Alcock canal syndrome: Cause, Symptoms, Diagnosis, Treatment, Exercise
When the Pudendal nerve is compressed in Alcock’s canal of the pelvis region is called Alcock canal syndrome also called Pudendal nerve entrapment syndrome (PNE). It rarely occurs in which chronic neuropathic pain in the distribution of the pudendal nerve mainly increased in sitting positioned with genital numbness and bladder-bowl incontinence are the major symptoms.
There are several variations of pudendal nerve entrapment, based on the location of compression of the nerve anatomically. it is called pudendal neuralgia in various medical journals. It highly affects your quality of life mostly because the pain comes and goes and it can make it hard to use the bathroom, disturbed your sex life, or even sitting position is painful.
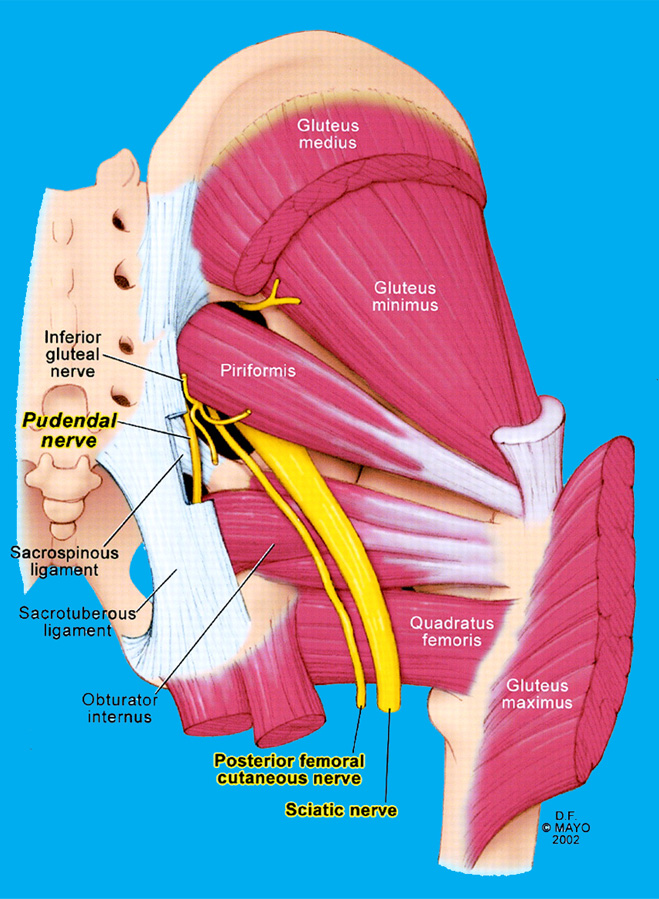
The pudendal nerve travels from the back of the pelvis to near the base of your penis or vagina, where it gives branches into other nerves. The Sacrotuberous Ligament originates from the Ischial Tuberosity and inserts onto the sacrum and the coccyx while the Sacrospinous Ligament is located at 90 degrees to it, deep to the Sacrotuberous Ligament, and attaches to the Ischial Spine. The thickness of these ligaments could result in compression of the Pudendal Nerve, also called Alcock Canal Syndrome or Cyclist Syndrome(Pudendal Nerve compression in Alcock’s canal.).
It mostly occurs mainly due to prolonged sitting position mainly on the bike, extreme cycling, or falls on the buttock region. These symptoms may increase with the sitting position, while standing and supine positions will relieve the symptoms.
Table of Contents
Anatomy of The pudendal nerve
The pudendal nerve is a major nerve in your pelvic area, which is paired nerve, which means there are two nerves, one is located on the left while another one is situated on the right side of the body.
This nerve work as motor function and sensory information to your genital area. This nerve passes through your pelvic floor muscles that support organs and ends at your external genitalia.
Nerve roots – S2-S4
Sensory function– innervates the external genitalia of both sexes and the skin around the anus, anal canal, and perineum
Motor function– innervates various pelvic floor muscles, the external urethral sphincter, and the external anal sphincter.
Autonomy function – carries sympathetic nerve fibers to the skin of the S2-S4 dermatomal region.
Pudendal nerve compressed at various levels such as the ischial spine, sacrospinous, and sacrotuberous ligament, Alcock’s canal which may lead to disabling, chronic, and intractable pelvic pain that is particularly variable and complex as it is also combined with multiple, perplexing functional symptoms.
Pathophysiology of Alcock canal syndrome
The nerve dysfunction and damage are mostly dependent on its cause.
Alcock canal syndrome can be on one side or both sides (unilateral or bilateral)
The most common causes of nerve Entrapment are overstretching, direct trauma, and positional. It is a functional entrapment where pain occurs during compression or during the stretch maneuver. The symptoms worsen due to repetitive micro-trauma resulting in continuous pain and related dysfunctional symptoms. The pudendal nerve is mostly compressed during long sitting and cycling.
This nerve is also Stretch during constipation and childbirth straining with constipation and childbirth. Over exercises, labor work with machines, weight lifting with squats, leg presses or karate with kickboxing and rollerblading are all the causative factors.
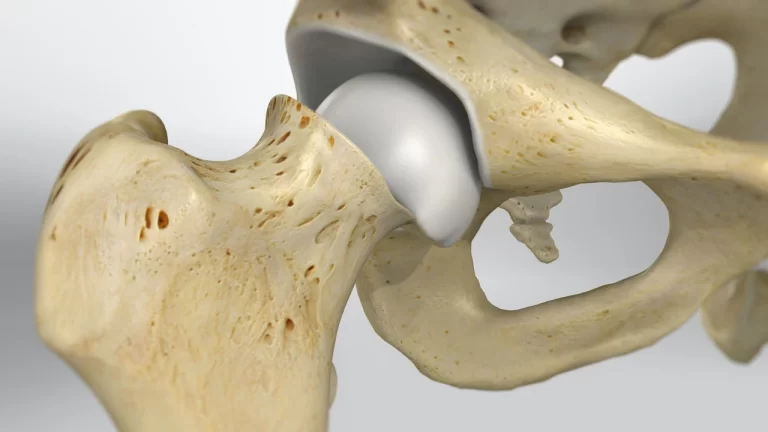
Sportsman with jerky activity is also a risk factor, mainly due to bony remodeling of the ischial spine. Long driving on rough roads or farm fields causes micro-trauma. Falls onto the pelvis region can cause pudendal nerve injury.
Causes of Alcock canal syndrome:
The most common causes are:
- Prolonged sitting or cycling position
- Post operative surgical scarring
- trauma to the pelvis
- pregnancy- delivering larger than average babies can cause nerve compression
- childbirth
- anatomic abnormalities
- Overstretch exercise
- surgical procedures that involve this area, such as a cesarean section, can cause nerve injury
- Professional cyclists, mainly due to both the compression and stretching of the pudendal nerve for prolonged time – if marathon cyclist used an inappropriately shaped or incorrectly positioned bicycle seat, may leads to thicken the sacrotuberous and/or sacrospinous ligaments and puts pressure on the nerve between them, resulting in PNE.
- Anatomic variations can result in nerve compression due to the pudendal nerve being fused to different parts in the pelvis and leads nerve being compressed between the sacrotuberous and sacrospinalis ligaments.
Alcock canal syndrome Symptoms:
The most common symptoms are gluteal pain which increases during sitting position throughout the day and relieves with standing or supine lying down, sexual dysfunction, and difficulties with urination and/or bowl. To confirm pudendal neuralgia, the Nantes criteria are used. The referred pain along the nerve distribution area.
Tingling numbness with burning sensation particularly in sitting position or cycling, less severe pain or relief in standing or supine lying position.
Initially, the nerve is compressed during the sitting position only so pain and other symptoms may be seen only with a long sitting position only, but as nerve entrapment increases, pain and related symptoms become more continuous and severely aggravated by sitting.
Many patients are not able to take sitting positions. However, few patients show that pain is relieved during sitting on a toilet seat, which is mainly due to pressure on the nerve is relieved to the ischial tuberosities rather than to the pelvic floor muscles. The pain and symptoms are usually progressively worse through the day due to activity and are relieved with rest.
In male cyclists sportsmen, it is mostly called “cyclist syndrome”, in which cyclists gradually develop recurrent tingling numbness of the penis and scrotum after prolonged cycling, or an altered sensation of ejaculation, with difficulties of urination and reduced awareness of defecation.
Pudendal nerve syndromes, related symptoms such as genitalia numbness, are amongst the most common bicycling associated urogenital problems.
Diagnosis of Pudendal Neuralgia:
For Doctors Pudendal nerve entrapment is difficult to diagnose, However, They ask you about the history of pain, also check you Physically and perform examination tests to differentiate from other conditions.
Pudendal neuralgia can be diagnosed through a proper history and physical examination if required also prescribed imaging studies such as MRI or CT Scan.
Diagnostic criteria developed by Robert Nantes are highly used. Five important criteria that help the diagnosis are:
pain along with the innervation of the pudendal nerve
pain increase in long sitting position or cycling
pain relieves in sleep or during a standing position
no objective sensory defects
a positive effect of anesthetic pudendal nerve block
This criterion is also helpful to determine the function of a patient at the start of treatment. Once treatment has started, the same criteria can be used to examine the progress and treatment effectiveness.
Physical examination also focuses on a simple pudendal neurological assessment. Pinprick sensation is tested at each branch at both sides: dorsal nerve (clitoris and glans penis), perineal nerve (posterior labia and posterior scrotum), and inferior anal nerve (posterior perianal skin).
Tingling numbness and pain is more common than loss of sensation. During an examination, Pressure is placed on the nerve at the Alcock canal and medial to the ischial spine to see the related symptoms such as pain, bladder, or rectal symptoms—the Valleix phenomenon.
MRI (Magnetic resonance imaging) allows, depending on the location of the nerve compression:
- Type 1, at the sciatic notch
- Type 2, at the ischial spine and Sacrosciatic ligament
- Type 3-a, the obturator internus muscle
- Type 3-b, the obturator internus and piriformis muscles
- Type 4, the distal branches of the pudendal nerve
Other Measurements that help are:
- Visual Analogue Scale (VAS)
- McGill Pain Questionnaire(MPQ)
- DN4 (which stands for Douleur Neuropathique 4)
- Brief Pain Inventory – Short Form (BPI-sf)
High-frequency ultrasonography also helps to identify the location of pudendal nerve compression. Doppler ultrasound help to detect vein compression, a result of nerve compression.
Imaging with MR neurography may be helpful. In people with one-sided pudendal entrapment in the Alcock’s canal, it is most helpful in the asymmetric swelling and hyperintensity affecting the pudendal neurovascular bundle.
Treatment of Alcock canal syndrome:
Medical treatment:
Most medical treatment is symptomatic pain-relieving medicine such as Analgesics (NSAIDs) are with Muscle Relaxants and rarely Anti-convulsants are prescribed.
Other various pharmaceutical treatments option for neuropathic pain is anti-epileptics (such as gabapenti), antidepressants (such as amitriptyline), and palmitoylethanolamide. In severe cases, polypharmacy is also used with the risk of side effects according to medication history.
Injections (Invasive) treatment options are:
Another treatment option is to identify and block the pudendal nerve pain is a “CT-guided nerve block.” In this procedure, “a long-acting local anesthetic injection such as bupivacaine hydrochloride and a corticosteroid (e.g. methylprednisolone) is injected to relieve immediate pudendal anesthesia.”
A pudendal nerve block injection can be inserted from various anatomical locations such as transvaginal, transperitoneal, and perirectal.
There is quick relief from pain and related symptoms after injection, however, there is a risk of side effects such as site irritation. It is also helpful in chronic pain mainly due to its direct effects on the nerve and helps to reduce inflammation. This treatment may relieve symptoms for up to 73% of people. However, the pudendal nerve block treatment option is rarely used by doctors mainly due to “discomfort associated with the local injections as well as the risk of injuring critical body parts.”
Physiotherapy treatment of Alcock canal syndrome:
Goal of treatment is to relieve pressure on the nerve and symptomatic pain relieving treatment.
Physiotherapist will take assessment of movement mainly Hip, Lower back and also examine flexibility of muscles located near gluteal area to identify any muscle tightness and poor movement pattern. Evaluation of pelvic muscles strength, posture and other symptoms are helps to make proper treatment plan.
Most commonly prescribed treatment option are:
- Symptomatic pain relieving modalities such as Interferential therapy(IFT), Transcutaneous electrical nerve stimulation (TENS), Ultrasound therapy helps to reduce neurogenic pain
- Stretching exercise of the tight muscles
- Strengthening exercise of weak muscles mainly pelvic floor muscles exercise
- Manual therapy
- correction of body Bio-mechanics, improve position or alternative activity modification
Pelvic Floor Relaxation exercises are the mostly used technique used by physiotherapists who mastered in pelvic floor dysfunction and disorders. In this mobilization of the sacro-iliac joints, with reducing the tension on the sacrotuberous and sacrospinous ligaments.
Exercises that helps to relive pressure on the pudendal nerve and will provide relief are:
Bridging exercise:

This exercise helps to Strengthens several core muscle groups – e.g buttocks, back, abs.
To do supine Lying position flat on back; keep bend knees at 90-degree angle, feet flat on the floor.
Tighten abs.
Raise buttocks off the floor, keeping abs tight.
Tighten buttocks. Shoulder to knees should be in a straight line.
Hold for a count of five. Slowly lower buttocks to the floor.
Repeat 5 to 10 times.
Superman position:
Starting position is prone .
Lie on the stomach with to the arms & legs stretched to the out.
Raise to the one arm & opposite leg is to the together.
Holding to this position for to the few seconds.
Then lower to the ground
Repeat this exercise of to the opposite side.
Side-lying hip abduction and extension
Starting position is the side lying
One leg is bend and other leg to raise .
It is called the abduction .
For the extension other leg is extended form the hip.
Hip extension in the quadruped position
Starting position is the quadruped position
Then the extended the leg form this position
Hold for the 10 second .
Repeat this exercise for the 10 times & 3 times per a day .
Back extension exercise (Cobra pose)
Starting position is prone .
Roll over to the stomach & place to the elbows right underneath onto the shoulders & hands are flat on to the ground.
Push down onto the hands & lift to the shoulders away from to the floor.
Hold the position for to the 30 seconds.
Do the 10 times in 1 session & perform 3 session per day .
Single Knee to Chest
You can start with Supine Lie on your back and bring one knee up to your chest. Hold for few seconds and then slowly return to the starting position.
Maintain relaxed breathing throughout the exercise. Repeat the above steps 8-10 times to each leg.
This is a great stretch for the hip, pelvis and lower back.
Piriformis stretching exercise

Take a supine lying position on your back and cross the right ankle over the left knee.
Grip the thigh of your left leg and take a deep breath in.
As you breathe out pull the knee in towards you. Hold the stretch for 10-30 seconds.
Repeat two times for each side.
Hamstring stretches:
Starting position is supine .
Lay on to the back.
Then bent to the one leg & one leg in to the air with to the stretch band around to the foot.
Hold for to this stretches 30 seconds.
Then repeat this stretch on to the other leg.
Do the 10 times in 1 session & perform 3 session per day .
Preventive measures:
This is a form of selfcare measures to relieve pressure on the pudendal nerve. It involves avoiding any activities that may increase pain and related symptoms in the pelvic area.
A cusion-seat with center part is opened is also recommended by doctor that helps to relive pressure on the nerve. Avoiding long sitting position or using sitting position with back is fully supported position that also reduced pressure on the gluteal region. You can also use wide sit during cycling to avoid recurrence of the symptoms. Marathon cyclist also advise to maintaining proper posture and fitness level.




One Comment