Knee joint
Table of Contents
What is the knee joint?
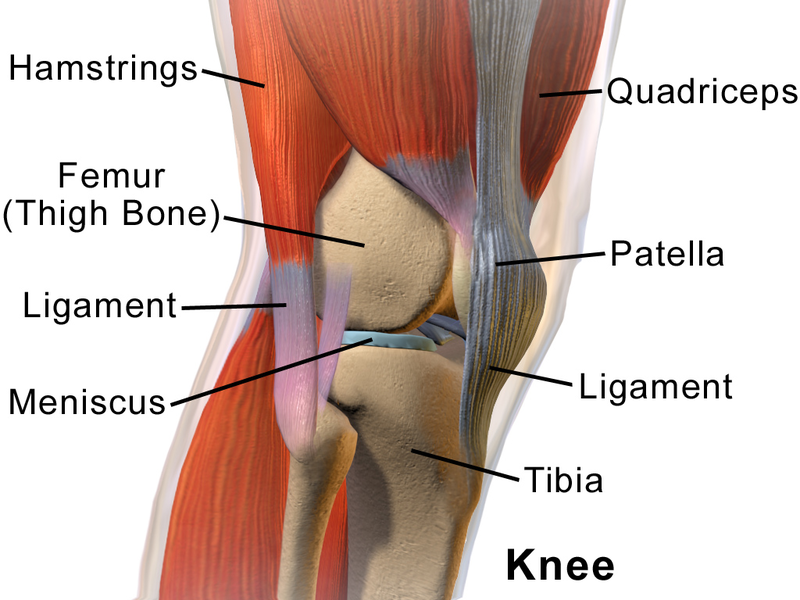
A knee is the modified hinge joint, a type of synovial joint, that is composed of three functional compartments: a patellofemoral articulation, consisting of a patella, or “kneecap”, as well as a patellar groove on the front of a femur through which it slides; & the medial as well as lateral tibiofemoral articulations linking a femur, or thigh bone, with a tibia, the main bone of a lower leg.
A joint is bathed in synovial fluid which is contained inside a synovial membrane called a joint capsule. A posterolateral corner of a knee is the area that has recently been a subject of renewed scrutiny as well as research.
The knee is the largest joint & one of the most essential joints in a body. This plays an important role in motion related to carrying a body weight in horizontal (running as well as walking) & vertical (jumping) directions.
At birth, the kneecap is just formed from cartilage, & this will ossify (change to bone) between the ages of three & five years. Due to it being the largest sesamoid bone in the human body, the ossification process takes significantly longer.
Anatomy of the knee joint
Articulating Surfaces
A thigh bone (femur), a shin bone (tibia) as well as the kneecap (patella) articulate through tibiofemoral as well as patellofemoral joints.
These three bones are covered in articular cartilage which is an extremely hard, smooth substance designed to reduce friction forces. A patella lies in the indentation of a femur famous as the intercondylar groove.
A smaller fibula runs alongside a tibia as well as is attached via a superior tibiofibular joint is not directly involved in a knee joint, but provides the surface for important muscles & ligaments to attach to.
A distal aspect of a femur forms a proximal articulating surface for a knee, which is composed of two large condyles. A medial & the lateral. These two condyles are separated inferiorly by an intercondylar notch even though they are connected anteriorly by the small shallow groove which is famous for either a femoral sulcus or even a patella groove or patella surface. This engages a patella in early flexion.
A tibia also has two asymmetrical condyles (medial as well as lateral) which are relatively flat, These are also famous as a tibial plateau. A medial tibial plateau is much longer as compared to a lateral anteroposteriorly, & the diameter of a proximal tibia is much greater than a shaft posteriorly which is sloped at approximately 7 to 10 degrees to facilitate flexion of femoral condyles on a tibia.
The two tibial condyles are separated by intercondylar tubercles, these are two bony spines that are roughened as well as their role lies within a knee extension. They become lodged in an intercondylar notch of a femur, adding to the stability of the knee joint. Overall a tibiofemoral joint is a relatively unstable joint as plateaus are slightly convex anteriorly as well as posteriorly. This emphasizes the importance of other structures of a knee namely the menisci.
Menisci
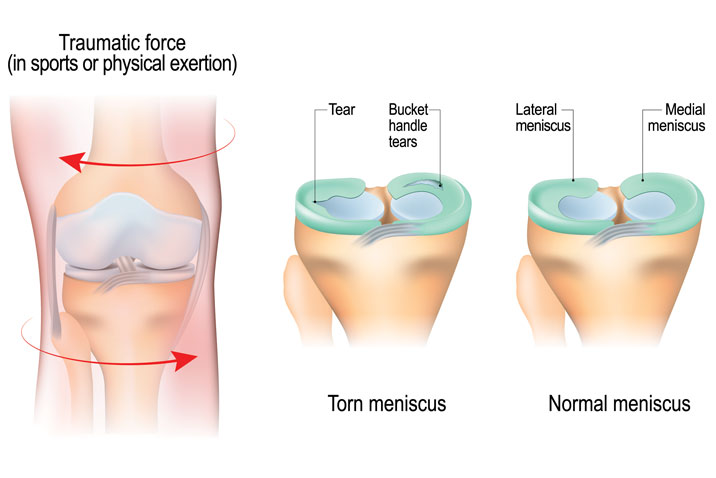
There are mainly two menisci in a space between femoral as well as tibial condyles. They are crescent-shaped lamellae, each with an anterior & posterior horn, & they are triangular in cross-section. The surface of each meniscus is concave superiorly, providing the congruous surface to femoral condyles & is flat inferiorly to accompany a relatively flat tibial plateau.
The horns of a medial meniscus are further apart as well as meniscus appears ‘C’ shaped, than those of a lateral one where the meniscus appears more ‘O’ shaped. It is because of the increased size of a medial meniscus, which unfortunately leaves the large exposed part that in turn may be prone to injury.
Menisci correct a lack of congruence between articular surfaces of the tibia as well as the femur increases the part of contact as well as increases weight distribution & shock absorption. They also assist to guide & coordinating knee motion, making them very essential stabilizers of the knee.
An arrangement of the fibers in menisci allows for axial loads to be dispersed radially reducing the wear on hyaline articular cartilage. It is mandatory as a compressive load through a knee may reach 1-2 times body weight while gait & stair climbing as well as an astonishing 3-4 times body weight while running.
Menisci are connected with a tibia by coronary ligaments. A medial meniscus is a much less mobile while joint movement than a lateral meniscus due in large part to its firm attachment to a knee joint capsule as well as medial collateral ligament (MCL). On a lateral side, a meniscus is less firmly attached to a joint capsule & has no attachment to a lateral collateral ligament (LCL). In fact, a posterior horn of a lateral meniscus is separated entirely from a posterolateral aspect of the knee joint capsule by a tendon of the popliteus muscle as it descends from the lateral epicondyle of a femur.
During the first year of life, the menisci are fully vascularized but once weight-bearing commences vascularity diminishes to an outer third (red zone), a red zone being the only part having the slight ability to heal. An inner non-vascularized part (white zone) receives nutrition through the diffusion of synovial fluid in the joint.
Ligaments & Joint Capsule
A joint capsule has thick as well as fibrous layers superficially & thinner layers deeper. It alongside the capsule ligaments increases the stability of the knee. As with all of the structures from a knee they are under most tension and hence more stable in the extended (closed packed) position in comparison to a laxity present in the flexed position (open packed).
Inside the capsule is the specialized membrane famous as the synovial membrane which provides nourishment to all the surrounding structures. A synovial membrane produces synovial fluid which lubricates a knee joint. Other structures mainly include an infrapatellar fat pad as well as bursa which function as cushions to exterior forces on a knee.
This synovial fluid that lubricates a knee joint is pushed anteriorly when a knee is in extension, and posteriorly when a knee is flexed & in the semi-flexed knee, a fluid is under the least tension, therefore, being the most comfortable position if there is the knee joint effusion.
The ligaments of a knee maintain the stability of the knee. Each ligament has a particular function in assisting in maintaining optimal knee stability.
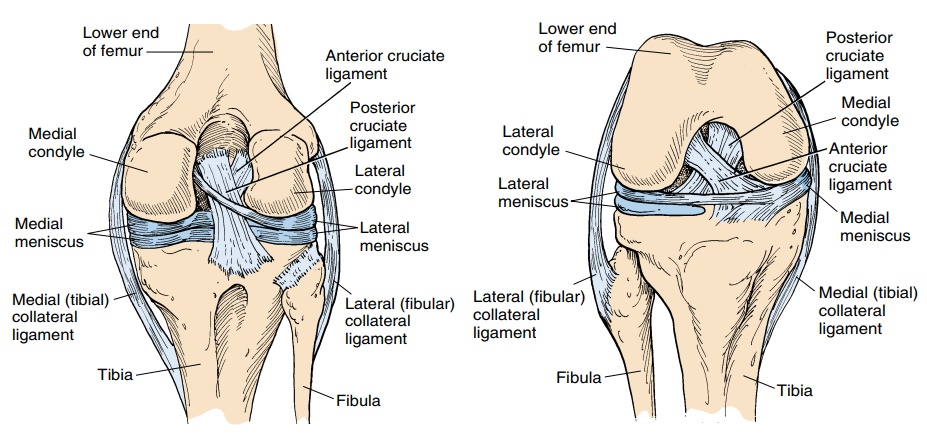
- Medial Collateral Ligament (MCL) – This medial collateral ligament may be divided into two sets of fibers – superficial as well as deep fibers. A general location of this band runs from a medial epicondyle of a femur to the medial condyle as well as a superior part of a medial surface of a tibia. The superficial fibers start from the medial femoral condyle & attach to a medial aspect of a proximal tibia distally to the pes anserinus. The deep fibers are continuous to a knee joint capsule & originate from the inferior aspect of a medial femoral condyle and insert into a proximal aspect of a medial tibial plateau. In the middle of a ligament, the deep fibers are attached to the medial meniscus. The medial collateral ligament primarily resists forces acting from the outer surface of a knee, valgus forces, but also resists a lateral rotation of a tibia on the femur. The medial collateral ligament is able to resist the valgus stress more effectively in the closed pack position (extension) because of the laxity of a ligament in the open packed position (flexed). The medial collateral ligament does have another role in restraining the anterior translation of a tibia on the femur. Thus, when someone has an MCL injury the protection of an anterior cruciate ligament needs to be considered.
- Lateral Collateral Ligament (LCL) – the cord-like ligament that starts on a lateral epicondyle of a femur & joins with a tendon of the biceps femoris (hamstring muscle) to form a conjoined tendon. The ligament is different from the medial collateral ligament & is considered to be the extracapsular ligament. this main role is resisting varus forces on a knee, as well as similar to the medial collateral ligament is most effective in full extension. another similarity of a medial collateral ligament, as well as a lateral collateral ligament, is the ability of the LCL to also resist lateral rotation of a tibia on a femur.
- Anterior Cruciate Ligament (ACL) – The ACL is the essential structure in a knee joint for resisting the anterior translation of a tibia on a femur. The ligament is a very well-known ligament owing to the high injury rate of athletes, which has resulted in a lot of research being done in the field of the anterior crucial ligament. The cruciate ligaments are so known because they form the cross in a middle of a knee joint. The anterior crucial ligament runs from the anterolateral aspect of a medial intercondylar tibial spine superolateral as well as posteriorly to a posteromedial aspect of a lateral femoral condyle. The anterior crucial ligament twists medially as it travels proximally. There are thought to be two bundles of fibers that form the ACL – an anteromedial bundle (AMB) as well as the posterolateral bundle (PLB). An anterior crucial ligament is responsible for resisting anterior shearing forces on a knee. Depending on the position of the knee, will depend on which bundle of the anterior crucial ligament fibers will be taut. So when a knee is close to full extension the PLB will be taut as well as resisting a force, but as a knee moves into the flexed position the PLB becomes lax & the AMB becomes taut taking over the role of resisting anterior shearing forces. At approximately 30 degrees of flexion, neither of the bundles of a ligament is taut leading to the most anterior translation available at this range. This is most commonly injured in twisting movements. An ACL is also the accessory ligament in resisting rotary forces medially & laterally as well as valgus & varus forces. The PLB of the anterior crucial ligament is theorized to be most effective at providing rotary stability to a knee. Moreover, to this, the AMB is under most tension at approximately 10-15 degrees of knee flexion with medial rotation.
- Posterior Cruciate Ligament (PCL) – The described ligament runs from a posterior surface of a tibia between the two posterior horns of menisci it then runs superiorly as well as anteriorly & attaches to a lateral aspect of the medial femoral condyle. The posterior cruciate ligament is much shorted as well as less oblique with a much larger cross-sectional area in comparison to the anterior cruciate ligament. As the posterior cruciate ligament blends with a posterior capsule as it crosses to a tibial attachment. Factors namely the size, shape as well as location possibly contribute to the increased strength of the posterior cruciate ligament in comparison to an ACL & which is much less frequently injured. The posterior cruciate ligament similarly has two bundles of fibers a posteromedial (PMB) as well as an anterolateral bundle (ALB). When a knee is in near full extension the ALB which is much larger & stronger is lax as well as the PMB are taut whereas in 80-90 degrees of flexion the PMB are lax & the ALB are taut. The posterior cruciate ligament is more adept at resisting posterior translation / sheering forces in the knee when it is flexed in spite of there being the most posterior translation available at 75-90 degrees flexion. The secondary stabilizers at this point in a range are ineffective as well as rely upon the posterior cruciate ligament. The posterior cruciate ligament also plays an essential role in resisting rotation & valgus/varus forces on a knee. The posterior cruciate ligament best resists medial tibial rotation at 90 degrees flexion rather than extension but is not very good at resisting lateral tibial rotation. If the posterior cruciate ligament becomes damaged a popliteus muscle plays an essential role in stabilizing a knee from posterior sheering forces. In a posterior cruciate ligament, deficient person hamstring contraction may destabilize a knee joint alongside the gastrocnemius contractions (at angles greater than 40 degrees knee flexion), while quadriceps contractions degrees the strain on the posterior cruciate ligament between angles of 20 and 60 degrees flexion.
Bursa
The bursa is a fluid-filled sac that reduces friction between two tissues. A knee is surrounded by several bursae. The largest bursa in a body is the suprapatellar bursa & which will often fill with fluid when a knee is injured. It may be referred to as “water on the knee”.
The most commonly injured bursa is a prepatellar bursa, which is in front of a patella as well as the pes anserinus bursa, which is located at the insertion of the three medial muscles of the knee joint.
Common conditions of a bursa include prepatellar bursitis, pes anserinus bursitis, and “fluid on the knee”.
Muscles around Knee joint
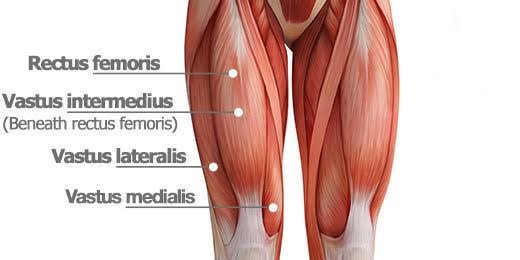
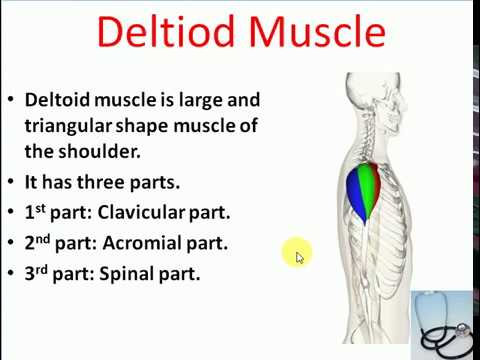
Extensors muscle of the knee : Quadriceps are the prime knee extensors of the knee joint.
- Articularis genus muscle
Origin: Distal end of the anterior femoral shaft.
Insertion: Proximal extension of a knee joint capsule.
Blood supply: Femoral artery
Nerve supply: Femoral nerve
Action: Pulling a suprapatellar bursa while the extension of the knee. - Rectus femoris muscle
Origin: Anterior inferior iliac spine & the exterior surface of a bony ridge which forms an iliac portion of the acetabulum.
Insertion: Patella as well as Tibial tuberosity via the Patellar ligament.
Blood supply: Femoral artery.
Nerve supply: Femoral nerve.
Action: Extension of the knee as well as flexion of the hip.
Antagonist: Hamstring muscle. - Vastus lateralis
Origin: Greater trochanter, Intertrochanteric line, and linea aspera of the femur as well.
Insertion: Patella as well as tibial tuberosity via the patellar ligament.
Blood supply: Femoral artery.
Nerve supply: Femoral nerve.
Action: Extends as well as stabilizes the knee.
Antagonist: Hamstring muscle. - Vastus intermediates
Origin: Superior 2/3 of the anterior as well as lateral surfaces of the femur; also from the lateral intermuscular septum of the thigh.
Insertion: Lateral border of a patella; and forms the deep portion of the quadriceps tendon.
Nerve supply: Muscular branches of the femoral nerve
Blood supply: Lateral circumflex femoral artery
Action: Extension of the knee - Vastus medialis
Origin: Lower part of an intertrochanteric line, along with the spiral line to a medial lip of a linea aspera, a medial intermuscular septum as well as the aponeurosis of adductor Magnus.
Insertion: Into a medial side of the quadriceps tendon, joining with rectus femoris as well as the other quadriceps muscles, enveloping a patella, then by a patellar ligament into the tibial tuberosity.
Blood supply: Femoral artery.
Nerve supply: Femoral nerve.
Action: Extension of a knee.
Antagonist: Hamstring muscle.
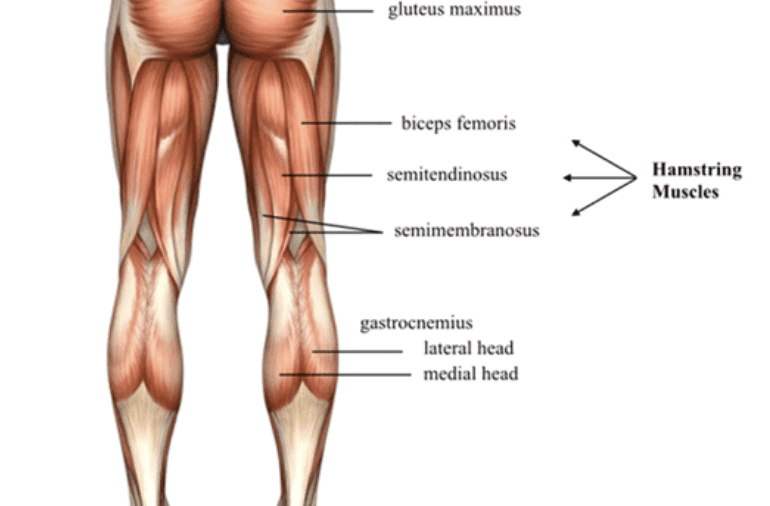
Knee Flexors muscles
Hamstring muscles are the chief Knee flexors muscle.
Posterior compartment
- Sartorius
Origin: Anterior superior iliac spine of the pelvis.
Insertion: Pes anserinus.
Blood supply: Superficial circumflex iliac artery, lateral femoral artery, deep femoral artery, descending geniculate artery, as well as the femoral artery.
Nerve supply: Femoral nerve.
Action: At the hip joint: flexion, lateral rotation as well as abduction. At the knee joint: flexion as well as medial rotation.
Antagonist: Quadriceps muscle (partly) - Biceps femoris muscle
Origin: Long head: Tuberosity of an ischium, short head: linea aspera on a femur.
Insertion: The head of a fibula articulates with a back of a lateral tibial condyle.
Blood supply: Inferior gluteal artery, perforating arteries, as well as popliteal artery.
Nerve supply: Long head: medial (tibial) part of the sciatic nerve, short head: a lateral (common fibular) part of the sciatic nerve.
Action: Flexion of the knee, laterally rotates leg at the knee (when the knee is in flexion), extends hip joint (long head only).
Antagonist: Quadriceps muscles. - Semitendinosus
Origin: Posteromedial impression of the Ischial tuberosity.
Insertion: Proximal end of the tibia below medial condyle via pes anserinus.
Action: At the hip joint: Thigh extension, thigh internal rotation, as well as stabilizes the pelvis, At the knee joint: Leg flexion, leg internal rotation.
Nerve supply: Tibial division of sciatic nerve (L5-S2)
Blood supply: First perforating branch of the deep femoral artery, medial femoral circumflex artery, inferior gluteal artery as well as an inferior medial geniculate artery. - Semimembranosus
Origin: Superolateral impression of the ischial tuberosity.
Insertion: Medial condyle of the tibia bone.
Action: At hip joint: Thigh extension as well as internal rotation.
Knee joint: Flexion, as well as internal rotation of the leg, stabilizes the pelvis.
Nerve supply: Tibial division of sciatic nerve (L5 – S2)
Blood supply: Perforating branches of the femoral and popliteal arteries as well. - Gastrocnemius muscle
Origin: Lateral head: Posterolateral aspect of the lateral condyle of a femur. Medial head: Posterior surface of the medial femoral condyle, the popliteal surface of the femoral shaft.
Insertion: Posterior surface of a calcaneus via the calcaneal tendon.
Nerve supply: Tibial nerve (S1, S2)
Action: Talocrural joint: Foot plantar flexion and Knee joint: Leg flexion. - Plantaris
Origin: Lateral supracondylar line of the femur, oblique popliteal ligament of the knee.
Insertion: Posterior surface of the calcaneus via a calcaneal tendon.
Action: Talocrural joint: Foot plantar flexion and Knee joint: knee flexion.
Nerve supply: Tibial nerve (S1, S2).
Blood supply: Superficially: lateral sural as well as popliteal arteries and Deeply: superior lateral genicular artery. - Popliteus
Origin: Lateral condyle of the femur, posterior horn of the lateral meniscus of the knee joint.
Insertion: Posterior surface of the proximal tibia.
Nerve supply: Tibial nerve (L4-S1)
Blood supply: Inferior medial as well as lateral genicular arteries (popliteal artery), posterior tibial recurrent artery, posterior tibial artery, nutrient artery of the tibia as well.
Action: Unlocks the knee joint; Knee joint stabilization.
Medial compartment
Gracilis
Origin: Anterior body of the pubis, inferior pubic ramus, ischial ramus as well.
Insertion: Medial surface of the proximal tibia via pes anserinus.
Action: At the hip joint: Thigh flexion, thigh adduction; At the knee joint: leg flexion, leg internal rotation
Nerve supply: Obturator nerve (L2-L3)
Blood supply: Deep femoral artery via artery to the adductors.
Function of the knee joint
Osteokinematics & range of motion
- The ligaments, as well as menisci, provide static stability & the muscles and tendons dynamic stability.
- The main motion of the knee is flexion as well as extension. For that matter, the knee act as the hinge joint, whereby an articular surface of a femur roll & glide over the tibial surface. While the flexion & extension of the knee, tibia as well as patella act as one structure in relation to the femur. The quadriceps muscle group is made up of 4 different individual muscles. They join together forming one single tendon that inserts into an anterior tibial tuberosity. Embedded in a tendon is a patella, the triangular sesamoid bone & its function is to enhance the efficiency of the quadriceps contractions. Contraction of the quadriceps pulls a patella upwards as well as extends the knee.
Range of motion
Knee range of Motion:
- Knee extension 0 degrees. A hamstring muscle group consists of the biceps femoris, semitendinosus and semimembranosus as well. They are situated at a back of a thigh & their function is flexing or bending the knee and providing stability on either side of the joint line. Range of motion: Knee flexion 135 degrees.
- Secondary movement is internal as well as external rotation of a tibia in relation to a femur, but it is possible only when a knee is flexed.

- Extended position
With a knee extended, both lateral as well as medial collateral ligaments, and the anterior part of an anterior cruciate ligament, is taut. While extension, the femoral condyles glide & roll into the position which causes a complete unfolding of a tibial collateral ligament. During the last 10 degrees of extension, the obligatory terminal rotation is triggered in which a knee is rotated medially 5 degrees. The final rotation is produced by the lateral rotation of a tibia in the non-weight-bearing leg, & by the medial rotation of a femur in the weight-bearing leg. The terminal rotation is made possible by a shape of a medial femoral condyle, helped by contraction of the popliteus muscle as well as the iliotibial tract & which is caused by the stretching of an anterior cruciate ligament. Both cruciate ligaments are slightly unwinded & both lateral ligaments become taut. - Flexed position
In the flexed position, the collateral ligaments are relaxed whereas the cruciate ligaments are taut. Rotation is controlled by twisted cruciate ligaments; the two ligaments get twisted around each other while the medial rotation of a tibia which decreasing the amount of rotation possible while they become unwound during lateral rotation of a tibia. Owing to an oblique position of the cruciate ligaments, at least part of one of them is always tense & these ligaments control a joint as the collateral ligaments are relaxed. In addition, the dorsal fibers of a tibial collateral ligament become tensed while extreme medial rotation & the ligament also decreases the lateral rotation to 45–60 degrees.
Arthrokinematics
- Viewed in a sagittal plane, the articulating surface of the femur is convex whereas the articulating surface of the tibia is concave. The knee arthrokinematics is based on the rules of concavity as well as convexity and is described in terms of open as well as a closed chain:
- Open kinetic chain:
- During the knee extension, the tibia glides anteriorly on the femur. More precisely, from 20 degrees knee flexion to full extension, the tibia rotates externally. During knee flexion, the tibia glides posteriorly on the femur & from full knee extension to 20 degrees flexion, the tibia rotates internally.
- Closed kinetic chain:
- During knee extension, the femur glides posteriorly on the tibia. To be more specific, from 20 degrees knee flexion to full extension, while that time the femur rotates internally on the stable tibia. During knee flexion, the femur glides anteriorly on the tibia & from full knee extension to 20 degrees flexion, the femur rotates externally on the stable tibia.
- The “screw home mechanism”:
- The “screw-home” mechanism, considered to be a key element to knee stability, is a rotation between the tibia as well as the femur. It happens at the end of the knee extension, between full extension (0 degrees) and 20 degrees of knee flexion. The tibia rotates internally while the open-chain motions (swing phase) as well as externally while the closed-chain movements (stance phase). External rotation happens during the terminal degrees of the knee extension & results in the tightening of both cruciate ligaments, which locks the knee. A tibia is then in a position of maximal stability with respect to a femur.
Clinical importance
- The knee pain is caused by trauma, misalignment, as well as degeneration by conditions such as arthritis. The most common knee disorder is generally famous as patellofemoral syndrome. The majority of minor cases of knee pain may be treated at home with rest as well as ice but more serious injuries do require surgical care.
- One form of the patellofemoral syndrome involves a tissue-related problem that creates pressure as well as irritation in a knee between the patella & the trochlea (patellar compression syndrome), which causes pain. The second major class of knee disorder involves the tear, slippage, or even dislocation that impairs a structural ability of a knee to balance the leg (patellofemoral instability syndrome). Patellofemoral instability syndrome can cause either pain, a sense of poor balance, or even both.
- Prepatellar bursitis also famous as a housemaid’s knee is a painful inflammation of a prepatellar bursa (the frontal knee bursa) often brought about by occupational activity namely roofing.
- Age also contributes to disorders of the knee. Particularly in elderly individuals, knee pain frequently arises because of
- Osteoarthritis of Knee joint. Moreover, the weakening of the tissues around a knee may contribute to the issue. Patellofemoral instability can relate to hip abnormalities or even to the tightness of surrounding ligaments.
Cartilage lesions may be caused by:
- Accidents (fractures),
- Injuries,
- Removal of the meniscus,
- Anterior cruciate ligament injury,
- Posterior cruciate ligament injury,
- Posterolateral corner injury,
- Medial knee injuries,
- The considerable strain on a knee.
- Any kind of work while which the knees undergo heavy stress can also be detrimental to cartilage. It is especially the case in professions in which individuals frequently have to walk, lift, or even squat. Other causes of the pain can be excessive on, & wear off, the knees, in combination with such things as muscle weakness as well as overweight.
Common complaints:
- The painful, blocked, locked, or even swollen knee. Sufferers sometimes feel as if their knees are about to give way or even can feel uncertain about their movement.
- Overall fitness & knee injury.
- Physical fitness is related integrally to the development of knee issues. The same activity namely climbing stairs can cause pain from patellofemoral compression for a person who is physically unfit, but not for someone else (or for that person at a different time).
- Obesity is another major contributor to knee pain. For example, a 30-year-old woman who weighed 120 lb at age of 18, before her three pregnancies, & now weighs 285 lb, had added 660 lb of force across her patellofemoral joint with each step.
Common injuries because of physical activity:
- Model demonstrating parts of the artificial knee
- In sports that place great pressure on the knees, especially with the twisting forces, this is most common to tear one or even more ligaments or cartilages.
- Some of the most known knee injuries are those to the medial side: medial knee injuries.
Anterior cruciate ligament injury:
Main article: Anterior cruciate ligament injury in the knee
The anterior cruciate ligament is the most commonly affected or even injured ligament of a knee. An injury is common while sports. Twisting of a knee is a common cause of over-stretching or even tearing the ACL. When the anterior crucial ligament is injured the popping sound can be heard, & a leg may suddenly give out. Besides swelling as well as the pain, walking can be painful & a knee will feel unstable. Minor tears of an anterior cruciate ligament can heal over time, but the torn ACL requires surgery. After surgery, recovery is prolonged & low-impact exercises are recommended to strengthen a knee joint.
Torn meniscus injury:
Menisci act as a shock absorber & separate the two ends of the bone in a knee joint. There are two menisci in a knee, a medial (inner) as well as a lateral (outer). When there is torn cartilage, this means that a meniscus has been injured. Meniscus tears happen while sports often when a knee is twisted. Menisci injury can be innocuous & one may be able to walk after the tear, but soon swelling as well as the pain set in. Sometimes a knee will lock during bending. Pain often happens when one squats. Small meniscus tears are treated conservatively but most large tears need surgery.
Fractures:
Knee fractures are rare but do happen, especially as a result of road accidents. Knee fractures include the patella fracture, & a type of avulsion fracture called a Segond fracture. There is usually immediate pain as well as swelling, & difficulty, or even inability to stand on a leg. The muscles go into spasm & even the slightest movements are painful. X-rays may easily confirm an injury & surgery will depend on the degree of displacement & type of fracture as well.
Ruptured tendon:
Tendons usually attach muscle to the bone. In a knee, the quadriceps & patellar tendon may sometimes tear. The injuries to these tendons happen when there is a forceful contraction of a knee. If a tendon is completely torn, bending or even extending a leg is impossible. The completely torn tendon needs surgery but a partially torn tendon may be treated with leg immobilization followed by physiotherapy.
Overuse:
Overuse injuries of a knee include tendonitis, bursitis, muscle strains, as well as iliotibial band syndrome. These injuries often develop slowly over weeks or even months. some activities that induce pain usually delay healing. Rest, ice, as well as compression, do assist in most cases. Once the swelling has diminished, heat packs may increase blood supply & promote healing. Most overuse injuries subside with time but may flare up if the activities are quickly resumed. People may decrease the chances of overuse injuries by warming up prior to exercise, limiting high-impact activities & keep their weight under control.
Varus or even valgus deformity:
Hip knee ankle angle:
There are two disorders relating to the abnormal angle in a coronal plane at a level of the knee:
Genu valgum is the valgus deformity in which a tibia is turned outward in relation to a femur, resulting in the knock-kneed appearance.
Genu varum is the varus deformity in which a tibia is turned inward in relation to a femur, resulting in the bowlegged deformity.
The degree of varus or even valgus deformity may be quantified by a hip-knee-ankle angle, which is the angle between a femoral mechanical axis & the center of an ankle joint. This is normally between 1.0° & 1.5° of varus in adults. Normal ranges are different in the children.

47 Comments