What is Fibromyalgia?
Table of Contents
Definition-
- Fibromyalgia Syndrome is a disease distinguished by chronic pain, stiffness, and tenderness of muscles, tendons, and joints, without noticeable inflammation.
- Fibromyalgia does not cause human body damage or diseases.
- Fatigue affects 90 percent of. Fatigue affects 90 percent of individuals and sleep disorders are general.
- Fibromyalgia may be related to other rheumatic conditions, and irritable bowel syndrome (IBS).
- There is no ultimate medical test for the diagnosis of fibromyalgia and fibromyalgia symptoms may come and go over time.
- Diagnosis is dissolved by eliminating other possible causes of the symptoms.
- It may take time to establish which symptom is caused by what problem.
- FMS is NOT just one condition; it’s a complex syndrome that includes many different factors that may severely impact and disrupt a patient’s daily life.
- Fibromyalgia Syndrome (FMS) is reviewed as a systemic difficulty including biochemical, neuroendocrine, and physiologic abnormalities, leading to a disorder of pain processing and perception(i.e. allodynia, hyperalgesia).
- The symptoms correlated with FMS may arise from primary or secondary/reactive causes.
Prevalence-
- FMS occurs in more than 6 million Americans, or 4% of the population, causing it to be the most general musculoskeletal disorder in the U.S.
- It affects mainly females (90%) more often than males.
- Symptoms typically present among the ages of 20-55 years, but a person has been diagnosed as young as 6 years and as old as 85 years of age.
Pathophysiology
- The pathogenesis of FMS is theorized to be impairment of the central nervous system (CNS), distinguished by central sensitization, which is an intensified pain perception accompanied by ineffective pain inhibition and/or modulation.
- This elevated response to peripheral stimuli causes hyperalgesia, allodynia, and referred pain across multiple spinal segments, resulting in chronic widespread pain and reducing the tolerance to the sensory input of the musculoskeletal system.
- FMS systemically causes dysregulation- in neurologic, immunologic, endocrinologic, and enteric organ systems,
Autonomic Nervous System-
- The Autonomic Nervous System (ANS) is accountable for regulating the Sympathetic (“fight or flight”) and the Parasympathetic (“rest and digest”) responses, With FMS, patients feel the systemically accountable sympathetic (SNS) response with a diminished parasympathetic (PNS) modulation.
- Uninterrupted over-activation of the SNS results in improved heart rate, excessive gastric secretions and contractions, abnormalities of smooth muscle contraction throughout the digestive tract, fast and shallow respiration, and vasoconstriction.
- This may lead to malnourishment due to absorption and digestion disruptions. Long-lasting inhibition of PNS make difference in the neuro immunoendocrine systems, directly affecting growth hormone secretion by the pituitary gland.
- This may outcome in nonrestorative sleep, pain, fatigue, and cognitive/mood symptoms.
Immune System-
- The immune response to infection, inflammation, and/or trauma is the liberation of cytokines for local healing, which activate the CNS to release glial cells within the brain and spinal cord for healing support and pain response.
- With FMS, this auto-immune response is accounted for, causing an excess of glia in the human body which produces an overemphasized state of pain (chronic).
Causes of fibromyalgia-
- There are numerous hypotheses of how multiple factors play their role in the development of FMS.
- The exact etiology of FMS is still being researched; although, there are too many potential causes and risk factors, listed below, that are currently associated with, or improved one’s risk for developing this condition.
- Diet.
- Food Pyramid.
- Viral.
- Occupation, seasonal, and environmental influence.
- Adverse childhood experiences (i.e. PTSD).
- Psychological and cognitive/behavioral factors.
- Other diseases- RA, systemic lupus erythematosus, or AS.
- Present-day research leftovers inconclusive regarding the genetic or hereditary cause of SMS. A family history of FMS is a risk factor.
Characteristics/Clinical Presentation-
- Muscle pain is distinguished as the major symptom of FMS, generally mark out by patients as “aching or burning” regardless of physical activity.
- Other symptoms or associated problems happen, with various reports of frequencies, that may also affect function.
- FMS can cause residual pain sensations at a minor intensity due to repetitive exposure to peripheral stimuli or activity, also known as the “Wind-up Response.”
Symptoms-
Symptoms are often aggravated by:
- Stress.
- Overloading physical activity.
- Overstretching.
- Damp or chilly weather.
- Heat exposure to humidity.
- Sudden change in barometric pressure.
- Trauma.
- Another illness.
- Recent research carried out that functional capacity, upper limb muscular strength, postural maintenance, pain threshold, and anxiety is the most crucial predictive factor of Quality Of Life in women with FMS.
Associated Co-morbidities-
- Patient with FMS is likely to present with too many different co-morbidities. It is crucial that a diagnosis of FMS is not overlooked given the presence of additional co-morbidities more regularly diagnosed. Listed below are the most common co-morbidities associated with FMS:
- Depression
- Sleep disturbances/apnea
- Depression
- Anxiety
- PTSD
- Rheumatoid arthritis
- Systemic Lupus Erythematosus.
- Ankylosing Spondylitis (Axial Spondyloarthritis).
Fibromyalgia Diagnostic Criteria-
- There is no definitive diagnostic test nowadays available to decide the presence of FMS.
- A diagnosis of FMS is normally made based on the results of a physical examination and ruling out other similar conditions.
- No particular laboratory or radiologic testing is important for making a diagnosis; although, some recommended lab tests may be performed in order to find out other conditions.
- These tests used to find out include CBC, ESR, basic chemistry (blood urea nitrogen, creatine, hepatic enzymes, serum calcium), thyroid levels (TSH, T3, and T4), and Rheumatoid factor.
How is Fibromyalgia Diagnosed?
- The symptoms of fibromyalgia may be associated with too many conditions or diseases, making it tough to diagnose.
- The doctor or rheumatologist generally makes the diagnosis after finding out about other diagnoses.
- As well as palpating a few sensitive points around the body, the doctor may perform blood tests, scans, and x-rays to find out other causes of pain.
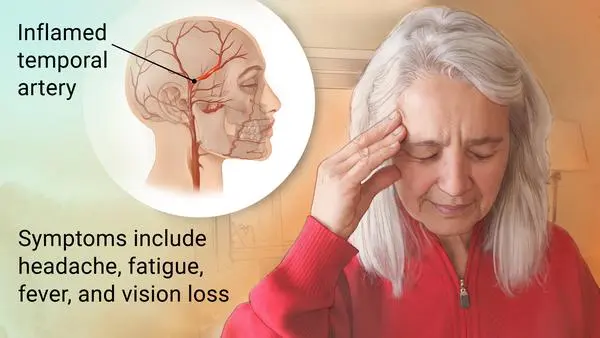
- Conditions that may mimic fibromyalgia features incorporate an underactive thyroid (hypothyroidism), vitamin D deficiency, rheumatoid arthritis, and even sleep apnoea.
Management and treatment-
Medication-
- Active rehabilitative approaches have superiority in management, but drugs may help to control symptoms.
- There is proof to support the use of amitriptyline, duloxetine, milnacipran, or pregabalin, but pure opioids should be avoided.
Physical Therapy Management & Exercise-
Passive Physical Therapy Treatments for Fibromyalgia-
Deep Tissue Massage:

- Unless the patient is in extreme amount of pain, deep tissue massage is the best fibromyalgia treatment because it uses a great deal of pressure to relieve deep muscle tension and spasms.
- Spasms prevent muscle motion at the injured level, which is one of the reasons an individual with fibromyalgia experience a reduced range of motion.
- physical therapy techniques, including deep tissue massage, will help the patient to use their muscles in a more corrective way.
- This treatment can be combined with heat or cold therapies to improve the benefits.
Heat Therapy:
- Heat therapy is one of the most desirable methods of decreasing chronic aches and pains associated with fibromyalgia.
- Heat triggers the human body’s natural healing process by relaxing the muscles and quickening the blood flow to the affected area.
- some extra blood delivers extra oxygen and nutrients.
- Blood also pulls out the waste byproducts from muscle spasms.
- Heat may not completely get rid of the source of the pain, but it may effectively reduce the pain.
- This therapy is used in two different ways—through dry heat (a heating pad or a dry, hot towel) or moist heat (steam heat or a moist, warm cloth).
- When using heat therapy on your own after physical therapy ends, never overheat painful areas.
- If the person using a heating pad, set it to low or medium.
- When using a hot towel, touch it first to be sure that it’s not too hot.
- Excessive heat may not only exacerbate the fibromyalgia pain but also potentially cause burns.
Hydrotherapy:
- As the name suggests, hydrotherapy incorporates water.
- As a passive treatment, hydrotherapy can simply involve sitting in a whirlpool bath to relieve pain, relax muscles, and condition the body without adding unnecessary stress.
Electric Muscle Stimulation:
- Electric muscle stimulation sounds exceptional, but it really isn’t painful.
- This technique decreases muscle spasms and is commonly believed to trigger the release of endorphins, which are the body’s natural painkillers
Ultrasound:
- This therapy uses sound waves to create a gentle heat that increases blood circulation to the deep tissues.
- Ultrasound helps decrease muscle spasms, inflammation, stiffness, and pain and is most effective in relieving a range of motion limitations in chronic pain sufferers, as opposed to those with acute inflammatory conditions.
Active Treatments for Fibromyalgia-
- The most important effect of active treatments is to address core stability, flexibility, strength, and joint movement.
- An exercise program can also be prescribed to achieve optimal results.
- This will not only curb recurrent pain but will also benefit overall health.
- The physical therapist will work with the patient to develop a program based on the specific symptoms and health history.
Core stability:
- The core (abdominal) muscles have a greater influence on overall health than the patient may think.
- Strong core muscles serve as good allies to the back muscles in supporting the spine.
- It’s called the core because it’s the central powerhouse of the body.
- Naturally, a healthy and wealthy core provides the body with a strong, stable center point.
Hydrotherapy:
Water-based exercises can be recommended to provide gentle aerobic conditioning.
Exercise in moderation-
- Exercise is a brilliant way to help deal with stress and depression.
- Daily basic exercise also helps to improve eating and sleeping habits, which will lead to better general health, better mental health, and less sleep deprivation.
- Activities like hydrotherapy, tai chi, pilates, yoga, walking, swimming, or cycling may benefit people with fibromyalgia stretching and mobility exercises may also help in decreasing the pain and tightness, and some specific exercises help improve strength and endurance in the ‘posture’ muscles of the body and take the load off achy muscles.
Aerobic and Resistance Exercise-

- Especially, aerobic activity has been shown to increase psychological symptoms associated with depression, cognitive decline, and sleep disturbances.
- Exercise also enhances patients’ cellular metabolism and respiratory capacity, improves lean muscle mass and tone, and also increases oxygen uptake within the body’s system(s), which ultimately diminishes their complaints of chronic pain and fatigue.
- It also incorporates walking and pool exercises.
Walking-
- A physical therapist may help the patient to develop a home exercise program, but first, why not try simply walking?
- The easiest form of activity is often the best. An individual can do it anywhere and the patient needs a decent pair of shoes.
- Begin with a short, easy walk and build up to walking for longer periods or a brisk pace.
- A better goal, according to the research, is to work up to at least 30 minutes of aerobic activity three times per week.
Pool exercises
- Warm luck water and light exercise make for a soothing combination to help ease the pain of fibromyalgia.
Manual / Passive Therapy-
- Some researches support that TENS and joint mobilizations encourage the reduction of pain as short-term relief in patients with FMS.
- Especially, patients with chronic back pain due to FMS can benefit from spinal manipulations with limited resources to support this modality.
- Moderate resources show that the use of passive STM is helpful with pain regulation.
- Furthermore, diffuse chronic pain presentations are less likely to be reliable for medical management with TENS compared to localized pain.
- Passive therapy should not be the foundation of FMS medical management due to the maladaptive sickness beliefs and coping strategies for patients’ pain.
- Manual lymph drainage therapy and connective tissue massage have also been tried in women with fibromyalgia.
- Analyzers used the Fibromyalgia Impact Questionnaire and the Nottingham Health Profile to measure the impression of the treatment.
- Their study suggests that both manual lymph drainage therapy and connective tissue massage show refinement in both the FIQ and the Nottingham Health Profile.
- Although, there was significantly greater development in the group that received manual lymph drainage therapy, suggesting that manual lymphatic drainage therapy be can preferred over connective tissue massage.
Aquatic Therapy & Balneotherapy-

- Recent research has proven that aquatic therapy is a more endurable workout for people with FMS pain.
- The water’s buoyancy allows the patient to carry on active movement without exerting excessive energy and/or improving pressure on their joints.
- In addition, proof has shown that aquatic therapy and hydrotherapy help in improving the quality of life of those with FMS long term.
- The underlying symptom(s) of fibromyalgia, central hypersensitivity, and pain, can be alleviated by the hydrostatic pressure and the effects of soothing temperature on the nerve endings, along with general muscle relaxation.
Relief of muscle and joint stiffness, tenderness, and pain-
Massage –
May assist with pain relief and help muscle relaxation.
Acupuncture –
May be helpful for the comfort of your pain.
Joint mobilization-

May improve muscle tightness, tenderness, and joint stiffness.
Managing activity levels and fatigue-
- Fibromyalgia symptoms may fluctuate, meaning that an individual may have good and bad days.
- Sometimes overdoing it one day may lead to increased symptoms the next day, so being able to manage the effort is important.
- Pacing activities and doing activity/ fatigue diaries may also help manage the fluctuations in activity and assist a person in achieving their goals.
Improve ability to cope with daily stress and depression-
- Daily stress from work or home may increase fibromyalgia symptoms.
- The patient and their physiotherapist may work with the GP to help the develop strategies to manage these stresses.
Group Exercise-
- Group exercise may be particularly advantageous for patients with fibromyalgia as it inspires the patient to maintain a consistent exercise regimen.
- Ongoing group exercise will contribute to an increment in physical function and psychological distress. Due to these noted improvements, patients can be more likely to continue their exercises at home.
Sleep health-
Understanding sleep and its impacts on health are important in helping people who have Fibromyalgia. Poor sleep health may affect:
Mood –
Sleep benefits mood, memory, and concentration.
Brain function –
Sleep helps to organize memories and increase concentration.
Emotion –
Lack of sleep may make the patient irritable, affecting emotions, social interaction, and decision-making.
Immune system –
Without enough sleep, the immune system becomes weak, and the body becomes more vulnerable to infection and disease.
Nervous system –
Sleep is the best time for rest and repair of neurons. During the time of Sleep, neurons rest, replenish, and grow.
Hormones –
substances produced to trigger or regulate proper body functions are timed to release during sleep or right before sleep.
Surgery.
Other Types of Management-
Occupational Therapy-
- Treatment focuses on activity modification principles, like working at a moderate pace, frequent positional/postural changes, and resting before fatigue sets in.
- Patients are motivated to incorporate regulating principles into all areas of life including self-care, work, and leisure.
- Proper body mechanics and posture related to home care management and work activities are evaluated and adjusted according to the individual.
Cognitive Behavioral Therapy-
- There is proof that supports the consideration of cognitive behavioral therapy (CBT) to be incorporated into the assessment and plan of care of patients with chronic pain.
- Growing proofs continue to demonstrate that CBT shows an increment in reports of pain, and decreases hyperalgesia, and chronic pain-related brain response in FMS. One other study found that behavioral insomnia therapy for patients with FMS can have a promising impact.
- The study incorporated patient education on sleeping habits and proper sleeping schedules to decrease the bouts of insomnia experienced by the patient with fibromyalgia.
- The researchers summarized that patients who received the behavioral therapy felt improvement in how long they slept and in their general condition compared to other groups.
Emotional Awareness and Expression Therapy-
- A group intervention focusing on emotional awareness and expression of emotions was found to be the most effective therapy than cognitive behavioral therapy in reducing pain for up to 6 months.
Chiropractic care & Massage-
There is no proof to support chiropractic care nor therapeutic massage is effective in pain management.
Acupuncture–
While many patients tried this treatment for reducing pain and fatigue, acupuncture techniques have weak evidence to support their effectiveness in current literature.
FAQ-
Physiotherapy is an effective method of treatment that will help reduce some of the symptoms that patients are experiencing as a result of fibromyalgia. The main goal of physiotherapy in the treatment of fibromyalgia is to decrease pain and stiffness using a combination of strategies.
Fibromyalgia was formerly classified as an inflammatory musculoskeletal disease but is now considered to be an illness that first affects the central nervous system.
Experts typically recommend any low-impact aerobic activity, like walking, swimming, or cycling. The doctor can advise the patient to work with a physical therapist on exercises specifically aimed at reducing pain and stiffness and improving function.
The 5 Stages of a Fibromyalgia Diagnosis
Stage 1: The Unknown. The patient has a variety of symptoms of widespread, ever-changing pain, often ignored as they struggle through the days, slipping behind your social engagements and housework.
Stage 2: The Aware.
Stage 3: The Flare.
Stage 4: The Roundabout.
Stage 5: Making Peace.
Fibromyalgia may be connected with ocular symptoms (foreign body sensation, irritation) and visual interference (blurred vision), coexisting with dry eye syndrome and reduced corneal sensitivity. Cases of scleritis, involving the necrotizing form, accompanying fibromyalgia have been reported.





9 Comments