relax while you are asleep, causing the surrounding tissue to press on your windpipe. That obstructs air’s ability to cross through it.
Central sleep apnea
- This form of sleep apnea occurs because of a problem in your brain. Under ordinary circumstances, your brain manages your breathing all the time, involving it while you sleep. Central sleep apnea happens when your brain does not send signals to keep breathing-related muscles working.
Central sleep apnea can happen for many reasons, involving:
- Heart failure,
- Low blood oxygen levels (hypoxia) because of great altitude,
- Nervous system damage, especially in your brainstem (which is what manages your breathing) or areas of your spinal cord,
- Managing obstructive sleep apnea initially with CPAP (this typically goes away with consistent CPAP use),
- Nervous system conditions such as amyotrophic lateral sclerosis (ALS, known as Lou Gehrig’s disease).
Mixed/complex sleep apnea
- There is also a mixed/complex type of sleep apnea. This form has a merge of both obstructive events & central events.
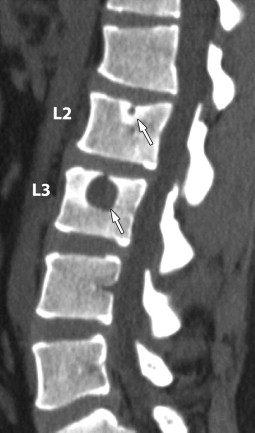
How is obstructive sleep apnea diagnosed?
- Diagnosing obstructive sleep apnea usually includes a healthcare provider (doctor) asking questions about your symptoms and history. If they suspect obstructive sleep apnea based on your symptoms and answers, they will likely want you to undergo testing for obstructive sleep apnea.
What tests will be done to diagnose obstructive sleep apnea?
The most common tests for sleep apnea involve:
- An overnight sleep study (polysomnogram): This is an overnight test where you sleep in a medical facility (often known as a “sleep lab”) that is specially equipped to be as comfortable as possible while still monitoring your sleep. This test includes sensors that monitor your heart rate (HR), breathing, blood oxygen levels, brain waves, and more. Experts examine this test as the gold standard for diagnosing sleep apnea.
- Home sleep apnea testing: This form of testing allows a person to whole a sleep study from home. It is similar to an overnight sleep study but does not involve brain wave monitoring. This test can not diagnose central sleep apnea, and it is usually not an option when providers suspect more severe sleep apnea, or if you have other sleep disorders or medical conditions. Often, when a home study does not show sleep apnea, experts recommend confirming this with an overnight sleep study.
How is obstructive sleep apnea treated, and is there prevention?
- There are many approaches to treating obstructive sleep apnea, turning on the specific type of sleep apnea and how severe it is. While none of these is a cure, they can assist prevent apnea events or reduce how often they happen or how severe they are.
- Many treatments should be an area of your daily (or nightly) routine. That can ultimately decrease or even throw obstructive sleep apnea’s effects on your life for as long as you use these treatments.
Possible treatments involve:
- Conservative (nonmedical) treatments,
- Positive airway pressure and adaptive ventilation devices,
- Oral appliances (mouthpieces),
- Nerve stimulators,
- Surgery,
- Medications (central sleep apnea only).
Conservative treatments
- These nonmedical treatments or approaches can commonly improve obstructive sleep apnea or resolve it. They are not cures, yet they can reduce apnea to the point where it stops happening or is not severe enough to cause symptoms.
These involve:
- Weight loss: A 10% decrease in body weight can significantly increase sleep apnea for people who have excess weight or obesity.
- Position changes while sleeping and sleep aid items: Sleeping on your back creates sleep apnea more likely to happen. Special support pillows and similar items can help change the position in which you sleep, keeping you off your back so soft tissue does not press on your windpipe and block breathing.
- Nasal sprays, adhesive strips, etc: These over-the-counter products improve breathing by creating it easier for air to travel through your nose. While they can not help moderate or severe sleep apnea, they can sometimes help snoring and mild sleep apnea.
- Treating the underlying condition: Treating conditions such as heart failure can often increase central sleep apnea.
- Medication changes: Working with your doctor to reduce or stop opioid pain medications may be able to improve or even resolve central sleep apnea.
Positive airway pressure (PAP) and adaptive ventilation
- Positive airway pressure (PAP) is a method that uses a specialized device to increase the air pressure inside of your airway while you inhale. This method can manage obstructive, central, and mixed sleep apneas.
- Pushing pressurized air down your windpipe retains it open so you can breathe. These devices push air through a hose that joins to a special mask you wear on your face while you sleep. Masks can cover your nose, mouth, or both, and there are many various types and styles to choose from.
- The best-known Positive airway pressure (PAP) device is the Continuous Positive Airway Pressure (CPAP) machine. However, there are other types of PAP machines, very much (look at our CPAP Machine article for more about the different types of devices, including adaptive servo-ventilation devices). These devices improve the air pressure inside your airway and lungs when you inhale, keeping surrounding tissue from pressing your airway shut.
Oral devices
- Obstructive sleep apnea occurs when the soft tissue in your head or neck, especially all over your mouth and jaw, presses downward on your windpipe. Special mouthpiece devices can assist hold your jaw and tongue in a position that keeps pressure off your windpipe. Dentists and sleep medicine specialists often work together to make these for people who require them.
Nerve stimulators
- The hypoglossal nerve (the name comes from Greek and means “under the tongue”) is what regions your tongue’s movements. A nerve stimulator connected to this nerve can stimulate it, pushing your tongue slightly forward when you breathe while you are sleeping. That retains your tongue from relaxing and pressing backward on your windpipe while you sleep, which is one of the ways that obstructive sleep apnea occurs.
- An electrode connects to the nerve under your jaw and connects to a device implanted under the skin in your chest. You can turn the stimulator on before you sleep and turn it off later you wake up. The electrical current is strong enough to retain your tongue from relaxing too much but mild enough that it is not uncomfortable.
- The same kind of nerve stimulation is also possible with central sleep apnea. This type of stimulation harms the phrenic nerves. This pair of nerves attach your spinal cord to the diaphragm, a layer of muscle underneath your lungs that controls your ability to inhale and exhale. Stimulating the phrenic nerve causes those muscles to flex, assisting you to breathe.
Surgery
- Surgeries on your nose, mouth, and throat can assist prevent blockages of your nose, throat, and windpipe. However, the impact of these in adults is commonly limited and varies from person to person.
These surgeries involve:
- Somnoplasty: This procedure uses radiofrequency (RF) to decrease soft tissue around the upper parts of your windpipe.
- Tonsillectomy/adenoidectomy: Tacking out your tonsils and adenoids can widen the opening where your mouth, throat, and nasal passages connect. That makes it easier for air to pass through and decreases soft tissue that can block your breathing. This procedure is most assist for children with obstructive sleep apnea.
- Uvulopalatopharyngoplasty (UPPP): This procedure takes out your uvula (the teardrop-shaped soft tissue that sways at the back of your mouth). It removes soft tissue from your soft palate and pharynx. These widen the area where your mouth and throat meet, creating it easier for air to pass through.
- Jaw surgery: Various surgery procedures can subtly change the position of your jaw so soft tissue can not easily press back on your airway. These procedures are especially helpful for people who have sleep apnea for structural reasons such as micrognathia.
- Nasal surgery: One usual form of nasal surgery is septoplasty, which straightens the soft tissue in your nose, making it easier for air to travel through your nose and nasal passages.
Medications for central sleep apnea
- In addition to positive airway pressure, adaptive ventilation, and phrenic nerve stimulators, there are some medications that may assist central sleep apnea. Some examples of these medications involve hypnotic (sleep-promoting) medications, respiratory-stimulating drugs, and more. However, no one of these medications is formally approved or definitively accepted for this utilization.
Physical Therapy Management
- Although there is little research providing sound evidence-based physical therapy interventions for obstructive sleep apnea (OSA) at this time, it often goes undiagnosed providing opportunities for physical therapists to identify, educate and refer patients who present with signs and symptoms of obstructive sleep apnea (OSA).
- Undiagnosed obstructive sleep apnea (OSA) is associated with an increased risk of hypertension, cardiovascular disease, motor vehicle accidents, and reduced quality of life.
Physical Therapists can educate patients on obstructive sleep apnea (OSA):
- Signs and symptoms,
- Risk factors,
- Associated co-morbidities,
- How to get diagnosed/tested,
- Risks of undiagnosed OS,
- Aerobic Exercise.
- Studies show a significant effect of exercise in reducing the severity of sleep apnea in patients with obstructive sleep apnea (OSA) with minimal changes in body weight. The interventions commonly involved aerobic activities for 30 minutes minimum on 3-5 days a week. The significant results of exercise on cardiorespiratory fitness, daytime sleepiness, and sleep efficiency indicate the potential value of exercise in the management of obstructive sleep apnea (OSA).
An example of physiotherapy intervention
- Supervision 150 min/week of aerobic exercise (treadmill, elliptical, trainer, or recumbent bicycle), performed at 60 % of heart rate (HR) reserve, spread across 4 days/week for 12 weeks,
- On 2 days/week for 12 weeks, aerobic exercise was followed by resistance exercise, consisting of 2 sets of 10–12 repetitions for 8 various exercises.
Tongue Exercises
- Physiotherapeutic treatment eg muscular exercises could have a place in the treatment of obstructive sleep apnea (OSA), particularly in mild cases. This treatment could help to prevent the muscular hypotonia that develops progressively in obstructive sleep apnea (OSA).
Below shows examples of exercises For Obstructive Sleep Apnea (OSA)
- Exercises for the tongue
Tongue brushing
Method:
- With your toothbrush brush the topmost and sides of your tongue, while your tongue is sitting on the deck of your mouth.
- Repeat the individual sections five times each.
- Complete the exercise 3 times daily.
Purpose – to strengthen the tongue muscles with the added advantage of maintaining high oral hygiene.
Tongue slide
Method:
- Seeing straight ahead, position the tip of your tongue against the back of your top, and front teeth.
- Slide your tongue in reverse.
- Repeat ten times.
Purpose – to tone & strengthen the tongue & throat muscles.
Tongue Force
Method:
- Force the back of your tongue downward until the full tongue is resting on the floor of your mouth.
- Retain the tip of your tongue touching the back of your lower teeth.
- Hold for four seconds.
- Repeat five times.
Purpose – both of these exercises strengthen the tongue and tone your mushy palate.
Tongue Press
Method:
- Push your tongue against your rigid palate (the top and front of your mouth).
- Do this for five seconds.
- Slide your tongue reverse to the back of your mouth.
- The initial 3rd of your tongue should be against your hard palate, not just the tip.
- Retain your jaw open throughout the exercise.
- Refrain from biting down – retain your teeth apart.
- Repeat this movement ten times.
- Repeat four times a day.
Purpose – to strengthen the genioglossus (the main muscle used for sticking your tongue out), and to improve the strength in the hyoid muscles and bone. The hyoid bone is placed in the center of the neck. It sits middle of the chin and thyroid cartilage.
- The exercise assists by putting the hyoid bone in the correct position and retaining it there1.
- The hyoid bone is a free-motioning, u-shaped bone in the neck. The volume of the tongue should decrease too.
What can or can not I eat or drink with obstructive sleep apnea?
- People who have obstructive sleep apnea should avoid heavy drinking, and frequently utilize sleeping pills or other drugs (recreational and otherwise) that cause heavy sedation. These can create obstructive sleep apnea worse. Your healthcare provider (doctor) can talk to you about drugs that can cause that and how you can avoid the effects.
Complications or side effects of the treatment
- The complications and side effects of the treatments turn on many factors, especially the treatments themselves. Your healthcare provider (doctor) is the best source of information for what you can do to minimize the side effects or prevent them when possible.
How to take care of myself or manage symptoms?
- Obstructive sleep apnea is a condition that can seriously disrupt your life and put you at risk for life-threatening complications and events (see more about these under the Outlook/Prognosis section below). Because of this, you should not try to self-diagnose or self-treat it. If you think you have obstructive sleep apnea, you should schedule an appointment with a sleep specialist or ask a primary care provider (doctor) to refer you to a sleep specialist.
How you can help with diagnosis?
- If you suspect you or a loved one has obstructive sleep apnea, you might be able to help a healthcare provider (doctor) diagnose it. Video and audio recordings of a person sleeping, especially where the provider can hear breathing, can give a provider (doctor) key evidence they need to speed up the diagnostic process.
How soon after treatment will I feel better?
- The time it takes to recover or feel better later treatment for sleep apnea depends on the treatments themselves. Some people will feel better almost immediately, while others may need 3 to 6 months of consistent nightly treatment to see the full benefits. Your healthcare provider (doctor) can tell you more about the timeline for your recovery and when you should expect to feel better.
- Devices that treat obstructive sleep apnea, especially positive airway pressure (PAP) devices, often bring very fast results. Older devices may take certain tweaking and adjusting (a process known as “titration”) of the settings, but many newer devices can often adjust automatically to meet your needs (especially if your sleep apnea is mild or on the decrease end of moderate).
- While some people may require to get used to wearing a mask to sleep, most people can overcome that fairly quickly. Many people see improvements immediately when they sleep through the night using a positive airway pressure (PAP) device.
How can I decrease my risk or prevent obstructive sleep apnea?
- Obstructive sleep apnea is sometimes preventable, especially in cases where it occurs because a person has excess weight or obesity. Still, certain people maintain a healthy body weight or are underweight and still develop obstructive sleep apnea. For those individuals, a structural issue is usually the cause of their apnea, so they can not prevent it.
The best things you can do to reduce your risk of sleep apnea involve:
- Reach and maintain a healthy weight,
- Practice good sleep hygiene,
- Treat any existing health conditions, such as high cholesterol, high blood pressure, and Type 2 diabetes.
What can I look for if I have obstructive sleep apnea?
- Obstructive sleep apnea is a condition that can severely disrupt your life, and it improves your risk of several conditions that are life-threatening medical emergencies. Even if it does not cause these dangerous complications, people with sleep apnea can not get restful sleep, so they constantly feel tired. In the worst cases, this condition can create them so tired that they may fall asleep during the day, leading to accidents or causing problems with work, hobbies, social activities, etc.
Dangerous complications of obstructive sleep apnea
- Obstructive sleep apnea is a dangerous condition because it can cause several various complications, many of which are severe or life-threatening.
These involve:
- Heart damage and heart failure: Sleep apnea causes an improvement in pressure in the blood vessels around your heart and in some of the chambers of your heart itself. That pressure improvement puts a strain on your heart, ultimately causing damage to the heart muscle itself.
- Arrhythmias, especially atrial fibrillation: Atrial fibrillation is a dangerous arrhythmia because it confounds how blood flows through the upper left chamber of your heart. That disruption causes blood to pool and lingers for a very long. That can cause blood clots, which can then leave your heart and travel directly to your brain, causing a stroke.
- Sudden cardiac death: Some arrhythmias that can occur with sleep apnea are especially severe and can stop your heart. That stoppage is a life-threatening condition known as immediate cardiac death.
- Daytime drowsiness: While feeling sleepy during the daytime may not seem harmful, it can be hazardous depending on what you are doing. If you fall asleep while driving or operating harmful machinery, that can have deadly implications for you or others around you.
How long does obstructive sleep apnea last?
- Obstructive sleep apnea is a long-term, chronic condition. For some people, it is possible to resolve it by reducing their weight or undergoing certain treatments. For others, it may be a whole life condition.
The outlook for obstructive sleep apnea
- The outlook for obstructive sleep apnea depends on many factors. The severity and type of obstructive sleep apnea create a difference. However, adhering to treatment is usually the biggest determining factor in how this condition harms your life.
- It is critical to adhere to treatment closely. Using and sticking with treatments, especially ongoing ones such as positive airway pressure devices, can make a huge difference. Many people stick with treatments such as positive airway pressure devices for a month or so but then stop using them. That can improve the risk of complications and a negative outcome.
How do I take care of myself?
There are so many key steps you can take to manage this condition:
- Make lifestyle changes as good as you can. Changing how you live your life, especially concerning diet and physical activity, can be a challenge. Do not feel ashamed to talk to your doctor about these struggles. Not only are these common, yet your healthcare provider can also likely help you minimize these or even overcome them.
- Serious about your treatment plan closely. Ultimately, people who adhere to the treatments and create them a part of their routine — never or rarely missing a night — are more likely to have good outcomes and avoid serious or dangerous complications.
- Talk to your provider (doctor) about what you are experiencing. You should talk to your provider (doctor) if you struggle to stick to treatment because of issues with a PAP device. It is usual for people to have issues with how a PAP device mask fits, pressure settings, etc. Your provider (doctor) can help you remedy these issues, stick to your treatments and get a good night’s sleep.
- See your provider (doctor) as recommended. Follow-up visits can be crucial, especially quick on, to make sure your treatments are working as they should.
When should I go to the ER?
- You should go to the ER if you notice any of the symptoms of a heart attack or stroke, both of which are more likely to occur with sleep apnea.
Summary
- Obstructive sleep apnea is a widespread condition that disrupts a person’s breathing while they sleep. That causes a person to wake up just enough to breathe, interrupting their sleep and retaining them from feeling rested.
- Over time, sleep apnea can conduct to serious or even deadly complications, so early diagnosis and treatment are vital. This condition is sometimes very treatable and there are many treatment options.
- The most usual — and most effective — treatments, especially positive airway pressure devices, are meant for use every night. The best outcomes from these treatments are most likely to occur when you stick to them and make them part of your life every day without exception.
- If you are struggling to stick to treatments, it is absolutely vital that you talk to your healthcare provider (doctor). They can assist you to find ways to overcome these issues so you can finally get a good night’s sleep.
FAQs
Anything that could narrow your airways such as obesity, large tonsils, or changes in your hormone levels can improve your risk for obstructive sleep apnea. Central sleep apnea occurs when your brain does not send the signals required to breathe.
Obstructive sleep apnea is considered a severe medical condition. Complications can involve Daytime fatigue and sleepiness. Because of less of restorative sleep at night, people with obstructive sleep apnea often have severe daytime drowsiness, fatigue, and irritability.
Sleep apnea is a dangerous condition because it can cause several various complications, many of which are severe or life-threatening. These involve Heart damage and heart failure. Sleep apnea causes an improvement in pressure in the blood vessels around your heart and in some of the chambers of your heart itself.
Sleep apnea affects men, women, and some children and it may run in families. Studies specify that 9% of middle-aged women and 24% of middle-aged men suffer from sleep apnea. However, these rates are much higher for people that are overweight and those diagnosed with high blood pressure (HBP), heart disease, and type 2 diabetes.
Obstructive sleep apnea (OSA) happens when a child stops breathing during sleep. The cessation of breathing commonly occurs because there is a blockage (obstruction) in the airway. Obstructive sleep apnea harms many children and is most commonly found in children between 2 and 6 years of age, but can happen at any age.
Tests to detect sleep apnea involve Nocturnal polysomnography. During this test, you are hooked up to equipment that monitors your heart, lung, and brain activity, breathing patterns, arm and leg movements, and blood oxygen (O2) levels while you sleep.
In general, obstructive sleep apnea (OSA) is a chronic condition that does not go away on its own. This is especially true if you are an adult, as your anatomy tends to same fixed from adolescence onwards. There are so many factors that can cause obstructive sleep apnea, many of which relate to a person’s anatomy.
Home remedies, such as healthful lifestyle changes and elevating the head at night, may assist reduce episodes of apnea. However, if a person has moderate or severe sleep apnea, they should look for a doctor. They will probably require to wear a CPAP device to support their breathing.




5 Comments