Musculocutaneous nerve injury:
Table of Contents
Overview:
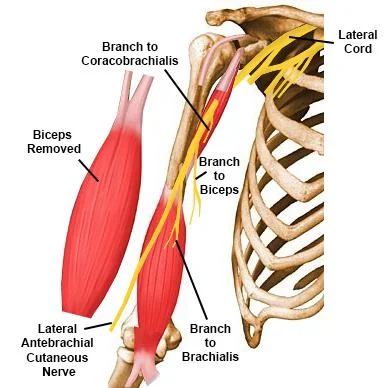
The musculocutaneous nerve originates from- C5-C6 nerve roots and the terminal branch of the lateral cord of the brachial plexus. it has both motor and sensory fibers. It supplies the muscles of the front of the arm and the skin of the lateral side of the forearm. The nerve passes through the coracobrachialis muscle and between the biceps and the brachialis muscle. Then it enters the elbow by piercing deep fascia and gives the Lateral Cutaneous nerve of the forearm. Above the elbow, it supplies only motor branches of nerve but below the elbow, it gives sensory branches. Due to anatomical variations, the clinical significance is also variable.
Musculocutaneous nerve injury is commonly associated with severe brachial plexus trauma. Isolated musculocutaneous neuropathy happens due to any trauma. This injury happens to any strenuous exercise. Injury to the nerve results in weakness of elbow flexion and supination movement. Sensation decreased on the lateral side of the forearm. The brachialis muscle is supplied by both the musculocutaneous nerve and the radial nerve. One study resulting that the musculocutaneous nerve contributes to 42% of the muscle power used for elbow flexion movement.
Anatomy of Musculocutaneous Nerve:
The musculocutaneous nerve originates from the fifth to seventh cervical nerve roots (C5 to C7), starts from the lateral cord, and then pierces to the coracobrachialis muscle. The musculocutaneous nerve emerges below the pectoralis minor muscle of the upper chest, near to the shoulder and armpit. That area of your body is called the axilla. The nerve enters the arm by running through the coracobrachialis muscle, where it joins the humerus bone of the upper arm.
Then runs down the upper arm between the brachialis and biceps brachii muscles. At the elbow, the nerve pierces connective tissue called the deep fascia and emerges near the biceps muscle tendon and brachioradialis muscle. After that, it runs down the lateral side of the forearm as the lateral cutaneous nerve and gives the branches and ends at the wrist.
The musculocutaneous nerve can go with the lateral head of the median nerve and subsequently it was given back as a communication to the musculocutaneous nerve. The musculocutaneous nerve supplies the flexor muscles on the front side of the arm, sensory supply on the lateral side of the forearm, and also to the elbow joint.
Root:
Ventral rami of C5, C6, C7.
Branches of Musculocutaneous nerve:
Motor branches:
Corocobrachialis Muscle
Brachialis Muscle
Biceps Brachii Muscle
Sensory branch:
lateral cutaneous nerve to the lateral forearm in front and back on both sides.
Articular Branch:
Humerus and Elbow joint
Functions of Musculocutaneous Nerve:
The musculocutaneous nerve runs through into the upper arm giving motor function to the muscles. When it enters the forearm known as the lateral cutaneous nerve and gives the sensory branch in the forearm.
Motor Function:
The Biceps, Brachialis, and Brachioradialis muscles are supplied by the musculocutaneous nerve and give movement to your arms. The musculocutaneous nerve works with the biceps to give the flexion movement of the arm at the elbow and shoulder, palm faces upward so it’s like a bodybuilder pose. The coracobrachialis muscle is situated inside the upper arm just below the biceps muscle. Its attachment is from the shoulder to the elbow. Muscle helps to flex the arm at the shoulder and plays a minor role in pulling the arm in toward the body.
The brachialis muscle is the primary muscle to helps flex the elbow. It starts in the middle of the upper arm, where it is situated under the biceps brachii muscle, then it passes through the elbow and connects to the ulna bone below the elbow joint. Muscle and their action which is supplied by the musculocutaneous nerve are the following:
- Coracobrachialis – flexion and adduction of the glenohumeral (GH) joint and stabilize the humeral head in the glenoid fossa when the arm is moving freely by side.
- Brachialis- flexion movement of the elbow joint.
- Biceps Brachii- It helps to stabilize the glenohumeral joint when elbow flexion and supination movement do with the weight.
Sensory Function:
The lateral cutaneous nerve runs down the forearm toward the wrist, it gives out multiple branches to the skin. The nerve provides sensation to the front half of the inner upper arm, from the elbow to the base of the thumb, and to the forward portion of your lateral part from the elbow to the wrist.
Anatomical Variation of Nerve:
The musculocutaneous nerve has different anatomical variations. In some people, it may:
Connect with, adhere to, and exchange fibers with the median nerve.
Runs under the coracobrachialis muscle instead of going through.
What is Musculocutaneous Nerve injury?
Injury is happen due to the direct trauma to the musculocutaneous nerve in any form of lacerations, gunshot injury, and any nearby bone fractures. Injury to the musculocutaneous nerve leads to biceps brachii and brachialis muscle weakness and atrophy and loss of sensation in the lateral forearm. This happens in active young adults that frequently do the arm and elbow flexion movement with the forearm pronated position. This nerve entrapment also occurs by the hypertrophy of the muscle.
Another important clinical scenario is a shoulder dislocation. While the most frequently injured nerve in this scenario is the axillary nerve, several cases of musculocutaneous nerve damage have been reported secondary to anterior humeral dislocations. The musculocutaneous nerve branches from the lateral cord just anterior to the glenohumeral joint, explaining its susceptibility to damage with anterior dislocations. Additionally, it has been found that downward traction and external rotation place significant tension on the nerve, and anterior humeral dislocations may place the nerve in this position.
Mechanism Musculocutaneous nerve injury:
The iatrogenic causes are prolonged positioning of the arm during an unrelated surgery or direct trauma to the nerve. Repetitive, jerky upper extremity activity (e.g. lifting, throwing, or carrying), or a forceful extension of the upper extremity (e.g. pushing or wrestling) are more common mechanisms of injury. Most common injuries to the musculocutaneous nerve occur to the biceps and brachialis muscles, at the coracobrachialis muscle, due to hypertrophy or strong contraction of the muscles, occur in mechanical or ischaemic nerve injury.
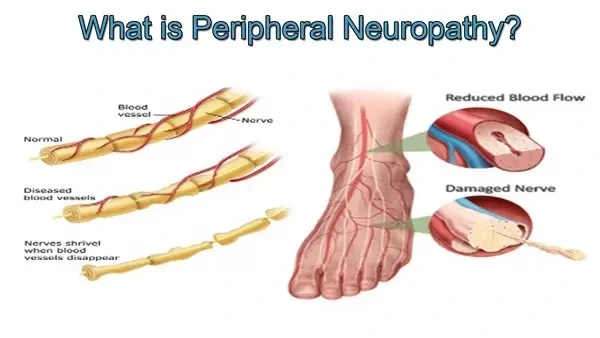
Peripheral nerve injuries have mainly 3 types: neuropraxia, axonotmesis, and neurotmesis.
Neuropraxia injuries are most common and involve a conduction block of motor or sensory function without damage to the neural elements and with intact connective tissue sheaths. This usually occurs due to compression, mild crush, traction, or local ischemia.
Axonotmesis is seen in axonal injury and distal axon degeneration with a connective tissue sheath and follows a more severe trauma that causes a crush injury.
Neurotmesis is a complete disruption of the nerve and nerve sheath and it is caused by a transaction or laceration of the nerve.
Nerve regeneration and repair processes occur differ entirely depending on the severity of the injury. With lesions, the involvement of axons is less than 20–30%. collateral sprouting from surviving axons occurs over 2–6 months. When more than 90% of axons are injured, nerve tissue regenerates from the injury site, and the rate of recovery depends on the distance to the injury site. Proximal injuries may be problematic because of the long distance to re-innervate distal muscles and the regeneration and repair phases continue for months. Peripheral nerve regeneration occurs at a rate of 1–2 mm per day.
Symptoms of Musculocutaneous nerve injury:
- Weakness in elbow flexion or shoulder flexion
- Atrophy of the biceps brachii
- Pain or paresthesia at the lateral forearm.
- Sensations are altered in that area which is supplied by the musculocutaneous nerve (Mainly the lateral side of the forearm).
What are the risk factors for musculocutaneous nerve injury?
- Injury to the shoulder and brachial plexus may affect the musculocutaneous nerve.
- Generate the pressure on the nerve by the biceps aponeurosis and tendon against the fascia of the brachialis muscle, it causes sensory affection below the elbow on the lateral side of the forearm.
- Musculocutaneous nerve injury can be one complication of shoulder joint replacement.
Diagnosis of Musculocutaneous nerve injury:
Physical Examination:
Neurodynamic testing: Check the physical capabilities of the peripheral nervous system by the movements of the upper limb. If the patient can’t do the movement properly and sensations are diminished the musculocutaneous nerve is injured.
Check the nerve tension or compression in the positioning of the patient for the musculocutaneous nerve may include the following: shoulder girdle depression, elbow extension, shoulder extension, ulnar deviation of the wrist with thumb flexion, and medial or lateral rotation of the arm.
Nerve palpation (sustained or unsustainable) and isometric contraction of a muscle supplied by the nerve may also identify mechanical sensitivity in neural structures.
If the nerve entrapment is present check the ULTT for the musculocutaneous nerve.
Sensory Examination: The therapist checks the sensation with the different equipment over the supplied muscle.
Manual muscle strength testing (MMST) can be a useful diagnostic tool to identify the strength of muscles that are supplied by the musculocutaneous nerve, including the biceps brachii, brachialis, and coracobrachialis. MMST is described in 0 – 5 grades.
- A grade of 5 is when the therapist applies maximum pressure and the patient breaks the pressure and does the movement.
- Grade 4 is a patient does complete movement in a full range against gravity but can’t hold the position against the maximum resistance of the therapist.
- A grade of 3 is when the patient does movement in complete a full range of motion against gravity but does not bear additional resistance.
- Grade 2 is muscle is so weak patient can’t do the movement against gravity.
- A grade of 1 is only some contractile activity visible or palpable, however, movement is not generated.
- A grade 0 is muscle completely inert on palpation. no movement is present.
Electro-diagnostic Test:
When entrapment neuropathies are diagnosed in the upper limb during the clinical assessment, different testing modalities can help to confirm the diagnosis.
Electrophysiological studies such as electromyography and nerve conduction studies usually give the location and severity of the injury.
- Ultrasonography and magnetic resonance imaging (MRI) may be used to confirm the location and etiology of the nerve compression or check an alternative diagnosis.
- Nerve conduction studies (NCS) It used to check the velocity along the course of the nerve.
- Electromyography (EMG) may identify the presence of denervated muscles, showing the absence or reduction of motor unit recruitment during voluntary movement, and also check the nerve electrical activity.
- Electrodiagnostic studies (NCS and EMG) should be done after 10–21 from a peripheral nerve injury. EMG abnormalities at the biceps brachii and brachialis and coracobrachialis muscle depend on the location of the lesion.
- Magnetic resonance imaging (MRI) is useful in checking the specific muscle denervation patterns and localizing entrapment or compressive neuropathies.
- Magnetic resonance neurography (MRN) can give results of a nerve abnormality, nerve entrapment or impingement lesions, diffuse peripheral nerve lesions, neuropathy symptoms, or exclude a neuropathy diagnosis by showing normal nerves and muscles.
Differential diagnosis of musculocutaneous nerve injury :
- Biceps tendon injury or rupture
- Strain or tear of the biceps or brachialis muscles
- C5 or C6 radiculopathy
- Brachial plexus injury
Treatment of musculocutaneous nerve injury:
Medical treatment:
Once the diagnosis of musculocutaneous neuropathy is confirmed, treatments include relative rest, non-steroidal anti-inflammatory drugs, splinting, and physical therapy. If the conservative treatment is not successful, surgical decompression treatment is required to decrease that symptom.
In cases of musculocutaneous nerve injury, some people experience spontaneous recovery, It takes several months for the recovery period.
Surgical treatment:
In surgical procedures nerve, grafting or nerve transfer may be necessary for restoring function.
Surgical decompression is indicated as first-line treatment if there is paresthesia or numbness as this suggests that the affected nerve still has some function.
Physiotherapy treatment:
- Electrical stimulation.
- Electro modality to relieve pain if present such as TENS.
- Manual active exercise
- Strengthening exercise
- Massage therapy
- Low-level Laser therapy.
- Relation technique.
- Acupuncture.
- Sensory reeducation.
- Kinesio taping and Neural gliding.
Pain management:
Neuropathic pain affects the patient’s quality of life. Complete relief of the neuropathic pain by the modality is rarely but 40-60 % means partial relief to the patient. Anticonvulsants and tricyclic anti-depressants are the most commonly used for neuropathic pain.
A Physiotherapist can help to decrease pain by exercising, improving mobility, and improving muscle strength. for pain relief the techniques are the following:
Massage help manages neuropathic pain and improves the quality of life of the patient. Many different massage techniques are given to patients according to their condition and symptoms for pain relief or to reduce the spasm. pain management and QOL.
Trans cutaneous Electrical Nerve Stimulation (TENS) applies the TENS over the pain area to reduce the pain. 100 Hz in constant mode is beneficial to reduce the pain.
Low-Level Laser Therapy (LLLT) is beneficial in pain relief and acceleration of healing of tissue in the affected part.
Active exercise:
The musculocutaneous nerve is supplied by the flexor muscle of the upper arm so which allows the elbow flexion movement. If the nerve is injured therefore the movement is restricted.
The therapist first checks the movement. Then start the exercise in a patient in the supine position. The therapist did the exercise starting with passive movement and gradually going for the active assisted then the active movement in a full range of movement.
Passive movement is required when the muscle is completely paralyzed. once the actively full movement is achieved then go for the strengthening exercise.
Strengthening exercise:
For example strengthening exercises of elbow flexion movement start with graded weight progression, open-close chain exercise, and movement done with the use of send bags or different weight of dumbbells. Treatments are the following:
- The patient is in the supine position.
- Bring weight into the palm start with low weight, and progressively weight increases.
- The therapist asks the patient to do an elbow flexion movement.
- The therapist observes whether the patient completes the whole movement easily or not.
- Done this movement 5 to 7 repetitions and then gradually increase it.
- In progression, done this movement with a holding period.
Splint:
Static and dynamic splints can help to rest paralyzed muscles in one position so that avoid overstretching and or contractures developed. It also assists in allowing unaffected muscles to heal or operate in correct positions.
Sensory reeducation:
Sensory reeducation is necessary for the recovery of sensibility. Sensory reeducation devices are pinching and tapping, brushing, and icing. Used by this device gave the stroke to the patient over the affected part, and the stroke was given from the bottom to the upward direction. It did for the 20 to 30 repetitions or 5 mins.
Electrical stimulation:
First check the RD TEST of that muscle which is supplied by the musculocutaneous nerve, if the muscle is in 0 grade give the first IG current to stimulate the muscle. When muscle strength is improved then gradually go for the SF current. During the period of both current intervals check the SD curve to check the nerve progression.
Kinesio tapping:
An example of the biceps muscle is that pain can occur from a number of causes including muscle tears, nerve impingement, ligament or tendon injury, or swollen lymph nodes. Lifting heavy objects, repeated strain or trauma on the muscle and tendons.
Kinesio Tape can help to relieve the pain in the bicep by relaxing a damaged muscle, increasing blood flow, or relieving pressure off the area.
One strip of KT tape is applied over the biceps muscle from shoulder to 5 cm above the elbow. It applies one hour before the start of the activity.
FAQ
Which muscles do the innervate by the musculocutaneous nerve?
The musculocutaneous nerve supplies the main three muscles of the anterior compartment of the arm: the coracobrachialis, biceps brachii, and brachialis. It also supplies the lateral part of the forearm by the lateral cutaneous nerve.
What is the root value of the musculocutaneous nerve?
The musculocutaneous nerve arises from the lateral cord of the brachial plexus and the root value is ventral rami of C5, C6, and C7 of the spinal cord.
What is the function of the musculocutaneous nerve?
The musculocutaneous nerve is a peripheral nerve in your outer arm. It’s the terminal branch of the lateral cord, and part of the brachial plexus that extends from neck to armpit. The musculocutaneous nerve gives both motor function (movement) and sensory function (feeling).
Coracobrachialis – flexion and adduction of the glenohumeral (GH) joint and stabilize the humeral head in the glenoid fossa.
Brachialis– flexion movement of the elbow joint.
Biceps Brachii– It helps to stabilize the glenohumeral joint when elbow flexion and supination movement do with the weight.
Sensation to the front half of the upper arm, from the elbow to the base of the thumb, and to the front part of the lateral part from elbow to wrist.What nerve causes bicep pain?
The brachial plexus is a bunch of nerves that give sensation and movement in the neck, arm, and hand. Injury to the musculocutaneous nerve, which runs down the arm, can result in pain and weakness in the biceps muscle.
What are the causes of musculocutaneous nerve damage?
The causes of musculocutaneous nerve injuries include biceps tendon injury or rupture, strain or tear of the biceps or brachialis muscles, C5 or C6 radiculopathy, brachial plexus injury, direct trauma to the nerve., Repetitive, jerky upper extremity activity, etc.