Ankylosing Spondylitis: Physiotherapy Exercise
Table of Contents
What is Ankylosing Spondylitis?
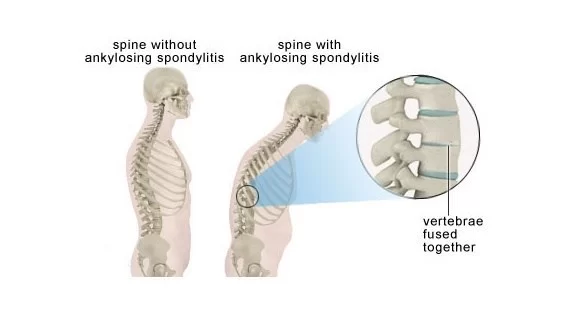
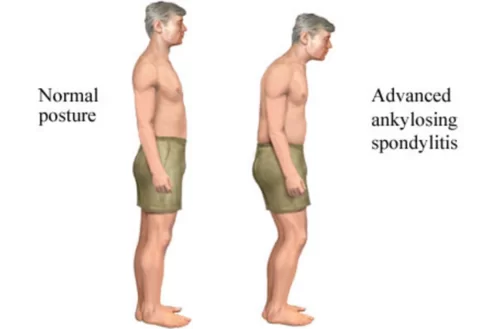
Ankylosing spondylitis (pronounced ank-kih-low-sing spon-dill-eye-tiss), or AS, is a form of arthritis that primarily affects the spine, although other joints can become involved. It causes inflammation of the spinal joints. this inflammation can lead to ankylosis — new bone formation in the spine — causing sections of the spine to fuse in a fixed, immobile position.
Ankylosing spondylitis is a form of chronic inflammation of the spine and the sacroiliac joints. The sacroiliac joints are located at the base of the lower back where the sacrum (the bone directly above the tailbone) meets the iliac bones (bones on either side of the upper buttocks) of the pelvis. Chronic inflammation in these areas causes pain and stiffness in and around the spine, including the neck, middle back, lower back, and buttocks.
ANATOMY OF SPINE:
The spine is made of a column of bones. A round bone called a vertebral body forms each bone. The body is located in the front of the spine. A bony ring attaches to the back of the vertebral body, forming a canal for the spinal cord and nerves. This bony ring is formed by two sets of bones. One set called the pedicle bone attaches to the back of each vertebral body to the side, transverse processes. Processes are outgrowths of bone and then subsequently named for where the outgrowth occurs. A lamina (Latin for plate) bone connects to the other end of the pedicle, one on the left and one on the right to connect the transverse process with the spinous process. The spinous process is your ‘back bone’. Each vertebral segment creates a bony circle, called the spinal canal or vertebral foramen, that protects the spinal cord and spinal nerves.
The lamina bones form a protective roof over the back of the spinal cord. When the vertebra bones are stacked on top of each other, the canal forms a long tube that surrounds and protects the spinal cord as it passes through the spine.
There are seven cervical (C) vertebrae, twelve thoracic (T) vertebrae, and typically five lumbar (L) vertebrae.
Pathology Related to Ankylosing spondylitis:
Synovitis Initially, the inflammation of the synovium occurs, which may be identical histologically to that in rheumatoid arthritis(RA). Most commonly synovitis starts, firstly from the sacroiliac joints followed by the other region of the spine.
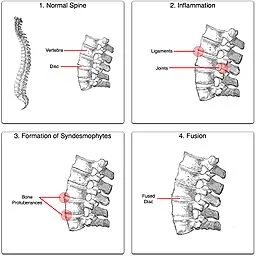
Enthesopathy This term refers to an inflammatory reaction at the enthesis which is the zone of ligamentous attachment to the bone, and this is the characteristic feature of AS that occurs commonly in the spine and near the pelvis.
Capsular Inflammation
Cartilage Destruction and Bony Erosion This occurs due to synovitis and the inflammation of the ligament and the capsules. The cartilage of the joint gets destroyed and becomes rough and the bony erosion occurs.
Ossification All the above factors lead to the formation of new bones at these areas, and bridging takes place between the vertebral bodies, usually from the edge of one body to that of the next, along the outer layer of the disc. This typical phenomenon is known as marginal syndesmophyte formation. Ossification also occurs in the anterior and posterior longitudinal ligaments and also in other ligaments of the spine.
Ankylosis All the features of the above and most importantly the ossification part, result in the fusion of all the vertebrae of the spine, and this condition is called the bamboo spine. The formation of the syndesmophytes starts usually from the dorso-lumbar region. After bony fusion the pain may subside, leaving the spine permanently stiff.
Sign and Symptoms of Ankylosing spondylitis:
Early signs and symptoms of ankylosing spondylitis might include pain and stiffness in your lower back and hips, especially in the morning and after periods of inactivity. Neck pain and fatigue also are common. Over time, symptoms might worsen, improve, or stop at irregular intervals.
Pain and stiffness. Constant pain and stiffness in the lower back, buttocks, and hips that continued for more than three months. Spondylitis often starts around the sacroiliac joints, where the sacrum (the lowest major part of the spine) joins the ilium bone of the pelvis in the lower back region.
Bony fusion. Ankylosing spondylitis can cause an overgrowth of the bones, which may lead to abnormal joining of bones, called “bony fusion.” Fusion affecting bones of the neck, back, or hips may impair a person’s ability to perform routine activities. Fusion of the ribs to the spine or breastbone may limit a person’s ability to expand his or her chest when taking a deep breath.
Pain in ligaments and tendons. Spondylitis also may affect some of the ligaments and tendons that attach to bones. Tendonitis (inflammation of the tendon) may cause pain and stiffness in the area behind or beneath the heel, such as the Achilles tendon at the back of the ankle.
Causes of AS
It’s not known what causes the condition, but there’s thought to be a link with a particular gene known as known as human leukocyte antigen B27 (HLA-B27). the general population has the HLA-B27 gene, but most don’t have AS.
DIAGNOSIS
X-rays allow your doctor to check for changes in your joints and bones, though the visible signs of ankylosing spondylitis might not be evident early in the disease.
An MRI uses radio waves and a strong magnetic field to provide more detailed images of bones and soft tissues. MRI scans can reveal evidence of ankylosing spondylitis earlier in the disease process but are much more expensive.
Lab tests
There are no specific lab tests to identify ankylosing spondylitis. Certain blood tests can check for markers of inflammation, but inflammation can be caused by many different health problems.
Your blood can be tested for the HLA-B27 gene, but most people who have that gene don’t have ankylosing spondylitis, and fewer black people with the disease have the gene than do white people.
Ultrasound scan:
An ultrasound scan can pick up inflammation of the tissues (tendons and ligaments) attached to your bones.
Ankylosing spondylitis Treatment:
The mainstay of therapy in all seronegative spondyloarthropathies are anti-inflammatory drugs, which include NSAIDs such as ibuprofen, phenylbutazone, diclofenac, indomethacin, naproxen and COX-2 inhibitors, which reduce inflammation and pain. Indomethacin is a drug of choice.
Medications used to treat the progression of the disease include the following:
Disease-modifying antirheumatic drugs (DMARDs) such as sulfasalazine can be used in people with peripheral arthritis. For axial involvement, the evidence does not support sulfasalazine. Other DMARDS, such as methotrexate, did not have enough evidence to prove their effect. Generally, systemic corticosteroids were not used due to lack of evidence. Local injection with corticosteroids can be used for certain people with peripheral arthritis.
Tumor necrosis factor-alpha (TNFα) blockers (antagonists), such as the biologics etanercept, infliximab, golimumab, and adalimumab, have shown good short-term effectiveness in the form of profound and sustained reduction in all clinical and laboratory measures of disease activity. Trials are ongoing to determine their long-term effectiveness and safety. The major drawback is the cost. An alternative may be the newer, orally administered non-biologic apremilast, which inhibits TNF-α secretion, but a recent study did not find the drug useful for ankylosing spondylitis.
Anti-interleukin-6 inhibitors such as tocilizumab, currently approved for the treatment of rheumatoid arthritis, and rituximab, a monoclonal antibody against CD20, are also undergoing trials.
Interleukin-17A inhibitor secukinumab is an option for the treatment of active ankylosing spondylitis that has responded inadequately to (TNFα) blockers.
Physiotherapy treatment :
Ultrasound, dry needling, and Transcutaneous Electrical nerve stimulation (TENS), Interferential therapy (IFT) can be effective, especially for localized pain.
Gentle spinal mobilization: passive movement applied to a spinal region or segment so as gently to increase the passive range of motion of that segment or region.”
Exercise of Ankylosing spondylitis:
Back exercise is highly important, especially in the early morning session is effective, Physiotherapy exercise helps to improve the flexibility of the spine and also reduces stiffness and maintains strength and stability of the spine, to know more about Physiotherapy exercise of Low Back click here

SQUATS EXERCISE
Stand with your back against a wall. Put your feet shoulder-width apart, and away from the wall. Slowly slide your back down the wall. It may take time, but work towards being able to get to the point where your thighs are parallel to the floor — like you’re sitting in a chair. Hold for 5 to 10 seconds. Hold for longer as you get stronger.
Repeat 3-5 times. Do 3 to 5 times a week.
Chin Tucks exercise:
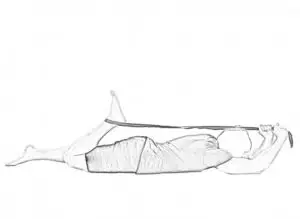
Lie on your back. Without lifting your head off the floor, tuck your chin in slightly toward your chest. Hold for 5 to 10 seconds. Repeat 3 to 5 times.
Do this stretch twice a day.
Stretch to Chest Exercise:
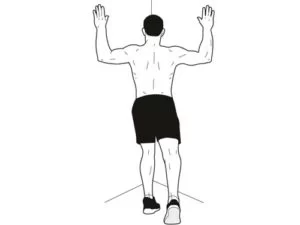
Raise your arms up. Rest the palms of your hands on the walls. Gently press your chest toward the corner. Your arms will provide tension. You’ll feel the stretch across the front of your chest. Along your back, you’ll feel your shoulder blades move toward each other. Hold for 20 to 30 seconds.
Standing Posture:

This exercise is best done in front of a full-length mirror. Stand with heels about 4 inches away from a wall. Shoulders and buttocks should be as close to the wall as possible. Stand straight and tall and hold the position for five seconds. Relax and repeat 10 times. Check your posture in the mirror and aim to stand straight and tall.
Shoulder Shrugs:
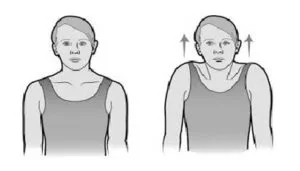
Gently shrug the shoulders towards the ears and move back down. If you are doing this exercise right, you will feel a tug in the upper back. Take a 5-second break between shoulder shrugs and repeat up to 10 times.
Quadriceps Stretch:
Lie on your stomach.
Loop a strap, belt, or sheet around the top of one foot.
Gently pull the strap over your shoulder until you feel a stretch through the muscle.
Hold for 10 to 20 seconds, then return to the start position. Repeat on the other side.
Deep Breaths Exercise:
Many people with AS eventually notice that they have trouble fully expanding their ribs and chest while they breathe. But deep breathing exercises can help prevent this problem.
Several times a day, take 3 to 4 deep breaths. Focus on pulling air deep into your chest as you inhale. Then, exhale slowly.
DO’S and DON’TS:
- Do eat a healthy diet
- Sleep on a firm mattress.
- Keep your back straight when working on a bench, table, ironing board, etc.
- Keep a cushion behind the lower back when sitting in a chair or while driving.
- Never bend at the waist to lift objects from the floor. You can kneel or bend at the knees.
- Regular back-strengthening exercises can make a huge difference to the prognosis. Lie face down on the floor with hands behind your back. Now raise your hands and shoulders off the floor, forming your back into an arch. Count three. Lower head and shoulders. Relax while you count to ten. Repeat this about 10 times.
- Get a back massage once a week.
- Relaxation techniques, yoga, and meditation help.
- Avoid sudden movements of the back.
- Do not use very thick pillows while sleeping.
- Avoid running, or jumping as they may aggravate the symptoms. Do not lift heavy weights.
- Don’t perform any exercises that cause pain. A little mild soreness afterward may be alright, but don’t overdo it.
Surgery
Your doctor might suggest surgery if you have a serious joint injury and are unable to carry out your regular activities. Not everyone is a candidate for surgery. Your doctor and you may talk over the possibilities and decide which is best for you.
Before considering surgery, your doctor will take the following into account:
- Your general well-being.
- the state of the bone or joint that is impacted.
- advantages and disadvantages of the procedure.
- Both joint replacements and repairs are possible surgical procedures.
In rare instances, some patients may require surgery to realign their spine, treat vertebral fractures, or both.
Ankylosing Spondylitis is Treated by Who?
A group of medical specialists may be needed for the diagnosis and treatment of ankylosing spondylitis. These could consist of:
- Rheumatologists are experts in treating conditions affecting the bones, joints, and muscles, including arthritis.
- Dermatologists: Skin, hair, and nail disorders are the specialty of dermatologists.
- Gastroenterologists are specialists in disorders related to the digestive tract.
- Mental health practitioners assist patients in managing challenges at work and home that may arise from their medical illnesses.
- Nurse educators are professionals with a focus on assisting patients in comprehending their overall health and developing treatment strategies.
- Occupational therapists: they provide instruction on how to decrease pain, protect joints, carry out daily tasks, and save energy.
- Ophthalmologists are specialists in eye disorders.
- Orthopedic surgeons focus on treating and operating conditions affecting the bones and joints.
- Exercise program supervisors are physiatrists, or professionals in physical medicine and rehabilitation.
- Physical therapists: they aid in enhancing joint health.
- Primary care physicians, such as family doctors or internal medicine specialists, manage additional issues as they come up and coordinate treatment across various healthcare providers.
- Social workers or psychologists who assist with psychological issues caused by illnesses.
Prognosis
A chronic (long-term) illness is ankylosing spondylitis. It’s likely that you will need to deal with your symptoms for the rest of your life. A recovery is a time when an AS patient experiences fewer or lesser symptoms. There is always a potential that symptoms could come back even if it has been a while since they occurred.
You don’t have to live in pain despite the fact that there is no treatment for AS or any other kind of arthritis. Discuss your feelings with your Doctor. Tell them how much your favorite activities are interfered with by your symptoms.
Conclusion
Taking care of any kind of arthritis can be difficult. A person with ankylosing spondylitis literally has back pain. Your daily energy levels may be negatively impacted by pain, stiffness, and other symptoms, but the good news is that AS is treatable.
Your doctor will assist you in locating therapies that lessen the degree to which AS symptoms disrupt your daily activities. Never hesitate to discuss your treatments with them or to ask questions. The greatest person to judge how you feel is you.
FAQs
Ankylosing spondylitis (AS) has no known cure, although there are treatments that can help manage the symptoms. Additionally, the process of the spine hardening and fusing together might be postponed or prevented with the use of treatment. If you have axial spondyloarthritis that is not radiological, these therapies may potentially be beneficial.
AS may have a genetic component. Yet, the precise cause remains uncertain. AS symptoms include hunched posture, stiffness in the morning, and back discomfort. Additional symptoms include weariness, fever, anaemia, inflammation of the eyes, appetite loss, weight loss, and digestive disorders can be caused by AS.
DMARDs, or disease-modifying anti-rheumatic medications, reduce inflammation and delay the progression of spondylitis. Muscle relaxants and painkillers should be used briefly to relieve extreme pain and lessen spasms in the muscles. Surgery can be used to repair a joint, insert rods into the spine, or remove sections of hardened, thicker bone.
Men are more likely than women to have AS (2:1). In most cases, the second and third decades of life are when an illness first manifests. About 80% of AS patients develop symptoms by the time they are 30 years old, whereas just 5% do so by the time they are 45 years old.





5 Comments