Polymyalgia Rheumatica
Table of Contents
What is Polymyalgia rheumatica?
Polymyalgia rheumatica is an inflammatory condition that causes muscle pain & stiffness, especially in the shoulders & hips. Signs & symptoms of polymyalgia rheumatica usually start quickly & are worse in the morning.
Polymyalgia rheumatica is widespread aching & stiffness. Symptoms tend to come quickly, over a few days or weeks, & sometimes even overnight. Both sides of the body are evenly involved. Involvement of the upper arms, with trouble raising them above the shoulders, is usual. Sometimes, aching occurs at joints such as the hands & wrists.
Achiness is always worse in the morning & improves as the day appears. Yet inactivity, such as a long car ride or sitting too long in one position, might cause stiffness to return. Stiffness might be so severe that it causes any of these problems:
Disturbed sleep-Trouble getting dressed in the morning (for instance, putting on a jacket or bending over to pull on socks & shoes) or even getting out of bed Problems getting up from a sofa or in & out of a car.
Most patients who develop polymyalgia rheumatica are older than 65. It rarely affects people under 50.
This disorder is related to another inflammatory condition called giant cell arteritis. Giant cell arteritis can cause headaches, vision difficulties, jaw pain, & scalp tenderness. It may have both conditions together.
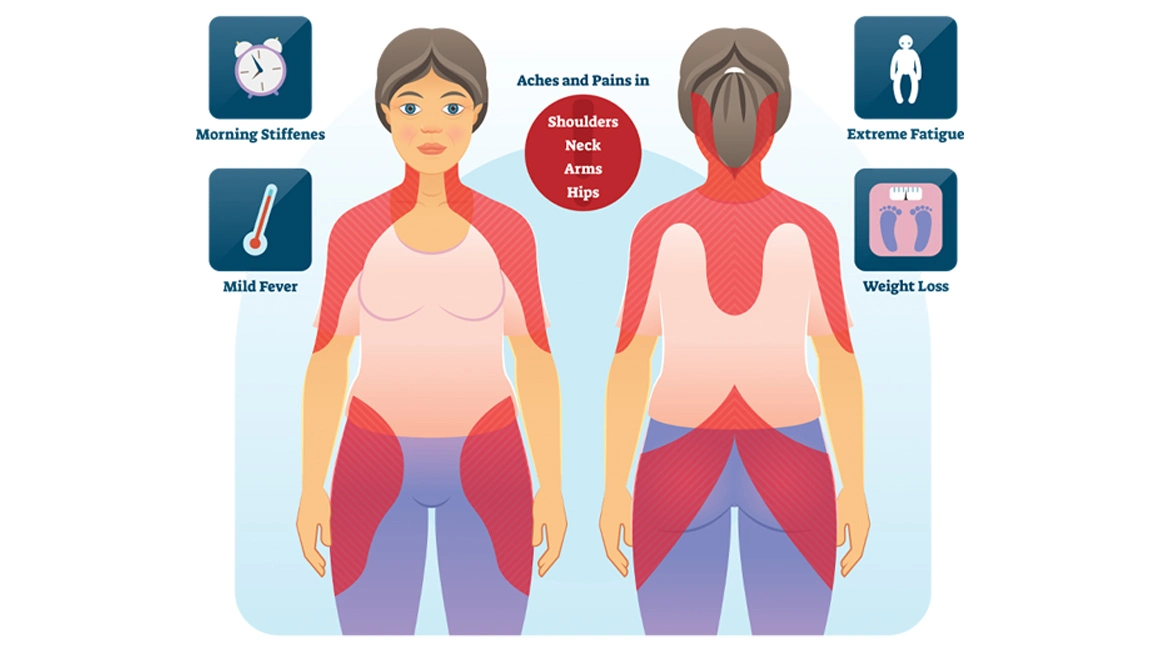
What are the symptoms of Polymyalgia rheumatica?
Pain & stiffness in the neck & shoulders is the most common symptoms of polymyalgia rheumatica.
The pain & stiffness might slowly spread to other areas, such as the shoulders, hips, & thighs. These symptoms generally affect both sides of the body.
Other common symptoms of polymyalgia rheumatica involve:
- fatigue
- malaise
- loss of appetite
- sudden, unintentional weight loss
- anemia
- depression
- Loss of appetite
- low-grade fever
- limited range of motion
The symptoms of polymyalgia rheumatica develop quickly, generally over several days. In some cases, the symptoms might appear overnight. They tend to be worse in the morning & gradually improve throughout the day.
- Aches or pain in the shoulders
- Aches or pain in the neck, arms, buttocks, thighs, or hips
- Stiffness in affected parts, particularly in the morning or after being inactive for a time
- Limited range of motion in affected areas
- Pain or stiffness in your wrists, elbows, or knee joint
Patients might find that being inactive or sitting in one position for a long period of time can make symptoms worse. The pain & stiffness might eventually become so severe that you have difficulty performing everyday activities, such as standing up from the couch, getting dressed, getting into a car, reaching, washing, climbing stairs, or even getting out of bed might be difficult. Sometimes, the symptoms of polymyalgia rheumatica can even make it hard to fall asleep.
What are the causes of Polymyalgia rheumatica?
The cause of polymyalgia rheumatica is not known. Nevertheless, it’s believed that certain genes & gene variations might increase your risk of developing it.
Environmental factors might also play a role in the development of the condition. New cases of polymyalgia rheumatic are frequently diagnosed in cycles & usually occur seasonally.
This suggests that there might be an environmental trigger, such as a viral infection, that causes the disorder. The rapid onset of symptoms also suggests that polymyalgia rheumatica might be triggered by an infection. Nevertheless, no such link has been found.
Familial aggregation of polymyalgia rheumatica has suggested a genetic predisposition. HLA class II alleles are found to be associated with polymyalgia rheumatica & among these, the HLA-DRB1*04 allele correlates most frequently, seen in up to 67% of cases. Genetic polymorphisms for ICAM-1, RANTES, & IL-1 receptors also seem to play a role in the pathogenesis of polymyalgia rheumatica in some populations.
There were reports of increased incidence of polymyalgia rheumatica along with Giant cell arteritis during epidemics of mycoplasma pneumonia & parvovirus B19 in Denmark suggesting a possible role of infection in etiopathogenesis. The Epstein-Barr virus (EBV) has also been proposed as a possible trigger for polymyalgia rheumatica. Nevertheless, several other studies have not supported an infectious etiology hypothesis.
There are also reports of an association between polymyalgia rheumatica & diverticulitis, which could suggest a role of a change in microbiota & chronic bowel inflammation in the immunopathogenesis of the disease.
A case series of previously healthy subjects developing Giant cell arteritis or polymyalgia rheumatica after influenza vaccination also exists. Vaccine adjuvants can trigger autoimmunity-causing autoimmune or inflammatory syndrome induced by adjuvants (ASIA) which can have clinical features similar to polymyalgia rheumatica.
Polymyalgia rheumatica & another disease known as giant cell arteritis share many similarities. Many patients who have one of these conditions also have symptoms of the other.
Giant cell arteritis results in inflammation in the lining of the arteries, most frequently the arteries in the temples. Signs & symptoms include headaches, jaw pain, vision problems, & scalp tenderness. If left untreated, this disease can lead to stroke or blindness.
“Myalgia” comes from the Greek word for “muscle pain.” Nevertheless, specific tests of the muscles, such as a blood test for muscle enzymes or a muscle biopsy, are all normal.
Recent research suggests that inflammation in Polymyalgia rheumatica involves the shoulder & hip joints themselves, & the bursae (or sacs) around these joints. So, pains at the upper arms & thighs, in fact, start at the nearby shoulder and hip joints. This is what doctors called as “referred pain.”
Polymyalgia rheumatica should not be confused with fibromyalgia, a different syndrome that unlike Polymyalgia rheumatica does not elevate typical markers of inflammation.
What are the risk factors of Polymyalgia rheumatica?
Risk factors for polymyalgia rheumatica involve:
- Age. Polymyalgia rheumatica affects older adults almost exclusively. It most frequently occurs between ages 70 & 80.
- Sex. Women are about two to three times more prone to develop the disorder.
- Race. Polymyalgia rheumatica is most usual among white people whose ancestors were from Scandinavia or northern Europe.
What are the complications of Polymyalgia rheumatica?
Polymyalgia rheumatica symptoms can interfere with the patient’s everyday activities, especially if the condition goes untreated.
Without appropriate treatment, the pain & stiffness can severely decrease your mobility. the patient might eventually be unable to complete simple tasks on their own, such as bathing, getting dressed, & combing their hair.
Some patients also experience a temporary loss of joint function. This increases your risk of developing lingering joint problems, such as a frozen shoulder.
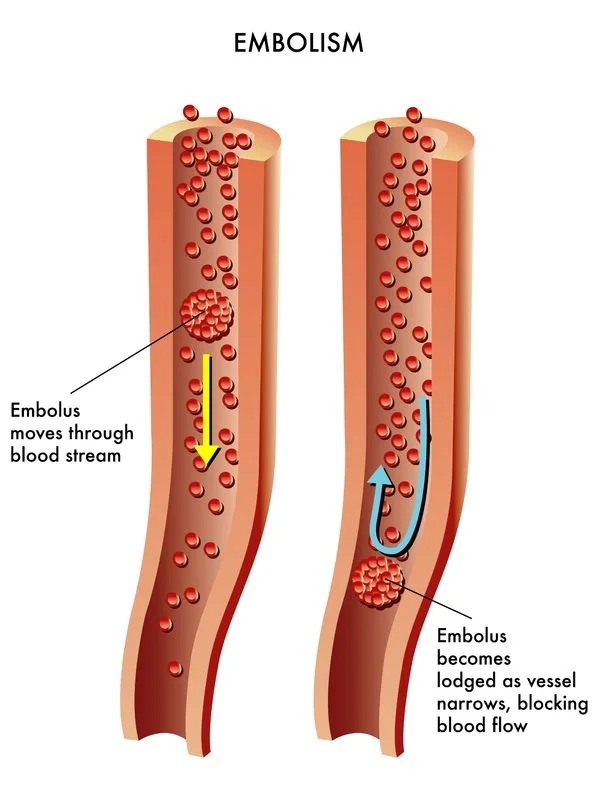
Patient with polymyalgia rheumatica is also more likely to develop peripheral artery disease. This condition impairs blood circulation & frequently causes leg pain & ulcers.
Polymyalgia rheumatica patients have an elevated risk of cardiovascular diseases. Premature atherosclerosis outcoming from chronic inflammation is the most likely cause of premature Coronary artery diseases.
Cancer association with Polymyalgia rheumatica is not entirely clear. In a study of the increased risk of lymphoplasmacytic lymphoma – Waldenstrom macroglobulinemia correlated with polymyalgia rheumatica with an OR of 2.9.
Polymyalgia rheumatic patients have higher chances of developing inflammatory arthritis. Features of small joint synovitis, younger age, & positive anti-CCP positivity in patients with Polymyalgia rheumatica were found to have an association with the risk of developing inflammatory arthritis.
What is the differential diagnosis of Polymyalgia rheumatica?
Polymyalgia rheumatica has nonspecific signs and symptoms that many other conditions could mimic. Other entities should be excluded from the investigations, as deemed needed by clinical suspicion, before diagnosing Polymyalgia rheumatica. Some important differentials are listed below:
- Rheumatoid arthritis
- GCA
- Anti-neutrophil cytoplasmic antibody (ANCA) related vasculitis
- Inflammatory myositis and statin-induced myopathy
- Gout & calcium pyrophosphate dihydrate crystal deposition disease (CPPD) condition
- Fibromyalgia
- Overuse or degenerative shoulder pathology i.g. osteoarthritis, tendon tear, rotator cuff tendinitis, and adhesive capsulitis
- Cervical spine disorders e.g. osteoarthritis, radiculopathy
- Crown dens syndrome
- Hypothyroidism
- Obstructive sleep apnea
- Depression
- Viral infections i.g. EBV, hepatitis, parvovirus B19, human immunodeficiency virus,
- Systemic bacterial infections, septic arthritis
- Cancer
- Diabetes
What is the diagnostic procedure for Polymyalgia rheumatica?
There is no specific test to evaluate polymyalgia rheumatica. The doctor will make a diagnosis after listening to a patient talk about the history of your symptoms & by carrying out a physical examination. You’ll also have blood tests to check for any inflammation in your body & to rule out other conditions.
The doctor might reassess your diagnosis as your treatment progresses. Some people are initially given a diagnosis of polymyalgia rheumatica and are then reclassified as having rheumatoid arthritis.
If the patient is over 50 & has the following symptoms & signs your general physician will probably diagnose polymyalgia rheumatica, & start treatment straight away:
- shoulder, neck, hip, or thigh pain evenly on both sides of the body, which has been present for at least 2 weeks
- pain & stiff muscles in the shoulders, hips, or thighs in the mornings that lasts at least 30 minutes
- high levels of inflammation found by blood tests
- no proof of rheumatoid arthritis, such as swollen joints, or positive blood tests.
The patient might be referred to a rheumatologist if there’s any hesitation about the diagnosis or if there are complicating factors. This could be if the symptoms don’t improve with steroid treatment or if the patient has side effects from the treatment.
The presence of inflammation alone will not confirm the diagnosis of polymyalgia rheumatica. Inflammation is a feature of many other conditions, including infections & rheumatoid arthritis, so the doctor might do some tests to look for signs of other conditions.
Laboratory Studies
Elevated ESR is a usual feature in polymyalgia rheumatica. ESR of more than 40 mm has been considered significant by the majority of authors. ESR less than 40 mm/h is present in 7% to 20% of patients. Patients with low ESR generally have a less frequency of systemic features like fever, weight loss, & anemia. Response to therapy, the frequency of relapses, & the risk of developing Giant cell arteritis among these patients appear to be comparable with high ESR patients. CRP is also typically elevated. CRP was found to be a more sensitive indicator of disease activity in one study while ESR was found to be a superior predictor of relapse. Normocytic anemia & thrombocytosis can occur. Liver enzymes & especially alkaline phosphatase are occasionally raised.
Serologic tests, such as an antinuclear antibody (ANA), rheumatoid factor (RF), & anti-citrullinated protein antibodies (Anti-CCPAB) are negative. The Creatine phosphokinase (CPK) value is within the normal range.
Imaging Studies
Ultrasound:
Ultrasound is useful in the diagnosis & monitoring of treatment by assessing degrees of subacromial or subdeltoid bursitis, long-head biceps tenosynovitis, & glenohumeral synovitis. In a research study power Doppler (PD) signals at subacromial or subdeltoid bursae were observed in a third of polymyalgia rheumatica patients. The positive power Doppler signal at diagnosis correlated with the increased frequency of relapses but the persistence of power Doppler findings did not correlate with relapse or recurrences. The 2012 ACR or EULAR PMR classification criteria include ultrasound.
Magnetic resonance imaging (MRI):
MRI helps depict bursitis, synovitis, & tenosynovitis in a similar way the ultrasound does, nevertheless, it is more sensitive to hip & pelvic girdle findings. Pelvic MRI often shows bilateral, peri-tendinous enhancement of pelvic girdle tendons & occasional low-grade hip synovitis. An enhancement of the proximal origin of rectus femoris seems to be a highly specific & sensitive finding.
Positron emission tomography (PET):
PET scan shows FDG uptake in shoulders, ischial tuberosities, greater trochanters, glenohumeral & sternoclavicular joints in patients with polymyalgia rheumatica. The role of PET in diagnosing large vessel vasculitis is described in a discussion below with Giant cell arteritis. 2012 Provisional classification criteria of polymyalgia rheumatica: A European League Against Rheumatism or American College of Rheumatology collaborative initiative Patients aged 50 years or older with bilateral shoulder aching & abnormal C-reactive protein concentrations or ESR, plus At least four points (without ultrasonography) or five points or more (with ultrasonography) from
- Morning stiffness in excess of 45 minutes time period (two points)
- Hip pain or restricted range of movement (one point)
- Absence of rheumatoid factor / anti-citrullinated protein antibodies (two points)
- Absence of other joint involvement (one point)
If ultrasonography is accessible, at least one shoulder with subdeltoid bursitis, biceps tenosynovitis, or glenohumeral synovitis (either posterior or axillary); & at least one hip with synovitis or trochanteric bursitis (one point) If ultrasonography is accessible, both shoulders with subdeltoid bursitis, biceps tenosynovitis, or glenohumeral synovitis (one point).
What is the treatment plan for Polymyalgia rheumatica?
Guidelines setting out the best treatment & care for patients with polymyalgia rheumatica state there should be shared decision-making between a patient & their healthcare professionals.
Medical treatment for Polymyalgia rheumatica:
If a patient has this condition, you should have a treatment plan tailored to the patient, that includes:
- the initial dose of steroids & a schedule for when this dose will ideally be reduced & by how much if your condition remains under control access to education focusing on the impact of the condition.
- the patient might be given a contact phone number or helpline number for access to doctors or nurses if they have concerns about any changes in the condition such as flares or side effects of drugs.
Steroids:
Steroid treatment is generally very effective to treat polymyalgia rheumatica. Steroids work by decreasing inflammation. They can not cure the condition, but the symptoms will improve significantly within two weeks once steroid treatment is initiated. Normally, steroid management for polymyalgia rheumatica will be taken as tablets.
Your symptoms might be almost gone after four weeks of steroid treatment. Nevertheless, treatment usually requires continued for up to two years, or sometimes longer, to stop the symptoms from returning.
Oral glucocorticoid (GC) is a well-proven treatment. The following summarizes the important points of (the European League Against Rheumatism) EULAR-ACR 2015 recommendations for management:
- 12.5 to 25 mg per day prednisone equivalent as a starting therapy
- Glucocorticoids should be tapered gradually
- Taper to an oral dose of 10 mg/day prednisone equivalent within 4 to 8 weeks
- Once remission is achieved, taper daily oral prednisone by 1 mg every 4 weeks until the halt
- Minimum of 12 months of treatment
For relapse, increase oral prednisone to the pre-relapse dose & decrease it gradually (within 4 to 8 weeks) to the dose at which the relapse occurred
Individualize dose-tapering schedules, based on regular monitoring of patient disease activity, laboratory markers, & adverse events
The steroid tablet most frequently prescribed is called prednisolone. Potential side effects can involve weight gain & the condition osteoporosis, which can cause the patient’s bones to become thinner & more fragile, and therefore might fracture more easily.
There are groups of patients who could be at an increased risk of side effects, including those who have:
- diabetes
- high blood pressure
- a recent fracture
- a peptic ulcer
- a cataract
- glaucoma.
If patients are in one of these groups, the doctor will talk to them about drugs that might be prescribed alongside steroids to reduce any risks.
After two to four weeks, the doctor will gradually reduce the dose of steroids. The reduction will be made in stages depending mainly on the symptoms but helped by carrying out repeated blood tests to look for inflammation.
If symptoms return when the dose is decreased, the doctor might have to increase the dose for a short time, possibly several weeks, & then try to decrease it again.
Patients shouldn’t stop taking steroid tablets suddenly or alter the dose unless advised by a doctor, even if their symptoms have completely cleared up. This is because the body stops developing its own steroids, called cortisol, while you’re taking steroid tablets. the body will require some time to resume normal production of natural steroids when the medicine is reduced or stopped.
Even when you feel well, the doctor might wish to see you regularly so that you can be assessed for signs of the condition coming back, or side effects from the drugs. the doctor might want to check your general health & check your blood pressure, blood sugar, & cholesterol. the patient might also be asked to have a bone density (DEXA) scan to check the strength of the bones.
It’s recommended you carry a steroid card that shows what dose of tablets you’re on & how long you’ve been taking them. This will help if a patient needs to see another doctor, for example, while you’re away from home, or another healthcare professional, for example, a dentist. Please show them the card – depending on what additional treatment the patient requires, the steroid dose might need to be adjusted.
Steroid cards are available from most pharmacies.
Other treatments:
Prevention of osteoporosis
Like all medicines, steroids can have side effects. One of the side effects of steroids is osteoporosis, which can lead bones to become thinner & then fracture.
The nationally recommended treatment for this is a medicine named bisphosphonates. These are a group of drugs that can reduce or prevent bone loss. You can ask the doctor about treatment with bisphosphonates. Examples include alendronate & risedronate.
Pain relief
Painkillers, such as paracetamol, or small courses of non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen can help ease pain & stiffness. They can be taken at the same time as steroid drugs.
Disease-modifying anti-rheumatic drugs (DMARDs)
There might be some situations where doctors will want to prescribe a type of drug called a disease-modifying anti-rheumatic drug (DMARD), alongside steroids.
These drugs work by decreasing inflammation that is causing symptoms such as pain & stiffness.DMARDs allow a lower dose of steroid to be utilized.
Consider early introduction of methotrexate (MTX) in addition to glucocorticoids, particularly in patients at more risk of relapse & prolonged therapy as well as in cases with risk factors, comorbidities, & concomitant medications where GC-related adverse events are more likely to occur. Clinical trials used methotrexate at oral doses of 7.5 to 10 mg/week. A study shows leflunomide is an effective steroid-sparing agent that can be used in polymyalgia rheumatica as well. It could be an alternative if the patient is not able to take methotrexate for various reasons. Sparse data for azathioprine exist for the treatment of polymyalgia rheumatica, its use might be an option in cases with contraindications for methotrexate. EULAR-ACR 2015 recommendations advise against the usage of anti-TNF agents.
These drugs could be prescribed if:
- patient’s symptoms don’t improve with steroids
- the patient has unusual symptoms
- it’s difficult to decrease the dose of steroids
- you get often flare-ups of your condition, where your symptoms rapidly get worse.
- You might need to see a specialist to be prescribed a DMARD.
The specialist might decide to prescribe a DMARD alongside steroid tablets, which might help to reduce the inflammation & lower the steroid dose. An example is methotrexate.
If a patient taking a DMARD it’s important to have regular check-ups, blood pressure checks, & blood tests to check for potential side effects.
Most of the data for the use of tocilizumab (TCZ) in polymyalgia rheumatica come from polymyalgia rheumatica coexisting with Giant cell arteritis. Case series & open-label studies have shown tocilizumab is useful in polymyalgia rheumatica with relapse or insufficient response to GC. An open-label study suggested that when used in newly diagnosed patients with polymyalgia rheumatica, relapse-free remission without GC treatment at 6 months was achievable. Randomized controlled trials are required to evaluate if tocilizumab is routinely beneficial in certain patients with polymyalgia rheumatica.
Calcium & vitamin D. Your doctor will likely prescribe daily doses of calcium & vitamin D supplements to help prevent bone loss as a result of corticosteroid treatment. The American College of Rheumatology recommends 1,000 to 1,200 milligrams of calcium supplements & 600 to 800 international units of vitamin D supplements for anyone taking corticosteroids for three months or more.
Vitamin D & calcium supplementation are routine recommendations for patients on long-term steroids. Bisphosphonate prophylaxis is a recommended option for patients in moderate to high fracture risk categories that would include patients over 40 years with FRAX scores of >1% & 10% risk of hip & major osteoporotic fracture respectively.
Close follow-up is recommended. Guidelines recommend follow-up at weeks 0, 1 to 3, & 6, then months 3, 6, 9, & 12 in the first year (with extra visits for relapses or adverse events). It appears prudent to follow up with patients every 3 months until remission & after that every 6 months to annually to monitor recurrence. Relapses frequently entail an increase in ESR & CRP and the return of symptoms. Elevated risk of relapse is found to correlate with a higher initial dose of steroid used, rapid steroid tapering, HLA-DRB1*0401, & persistently high inflammatory markers.
Physical therapy for Polymyalgia rheumatica:
There is currently no evidence for the usage of physical therapy in the treatment of patients with Polymyalgia rheumatica. Nevertheless, it is still important to be aware that patients might still be referred to you with a primary diagnosis of Polymyalgia rheumatica, or with Polymyalgia rheumatica as a co-morbidity. Physical therapy can be incorporated as a valuable component of a therapeutic regimen for this patient group in order to reduce the risk of early functional impairment & severe disability. A combination of exercise therapy & education is recommended in the treatment of Polymyalgia rheumatica.
Being sedentary can make Polymyalgia rheumatica stiffness worse. Physical activities & hobbies such as gardening, swimming or just taking a walk in the park are great ways to keep you active. It is good to rotate activities in order to avoid the same set of muscles & joints from getting overfatigued. Start slow & easy. Getting the body moving, even with low-impact activities, is better than rest for many patients with polymyalgia rheumatica. Work with a physical therapist. A session or two with a physical therapy professional can give you a customized set of exercises to ease your pain, improve your range of motion, fight inflammation & relieve stiffness. strengthening exercise can initiate after pain declines. Try a yoga or tai chi class it is important to perform stretches slowly & advance only if you feel comfortable & without pain.
- Strengthening exercises
- Pain control modalities
- Heat therapy
- Electrotherapy including ultrasound & Megapulse
- Transcutaneous electrical nerve supply (TENS) treatment for pain relief
- Range of movement exercises
- Hydrotherapy
- Wax therapy
- Cardiovascular activities
- Massage
- Provision of specialist equipment to help patients at home
- Pacing advice
Use Devices to Help Simplify Your Daily Activities
To help the patient get out of bed & walk around when hips and back are painful & stiff try a walker or rollator. To help with bending raising & moving arms try long-handled bath & hair brushes. If tying your shoelaces is complicated, try elastic shoelaces. To help with reaching the top of the highest kitchen cabinet or to grab clothes from the dryer purchase a reaching aid grabber tool. When buying clothing buy buttoned shirts or blouses so patients do not have to pull shirts over their heads.
Home management for Polymyalgia rheumatica:
Healthy lifestyle choices can help patients manage the side effects that corticosteroid treatment can cause:
- Eat a healthy diet. Eat a diet of fruits, vegetables, whole grains, & low-fat protein & dairy products. Limit the salt (sodium) in the patient’s diet to prevent fluid buildup & high blood pressure.
- Exercise regularly. Talk to a doctor about exercise that’s appropriate for patients to maintain a healthy weight & to strengthen bones & muscles.
- Get enough rest. Rest is necessary for the patient’s body to recover from exercise & activities of daily living.
What is the prognosis for Polymyalgia rheumatica?
When the diagnosis is made promptly, & appropriate treatment is initiated, Polymyalgia rheumatica has an excellent prognosis. Mortality among individuals with polymyalgia rheumatica is not typically increased compared to the general population.
There’s no cure for polymyalgia rheumatica, but the condition frequently improves once the patient starts treatment. In fact, it typically goes away after 2 to 6 years of treatment, & sometimes sooner.
Approximately 50% to 75% of patients can stop taking corticosteroid therapy after 2 years of treatment, & patients with polymyalgia rheumatica should be monitored regularly and carefully for symptoms & signs suggestive of Giant cell arteritis development.
FAQ (frequently asked questions)
Up to 1 in 5 people with polymyalgia rheumatica occur a more serious condition called temporal arteritis (also known as giant cell arteritis), where the arteries in the head & neck become inflamed.
Polymyalgia, or polymyalgia rheumatica, is an inflammatory condition of the muscle. The cause is uncertain but it is believed to be an autoimmune condition in which the body’s own immune system attacks the connective tissues. The primary symptoms are severe stiffness & pain in the muscles of the neck, shoulder, & hip areas.
Foods to avoid:
carbohydrates, like white bread or white rice.
alcohol
fried foods, like french fries
sugary drinks
margarine
foods with added sugar.
processed meats, like salami or hotdogs &
red meat.
Although the patient’s symptoms should improve within a few days of starting treatment, the patient will probably need to continue taking a low dose of prednisolone for about 2 years. Polymyalgia rheumatica frequently improves on its own after this time. Nevertheless, there’s a chance it will return after treatment stops.
Polymyalgia rheumatica (PMR) is an auto-inflammatory rheumatic condition of people over 50 years, presenting with pain & stiffness in the neck, shoulder, & hip girdles. The term Polymyalgia rheumatica was first used to underline that it appeared substantially milder than rheumatoid arthritis (RA) as no joint damage had been observed.





One Comment