Raynaud’s Disease
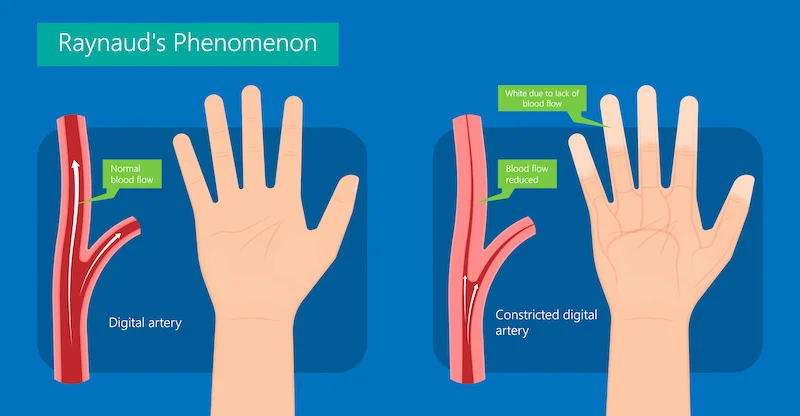
- Raynaud’s syndrome causes spasms in little blood vessels in your fingers and toes. This limits blood flow and you feel symptoms like skin color changes, cold skin, and a pins and needles sensation.
- The usual triggers of Raynaud’s attacks include cold weather and stress. Many people have small symptoms that they can manage through lifestyle changes.
Table of Contents
What is Raynaud’s syndrome?
- Raynaud’s (pronounced ray-nodes) syndrome is a disorder that affects little blood vessels in your fingers and toes. It may also harm blood vessels in your nose, lips, or ear lobes. Raynaud causes you to have episodic spasms, known as vasospastic attacks, in response to cold temperatures or stress.
- During a Raynaud’s attack, the arterioles & capillaries in your fingers and toes stiffen more than they should. As a result, the skin in the affected part turns white and then blue. This color change occurs because your blood lacks oxygen. Your skin may feel cold or numb. As your blood vessels relax and uncover again, your skin may look red or feel tingly. An attack commonly lasts around 15 minutes.
What are the different types of Raynaud’s syndrome?
There are 2 main types of Raynaud’s syndrome:
- Primary Raynaud’s syndrome (also called Raynaud’s disease).
- Secondary Raynaud’s syndrome (also called Raynaud’s phenomenon).
- The chart lower lists what you should know about each type.
What is the various between Raynaud’s disease, Raynaud’s phenomenon, & Raynaud’s syndrome?
Most people utilize these terms interchangeably. Yet scientists use them to distinguish between primary and secondary forms of the condition.
- Raynaud’s disease: Occurs on its own and is not connected with another disease or condition. This is also known as primary Raynaud’s syndrome.
- Raynaud’s phenomenon: This happens due to an underlying condition, medication, or lifestyle factor. This is known as secondary Raynaud’s syndrome.
- Raynaud’s syndrome: Touch to either the primary or secondary form of the condition.
Is Raynaud’s syndrome serious?
- Primary Raynaud’s syndrome is not severe and does not damage your blood vessels. It may disrupt some of your daily activities, but it is not dangerous.
- Secondary Raynaud’s syndrome can be more severe. It may conduct to skin ulcers &, rarely, tissue death (gangrene). It may impact your quality of life. The underlying disease causing it may be serious in and of itself.
Whom does Raynaud’s syndrome affect?
Primary Raynaud’s syndrome commonly affects:
- People assigned female at birth,
- People under the age of 30, sometimes starting in their teenage years,
- People who have a family study of Raynaud’s disease,
- Secondary Raynaud’s syndrome commonly affects people who have another disease or condition.
- It can also injure people who perform a job that puts repetitive pressure on their hands.
Here are certain facts to know:
- About 9 (nine) in 10 (ten) people with scleroderma have Raynaud’s phenomenon. This may be the scleroderma symptom they have had for many years.
- About 1 (one) in 3 (three) people with lupus have Raynaud’s phenomenon.
- People with autoimmune conditions, especially connective tissue diseases, are at greater risk of Raynaud’s.
- People who use hand tools that vibrate (such as jackhammers or chainsaws) face a greater risk of Raynaud’s phenomenon. The condition is also more usual in pianists and keyboard operators.
How common is Raynaud’s syndrome?
- Raynaud’s syndrome is usual. Estimates vary, yet Raynaud likely harms up to 1 in 20 people in the U.S.
How does Raynaud’s syndrome affect my body?
- Raynaud’s syndrome is an exaggerated version of a normal body process known as the vasomotor response. Vasomotor response means your blood vessels open up (vasodilation) and tighten (vasoconstriction) to assist your body respond to its environment.
- For example, if it is cold outside, blood vessels close to your skin’s surface and constrict to move blood to veins deeper in your body. This permits your body to conserve heat. Your blood vessels also constrict when you are stressed to help your body save oxygen.
- Raynaud disrupts this typical body process and causes your blood vessels to compress more than they should. This interrupts your typical blood flow and limits the oxygen available to your fingers or toes.
How does Raynaud’s disease affect my heart?
- Primary Raynaud’s syndrome does not affect your heart. Yet conditions associated with secondary Raynaud’s syndrome may harm your heart. Talk with your healthcare provider (doctor) to learn if your condition harms your heart.
What are the symptoms of Raynaud’s syndrome?
Raynaud’s symptoms affect your skin and may involve:
- Color changes. As blood flow stops and then returns, your skin color may exchange from white to blue to red. Some people do not experience all three changes in skin color.
- Feeling cold or numb. This occurs when your finger or other affected body part is not receiving oxygen-rich blood. It feels as if part of your body has “fallen asleep.”
- Feeling warmth, tingling or throbbing: This occurs as blood flow returns to your affected body part.
- Skin ulcers and gangrene: Longer or more frequent attacks may conduct in painful sores on your fingertips. These sores can take away a while to heal. Rarely, lack of oxygen to your tissues may conduct to tissue death (gangrene).
- Symptoms of Raynaud’s syndrome are episodic. That means they come and out. A usual episode, or attack, lasts about 15 minutes. Yet attacks may be shorter or longer. Episodes are often associated with some triggers such as cold weather. Symptoms are commonly mild in people with primary Raynaud syndrome. People with secondary Raynaud’s syndrome may have more serious symptoms, involving skin ulcers.
- Raynaud’s can cause your skin to change color shortly. It may first look white previous turning blue then red. Your skin may feel cold or numb at the beginning of an attack due to decreased blood flow. When blood flow returns, your fingers may feel the warmth or throb.
What triggers Raynaud’s disease?
Triggers that can lead to a Raynaud’s attack involve:
- Air-conditioned rooms or other cold spaces such as the frozen food aisle in a grocery store,
- Anxiety, emotional stress or excitement,
- Cold weather,
- Holding a glass of iced water or other cold drinks,
- Reaching into the freezer,
- Sweat that cools on your skin.
What causes Raynaud’s syndrome?
- The primary Raynaud’s syndrome has no identifiable underlying cause.
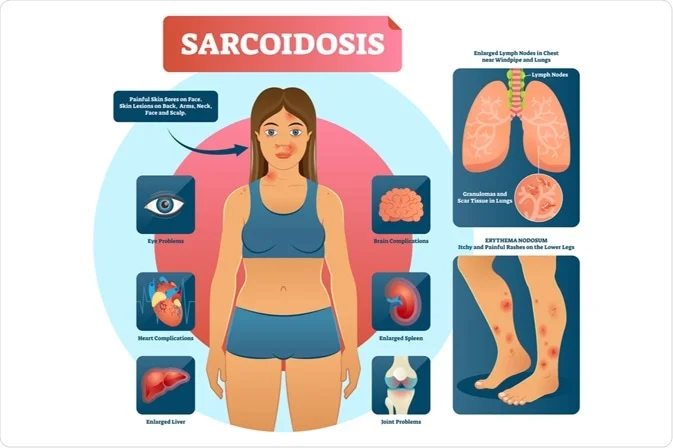
- An underlying disease or condition commonly causes secondary Raynaud’s syndrome (Raynaud’s phenomenon). It is especially usual in people with connective tissue diseases. Some of these diseases decrease blood flow to your fingers and toes.
- Other causes involve repetitive motions and some medications. The lists break down the many causes of Raynaud’s phenomenon.
Diseases & conditions that can cause Raynaud’s phenomenon
- Buerger’s disease (especially in the people assigned male at birth who smoke),
- Cancer
- Carpal tunnel syndrome
- Dermatomyositis
- Hypothyroidism
- Lupus
- Mixed connective tissue disease
- Peripheral artery disease (especially in the people assigned male at birth over age 50)
- Polymyositis
- Pulmonary hypertension,
- Rheumatoid arthritis,
- Scleroderma and CREST syndrome
- Sjögren’s syndrome
- Thoracic outlet syndrome
- Vasculitis.
Medications & substances that can because of Raynaud’s phenomenon
- Beta-blockers
- Caffeine
- Chemotherapy (bleomycin, vinblastine)
- Cocaine
- Decongestants containing phenylephrine or pseudoephedrine
- Epoxy resins
- Migraine medications containing ergotamine
- Nicotine
- Stimulant medications (like methylphenidate) treat attention-deficit/hyperactivity disorder (ADHD).
Other causes of Raynaud’s phenomenon
- Frostbite,
- Traumatic vasospasm from vibrating tools or recurrent pounding with the palm of your hand. This can involve playing the piano.
How is Raynaud’s syndrome diagnosed?
- Healthcare providers (doctors) can typically diagnose Raynaud’s syndrome from your symptoms. Your provider (doctor) may ask you to take photos of your skin changes when they happen. Your provider (doctor) may also perform a physical exam and talk with you about your medical and family history.
- Raynaud’s syndrome is commonly easy to diagnose. Yet it may not be obvious whether you have the primary or secondary form. That is where diagnostic testing can help.
What tests diagnose Raynaud’s syndrome?
- Several diagnostic tests can assist determine if you have primary or secondary Raynaud’s syndrome.
- One test that is particularly useful is a nail fold capillaroscopy. For this test, your provider (doctor) places a drop of oil on your skin at the base of your fingernail. This spot is known as your nail fold. Your provider (doctor) then looks at your nail fold under a microscope. If your capillaries in the part are enlarged or abnormal, you may have a connective tissue disease. This would indicate that you such as have secondary Raynaud’s syndrome.
Other tests your provider may order involve:
- Antinuclear antibody (ANA) test: A blood test that detects autoimmune diseases.
- Complete blood count (CBC): A blood test that detects a range of conditions.
- Erythrocyte sedimentation rate (ESR) test: A blood test that checks inflammation in your body. Assists diagnose rheumatoid and autoimmune disorders, among other conditions.
- Urinalysis: Urine test that detects a range of conditions.
- Pulse volume recording: Noninvasive test that detects blood flow in your arms and legs.
- Rheumatoid factor (RF) test: A blood test that detects autoimmune diseases.
- These tests can help your provider (doctor) identify or rule out underlying conditions as causes of Raynaud’s symptoms.
Who treats Raynaud’s syndrome?
You may receive care from healthcare providers (doctors) in different specialties. That is because Raynaud’s syndrome can affect your body in many ways. It can also outcome from a wide range of medical conditions. Providers who may assist with your diagnosis and treatment include:
- Cardiologists,
- Dermatologists,
- Primary care physicians,
- Rheumatologists.
What is the treatment for Raynaud’s syndrome?
- There is no cure for Raynaud’s Phenomenon (RP) but it can be managed with a proper and well-planned treatment based on the patient’s symptoms, age, severity, and overall health.
The treatment may involve:
- Avoiding exposure to cold,
- Retaining warm with gloves, socks, a scarf, and a hat,
- Stopping smoking,
- Wearing finger guards over fingers with sores,
- Avoiding trauma and vibrations to the hand (such as with vibrating tools),
- Taking blood pressure medicines during the winter months helps reduce constriction of the blood vessels,
- Patient education.
- The treatment involves medical therapy as well in form of antihypertensives, such as calcium-channel blockers (CCB) or sardines, and vasodilating agents, such as intravenous iloprost.
- Raynaud’s Phenomenon (RP) patients with no other symptoms than skin discoloration extremities may require only home-remedy measures to prevent complications.
The treatment turns on the severity of your condition and whether you have the primary or secondary form. Treatment goals involve:
- Cure Raynaud’s attacks,
- Help decrease the severity of attacks,
- Increase your quality of life,
- Treat with the underlying disease or condition (if you have secondary Raynaud’s),
- Cure skin ulcers and tissue damage.
For many people, lifestyle changes are enough to handle their condition. These involve:
- Avoid cold spaces (such as the frozen food aisle or extreme air conditioning),
- Avoid touching cold objects (such as glasses of ice water or cold metal surfaces),
- Manage stress & strong emotions that could trigger an attack,
- Wear warm clothes during cold weather.
However, if you have severe symptoms, you may require medication. Your provider (doctor) may prescribe one or more of the following medications:
- Calcium-channel blockers: These drugs assist your smallest blood vessels to relax and open up. As an outcome, you have fewer attacks, and those you do have are less severe. Calcium-channel blockers also can assist heal skin ulcers on your fingers or toes.
- Alpha-blockers: These drugs counteract norepinephrine. That is a hormone that constricts your blood vessels.
- Nitroglycerin skin ointment: This is a cream that you apply to your fingers to assist heal skin ulcers.
- If you have serious Raynaud’s and other treatment methods do not work, your provider may recommend a procedure known as a sympathectomy. A sympathectomy temporarily blocks or cuts small nerves near your affected blood vessels. This cures the nerves from sending signals that make your blood vessels get too narrow. The procedure should relieve your symptoms for one (1) or two (2) years, but you may require it again in the future.
Surgery
- If your condition does not improve after these steps and you are at risk of severe problems, such as losing parts of your fingers or toes, your doctor might consider surgery. These procedures include cutting the nerves to the blood vessels in your skin to limit how much they open and close. The doctor might inject drugs into your hands or feet to block those nerves.
Home Treatment for Raynaud’s disease
These steps can also assist you to control your condition:
- Avoid smoke: Do not smoke, and stay away from secondhand smoke, too. It can create your blood vessels close up, which lowers your skin temperature.
- Exercise: It will boost your circulation. If you have secondary Raynaud’s, check with your doctor previous you try an outdoors workout in cold weather.
- Manage stress: Keeping it under control could assist cut the number of attacks.
- Keep your temperature constant: Do not go straight from a chilly space to a warm space if you can help it. Keep away from the frozen-food section of the grocery store as much as possible.
- Dress for the cold: Have on layers, gloves, & heavy socks. Purchase chemical warmers for your pockets, gloves, & socks.
- Avoid some medications: Decongestants with phenylephrine, diet pills, migraine medications with ergotamine, herbal medications with ephedra, and the blood pressure (BP) medication clonidine (Catapres) can all little your blood vessels.
- Soak your hands: Or run warm water over them when you feel an attack beginning.
Can Raynaud Kill You?
- No, yet serious cases can cut off the blood flow to your skin and conduct tissue damage. A completely blocked artery can conduct skin sores (ulcers) or dead tissue (gangrene). It is rare, but if this happens, the doctor might have to remove a finger or toe.
How can I prevent Raynaud’s syndrome?
- There is nothing you can do to cure Raynaud’s syndrome. Yet you can assist prevent attacks by learning your triggers and taking action to avoid them.
- It is also main to visit your provider for yearly checkups. Doing so can assist your provider (doctor) diagnose and treat underlying conditions that may cause Raynaud’s phenomenon. Certain of these conditions are preventable with lifestyle changes, like avoiding tobacco products.
What can I expect if I have Raynaud’s syndrome?
- For most of the people with primary Raynaud’s syndrome, the outlook is positive. Symptoms may bother you off and on, yet the condition is not serious or life-threatening. Over time, you will learn more self-care tips for preventing attacks or helping them go away.
- If you have secondary Raynaud’s syndrome, your outlook turns on your underlying disease. Tell your provider (doctor) about what you can expect and how to manage your condition.
How do I take care of myself?
- Self-care is essential for managing Raynaud’s syndrome. Follow your healthcare provider’s (doctor’s) guidance on how to avoid triggers and how to manage an attack when it occurs. The following tips can also assist.
How to avoid Raynaud’s triggers
- Adjust your thermostat so your home and office are warm.
- Avoid caffeine.
- Avoid touching cold metals and putting your hands in cold water.
- Bring a jacket or sweater if you know the space will be cold.
- Do not go barefoot. Wear socks indoors, and wear 2 pairs of socks when going outside in the cold.
- Exercise regularly to increase your overall well-being. Check with your provider before beginning a new exercise plan.
- Retain your feet and hands dry and warm. Consider utilizing a disposable or rechargeable hand warmer.
- Retain your whole body warm, especially your hands, feet, and head. Wear so many layers of loose clothing. Do not forget mittens (warmer than gloves) and a hat.
- Learn current ways to manage stress in your life.
- Limit the use of tools (such as jackhammers) that vibrate.
- Limit your time in air conditioning and in cold spaces (such as the frozen foods aisle).
- Practice good skin care. Apply lotion to cure dry or cracked skin.
- Quit smoking (or do not start). Nicotine causes your skin temperature to down, which may trigger an attack. Talk to your healthcare provider (doctor) about ways to help quit smoking.
- Take rare breaks during the day to rub your hands together.
- Utilize a potation holder or insulating sleeve to hold cold drinks.
- Wear the oven mitts when you extend into your fridge or freezer.
- Wear cotton fabrics when you exercise to move sweat away from your skin.
- Also, it is main to know which medications can trigger an attack. Ask your provider (doctor) if any of your present medications could cause your condition to flare up.
These involve some medications that treat:
- ADHD
- Cancer
- Colds and nasal congestion
- High blood pressure
- Certain heart medicines
- Migraines.
How to manage a Raynaud’s attack
- If an attack does occur, be proactive. Do not ignore Raynaud’s attack or assume it will go away on its own. Taking the proper steps can decrease the length and severity of an attack.
Here is what to do:
- Immediately go to a warmer space
- Massage the affected part
- The motion of your arms in circles
- Put your hands below your armpits to warm them up
- Run warm (not hot) water above your fingers or toes
- Meditate or do deep breathing exercises if tension triggered your attack.
When should I see my healthcare provider?
Call your provider if you:
- Have attacks that happen on just one side of your body.
- Have sores and ulcers on your fingers or toes.
- Lose function in the harmed hand or foot.
- Notice new or worsening symptoms.
- Experience side effects from medications.
- As with any condition, see your provider any time you are worried, frightened, or have questions about how to care for yourself.
How can I assist my child manage Raynaud’s syndrome?
- Primary Raynaud’s disease sometimes begins during the teenage years. Rarely, it can start earlier. So, if your child or teen begins to have symptoms, take them to see their healthcare provider (doctor). Their provider (doctor) may want to go for tests to rule out an underlying condition.
- Typically, Raynaud’s in kids & teens is mild, and symptoms should simplicity as your child gets older. Similar management tips for adults also can assist your child. For example, dress your child warmly in cold weather (and give them 2 pairs of mittens to wear rather than just one). Retain your home and car warm, and avoid air conditioning that is too cold.
- It is also main to tell administrators at your child’s school about their condition. Your child may require special permission to avoid outdoor activities (such as gym class) during the colder months.
NOTE
- Raynaud’s syndrome is a usual condition that may affect your quality of life. Learning how to care for yourself at home can assist you to avoid and manage Raynaud’s attacks. If your symptoms are curing you from doing the things you love, talk with your provider (doctor) about treatment options. It may assist to connect with a support group to learn from others living with the same condition.
FAQs
Raynaud’s is typically triggered by cold temperatures, anxiety, or stress. The condition happens because your blood vessels go into a temporary spasm, which blocks the flow of blood. This causes the affected part to change color to white, then blue, and then red, as the blood flow returns.
Raynaud’s phenomenon is trouble that causes reduced blood flow to the fingers. In certain cases, it also causes decreased blood flow to the ears, toes, nipples, knees, or nose. This occurs due to spasms of blood vessels in those parts. The spasms occur in response to cold, stress, or emotional upset.
Calcium channel blockers are the class of drugs most widely used for the treatment of Raynaud syndrome—especially the dihydropyridines (eg, nifedipine, nicardipine), which are the most potent vasodilators. Nifedipine is the customary first choice.
Abnormalities of magnesium metabolism have been seen in people with Raynaud’s disease. Symptoms similar to those seen with Raynaud’s disease happen in people with magnesium deficiency, probably because a deficiency of this mineral results in spasms of blood vessels.
In very rare, severe cases, the loss of blood flow can cause ulcers or tissue death, but usually, Raynaud’s is not dangerous—it is just painful and frustrating.
Raynaud’s phenomenon, first described as cold-induced digital vasospasm, is a systemic disease with a multifactorial etiology, and vasospasms do not just affect the digits and skin, but also internal organs including the heart, lungs, and kidney.
Left untreated, Raynaud’s phenomenon can lead to gangrene (tissue death) in certain cases. Look up prompt medical care if you have symptoms of Raynaud’s phenomenon in the fingers or toes, such as unusual coldness, skin color changes, & the development of sores or lesions that do not heal.
Reduce exposure to cold or extreme temperature changes.
Wear extra warm clothing to protect yourself from the cold.
Quit smoking.
Limit caffeine and alcohol.
Exercise to improve blood flow, especially for primary Raynaud’s disease.
Avoid wearing clothing or jewelry that is very much tight.
Tests. A test called nail fold capillaroscopy can tell the difference between primary and secondary Raynaud’s. During the test, the provider uses a microscope or magnifier to see for anything unusual on the skin at the base of a fingernail. This might involve swelling of the blood vessels.
In rare cases, Raynaud’s can become severe. If it causes skin sores or gangrene—decay or death of body tissues—you may require antibiotics or surgery to remove the damaged tissue. In very severe cases, it might be necessary to remove the affected toe or finger.
There is no cure for Raynaud’s that happens on its own (primarily Raynaud’s). Yet you may be able to control it by avoiding the things that trigger it. Keep your body warm.
Secondary Raynaud is linked to diseases and conditions that directly damage the arteries. The disorder is also linked to diseases and conditions that harm the nerves that control the arteries in the hands and feet.
Raynaud’s phenomenon can happen on its own (primary Raynaud’s phenomenon), or it can be linked to another disease or condition (secondary Raynaud’s phenomenon). It can last from just a certain minute to many hours. Raynaud’s phenomenon does not usually cause permanent damage.




6 Comments