Quadrangular space syndrome:
Quadrangular space syndrome is characterized by compression or injury to the posterior humeral circumflex artery(PHCA), and the axillary nerve which is situated in the quadrangular space. So that may be the cervical radiculopathy, thoracic outlet syndrome, suprascapular nerve entrapment, and Parsonage-Turner syndrome.
Quadrilateral space syndrome(QSS) is a rare condition in which neural and vascular structures are entrapped in the quadrilateral space (QS).
Clinically tenderness is present over the quadrilateral space and teres minor atrophy. MRI investigation was used to check the axillary nerve compression.
This syndrome can also be caused by any type of injury, like a shoulder dislocation.
Table of Contents
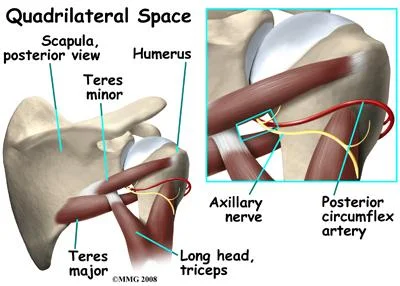
Anatomy of quadrangular space syndrome:
Quadrilateral space is present in the lateral to the triangular area and medial to the triangular interval.
Boundaries are the following:
- Superiorly – Teres minor muscles
- Inferiorly – Teres major muscles
- Medially – Long head of triceps brachii muscles
- Laterally – Surgical neck of the humerus
Contents:
- The axillary nerve.
- Posterior humeral circumflex artery.
These arteries are present in the quadrilateral space.
The axillary nerve supplies the teres minor muscle and deltoid muscle, which are primarily responsible for the abduction and external rotation movement. Characteristic fibrous bands are present in the quadrilateral space, which exacerbate symptoms, particularly pain, related to movements of the deltoid and teres minor muscles.
The anatomical differences in supplier patterns in the glenohumeral joint between patients can make it difficult to identify that pain is due to suprascapular nerve palsy or axillary nerve compression. Because the Posterior Humeral Circumflex Artery stretches around the neck of the humerus, repetitive tension and mechanical stress to the arterial wall can lead to thrombosis and aneurysmal degeneration.
Mechanism of injury:
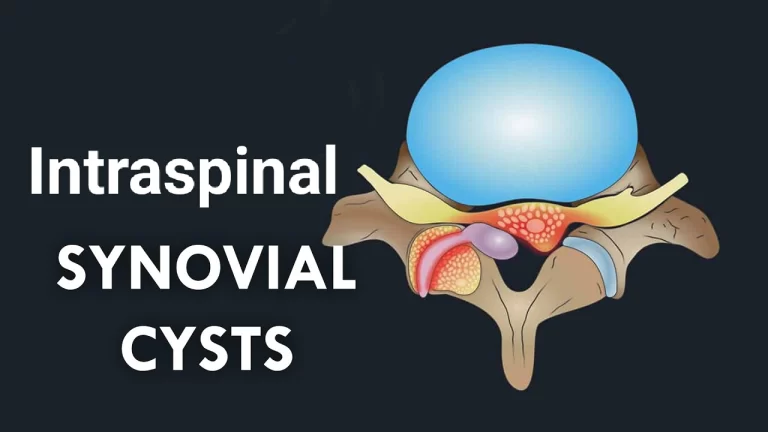
The exact mechanism and cause of the injury are unknown. However, it is often associated with overhead athletes like a pitcher, swimmers, or volleyball players who regularly use their arms in the position of abduction and external rotation. In this position more compression to the QS. Because of this, the dominant shoulder is mostly affected, and the syndrome is most common in active people aged 20-40. QSS can be caused by any reason that decreases the area of the quadrilateral space. It is caused by anatomical variations, a glenoid cyst, muscle hypertrophy, or paralabral cyst from any labrum injury.
Causes of QSS:
- Fibrous bands.
- Traumatic injury (scapular fracture).
- Paralabral cysts (inferior labral tear).
- Hypertrophied muscel.
- Benign or malignant mass.
Clinical presentation:
QSS typically occurs in young athletic adults between the age of 25 to 35 years without any history of significant trauma.
Symptoms:
- The pain is a dull aching or intermittent type. Pain is present in the posterior and lateral shoulder. These symptoms are aggravated by the active and resisted abduction and external rotation of the humerus. Pain can be worse at night
- Tenderness is present at the insertion site of the teres minor muscles.
- Atrophy or weakness is noted in the teres minor and deltoid muscles. Weakness is present in abduction and external rotation.
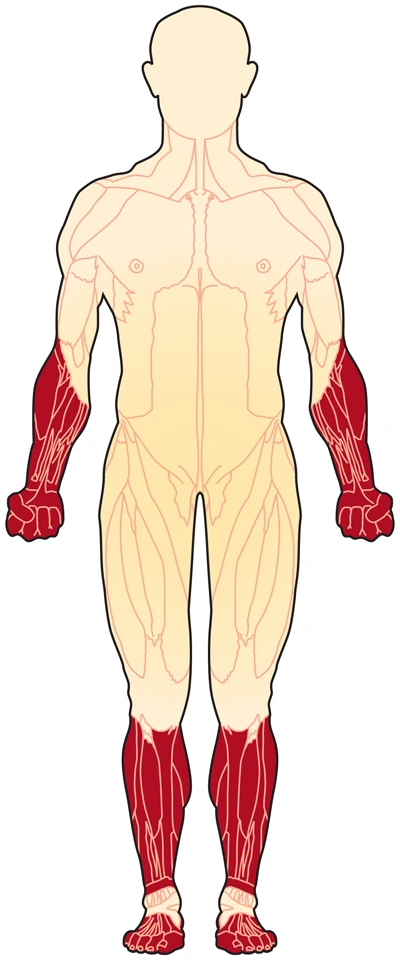
- Paresthesias are present in the sensory distribution of the axillary nerve, overlying the deltoid muscle in the lateral shoulder and upper posterior arm.
Signs:
Acute ischemia (pain, absent pulses), thrombosis, or embolism (coolness or cyanosis of the hand or digits). The patient has tenderness over the quadrilateral space. In severe condition thrombosis of the PHCA can block blood flow from the axillary artery, which cause embolization and subsequent cyanosis, digital ischemia, and cold intolerance.
Shoulder dislocation:
Quadrilateral space syndrome can happen 10 to 60 % time after a dislocation of the shoulder. There is a high risk depending on the type of dislocation. A blunt force injury on the back of the shoulder can cause quadrilateral space syndrome.
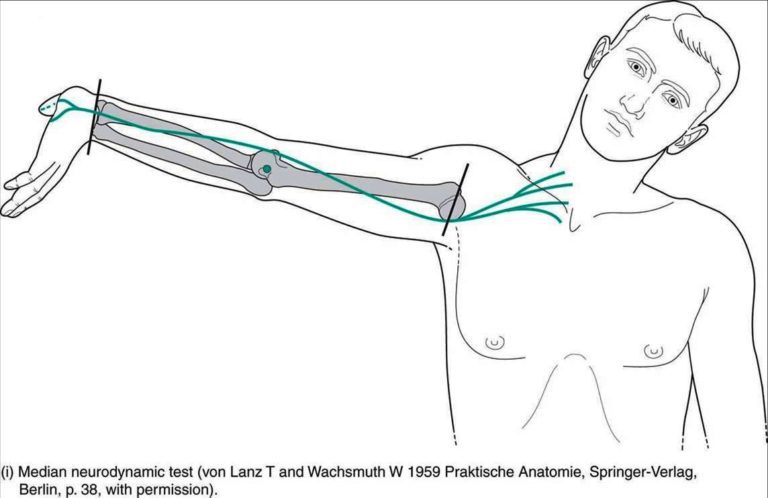
Physical examination:
- Atrophy of the teres minor and deltoid.
- Tenderness over the quadrangular space.
- Movement and strength: External rotation weakness with the arm abducted in the throwing position.
- Pain: Pain aggravated by active and resisted abduction and external rotation of the arm.
- Neurological examination: Mild sensory changes in the axillary nerve distribution.
Radiological examination:
X-ray:
X-rays should be performed to diagnose the pathological changes.
MRI:
Atrophied muscles can be identified by the MRI, which is a positive indicator of the syndrome. Compression of the QS can dependent on the position. (abduction and external rotation).
Arteriogram:
It may show a lesion in the posterior circumflex humeral artery.
EMG:
It shows axillary nerve involvement.
Differential diagnosis:
- Parsonage-Turner syndrome
- Suprascapular nerve compression at the spinoglenoid notch.
- Thoracic Outlet Syndrome
- Cervical Radiculopathy
- Rotator Cuff Pathology
- Internal/Posterior Shoulder Impingement
- Glenohumeral Instability
- Brachial Plexus Injury
Treatment:
Non-operative treatment:
In most cases, symptoms of quadrilateral space syndrome will improve with nonsurgical treatment.
There are different three degrees of nerve injury:
Most commonly, injury to the axillary nerve is a mild form of injury it’s called neuropraxia. It is recovered fully. The axillary nerve is very small, so even a severe injury can heal faster.
- NSAIDS such as ibuprofen.
- Heat or cold packs are applied on the shoulder.
- Physiotherapy treatment- It helps to maintain the shoulder’s range of motion or flexibility. The therapist should change the way a person does overhead sports activity when overuse is a possible cause.
- Posture correction training.
Outcomes:
Most people recover in 3-6 months of nonoperative treatment.
Diagnostic lidocaine block:
It will help to confirm the diagnosis.
Technique:
Plain lidocaine was directly injected into the quadrilateral space.
The starting point is 2 to 3 cm inferior to the posterior shoulder arthroscopy portal.
In minor symptoms, little weakness is present and no significant mass lesion in MRI. Rehabilitation and functional strengthening program can give result in improvements over a few months.
For weakness and functional disability, surgical decompression is necessary. Parlabral cysts can be approached arthroscopically and the labral tear repaired. Other large mass lesions require open surgical excision.
Operative Treatment:
Nerve decompression.
Indications:
Failure of nonoperative management.
Significant weakness and functional disability.
Decompression of space-occupying lesion.
Techniques:
Open release of quadrilateral space or arthroscopic repair of labral tear.
Extra fibers in the quadrilateral space usually compress the axillary nerve or the small artery or vein. These extra fibers are removed during decompression surgery. It is minor effective.
Due to high-energy trauma, or during surgery, the axillary nerve may be over-stretched or may be cut. It is known as neurotomesis.
The axillary nerve may be repaired. The injured portion of the nerve is replaced with another nerve. This is known as a nerve graft.
Post-surgical Rehabilitation:
Post-surgical shoulder rehabilitation includes three phases:
Phase I: Goals are to decrease the pain, and allow a range of motion at the shoulder. Start with gentle shoulder mobility exercises to keep scar tissue repaired. This also keeps the nerve and blood vessels moving freely. During the first four weeks not to overuse your arm after the surgery. Physical Therapists may also focus on posture correction exercises.
Phase II: It starts the gentle strengthening of the shoulder and upper limb. Whole-body conditioning is also important. Physical Therapists may recommend that ride a bike, walk on a treadmill, and strengthen the core muscles in your trunk.
Phase III: This phase usually starts six weeks after surgery, although the time for surgery is different for each patient. This includes sport-specific exercises, activities, functional activities, and regular strengthening-conditioning exercises.
The doctor may suggest doing the EMG test at monthly intervals to see if the axillary nerve is improving or not after surgery of the nerve grafting. By twelve weeks, the patient should have a full range of motion of the shoulder with good pain control. As in non-operated rehabilitation, the time required for return to different sports activity.
Physiotherapy treatment:
The therapist should take a detailed history, examination of active and passive movement of the shoulder, cervical spine, and thoracic spine, neurological examination, and special tests are checked. Once the diagnosis has been confirmed conservative treatment and physiotherapy are advised. There is no strong evidence to support specific physiotherapy treatments for Quadrengular Space Syndrome.
The physical Therapist’s goal is to help the patient’s pain under control, improve the range of motion, and improve strength and control in the shoulder. When a patient has recovery is well under way, regular visits to a therapist will end.
Physiotherapy treatment is focused on the following treatment:
- Optimizing the biomechanics of the shoulder by scapular stabilization and rotator cuff strengthening,
- Manual therapy to improve joint mobility.
- Use the modalities like electrical stimulation.
- Soft tissue release and transverse friction massage.
- Glenohumeral joint mobilization for tightness in the posterior capsule.
- Given the IR releases the soft tissue and enhances the healing process.
- Spinal manipulation to the cervical and thoracic spine.
- Scapular stabilization.
- Rotator cuff strengthening exercise.
Electrical muscle stimulation (EMS):
Electrical stimulation is necessary when muscle weakness or muscle wasting is present. This modality gives electrical current to the muscles to make them contract the muscle. It will help to maintain strength and decrease the wasting of the muscle.
Recovery times are different for each patient. In most cases, you can expect to do the whole movement, and be able to do the activity in 12 weeks.
Time required for back-to-sports activity.
Prognosis:
Long-standing cases often cause atrophy/weakness of teres minor and deltoid.
FAQ:
Why is the quadrangular space clinically important?
It is clinically important because the neurovascular structures pass through the quadrangular space and it is important for upper extremity function if it is damage that can cause disturbing the neurovascular symptoms.
What runs through quadrilateral space?
The axillary nerve and the posterior circumflex humeral artery run in the quadrilateral space.
Which muscles are innervated by the axillary nerve?
The axillary nerve gives motor and sensory distribution to the muscle. It has motor fibers that supply the deltoid muscle, which acts as an abductor, flexor, and extensor at the shoulder joint, also the teres minor muscle, which allows the lateral rotation of the glenohumeral joint.
Where is the quadrilateral space?
Quadrilateral space syndrome (QSS) is a rare condition in which neural and vascular structures are entrapped in the quadrilateral space (QS). This space is formed by the lateral head of the triceps, teres minor, teres major, and medial border of the humerus.
What are 3 facts about quadrilaterals?
A quadrilateral means a polygon ( 4 sides and 4 corners).
The word ‘quadrilateral’ arrived from ‘quad’ meaning ‘4’ and ‘lateral’ meaning ‘of sides’. So quadrilateral means 4 boundaries.
quadrilateral space The interior angles have 360 degrees.
Any quadrilateral with 4 right angles is a rectangle.