Anterior Cruciate Ligament
Table of Contents
Introduction
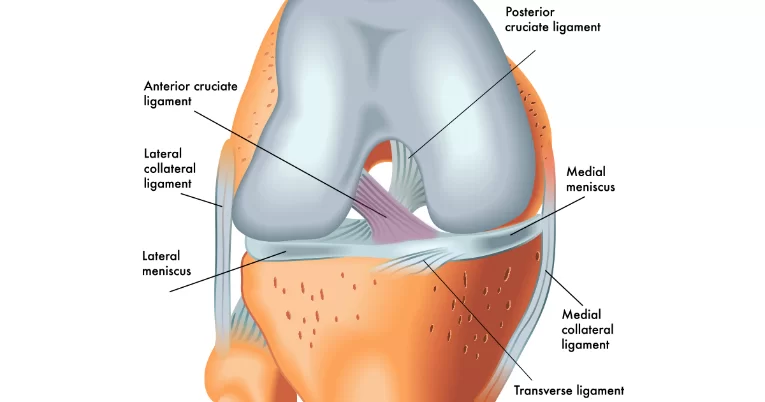
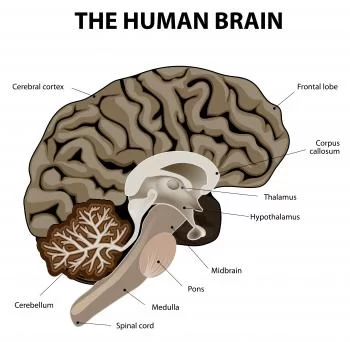
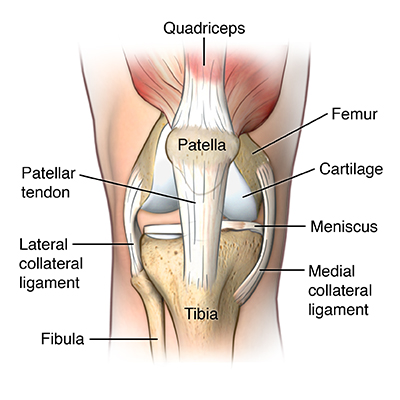
The anterior cruciate ligament (ACL) is one of the important ligaments in the knee joint. The ACL is a strong and rope-like structure. It is located in the center of the knee and is responsible for providing stability to the joint during movements such as jumping, running, and cutting.
The ACL connects the femur (thigh bone) to the tibia (shin bone) and prevents excessive forward movement of the tibia in relation to the femur. It also helps to control rotational movements of the knee joint. Injuries to the ACL are common in sports that involve sudden stops, changes in direction, or jumping and can result in significant pain and instability in the knee joint.
Origin and insertion of the ACL
The anterior cruciate ligament (ACL) originates from the posterior aspect of the lateral femoral condyle, which is a bony prominence on the outer side of the bottom end of the thigh bone (femur). The femoral attachment of the ACL is located just behind the intercondylar notch, which is a groove between the two bony prominences on the bottom end of the thigh bone.
From its origin, the ACL passes diagonally downward and forward through the center of the knee joint, crossing over the posterior cruciate ligament (PCL) to attach to the anterior aspect of the tibial plateau. The tibial plateau is a flat, upper surface of the shin bone (tibia) that forms the top part of the knee joint.
The tibial attachment of the ACL is located on a small bony prominence called the anterior tibial spine, which is located at the front of the tibial plateau. The ACL attaches to the tibial spine through a strong, fibrous band of tissue called the ACL tibial insertion.
Mechanism of the anterior cruciate ligament
The mechanism of the anterior cruciate ligament (ACL) involves its role in preventing excessive forward movement of the tibia in relation to the femur, as well as rotational instability of the knee joint. This is accomplished through a combination of passive and active stabilization.
Passive stabilization refers to the structural support provided by the ACL itself. The ligament is composed of strong, fibrous tissue that connects the femur to the tibia. It is oriented diagonally across the knee joint, which allows it to resist both forward and rotational forces.
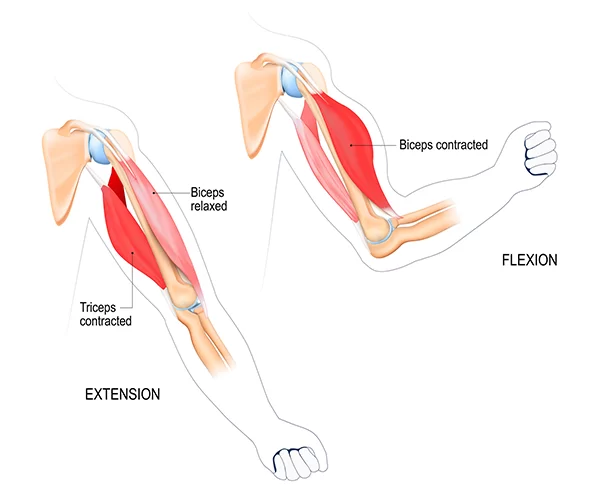
Active stabilization refers to the role of the muscles surrounding the knee joint in maintaining proper ACL function. The quadriceps, hamstrings, and calf muscles all play a role in stabilizing the knee joint during movement. These muscles work together to control the movement of the tibia in relation to the femur, which helps to prevent excessive stress on the ACL.
During physical activities such as running, jumping, and cutting movements, the ACL is subjected to significant forces. These forces can cause the ligament to stretch or tear, resulting in an ACL injury. Common causes of ACL injuries include sudden stops or changes in direction, direct blows to the knee, or landing awkwardly from a jump.
In summary, the mechanism of the anterior cruciate ligament involves its role in passive and active stabilization of the knee joint. The ligament provides structural support to prevent excessive forward and rotational movement of the tibia, while the surrounding muscles work together to control movement and reduce stress on the ACL.
Symptoms of the anterior cruciate ligament injury
Symptoms of an anterior cruciate ligament (ACL) injury can vary depending on the severity of the injury. Common symptoms include:
- Sudden pain: An ACL injury often causes sudden and intense pain in the knee.
- Swelling: A frequent sign of ACL damage is swelling around the knee joint. The swelling may occur immediately after the injury or may take a few hours to develop.
- Limited range of motion: An ACL injury can cause a limited range of motion in the knee joint. The knee may experience stiffness or difficulty moving.
- Instability: The knee may feel unstable or wobbly, especially when standing or walking. This is due to the loss of stability provided by the ACL.
- Popping sound: Some people may hear a popping sound at the time of the injury, which can indicate a tear in the ACL.
- Difficulty bearing weight: It may be difficult to bear weight on the affected leg due to pain and instability.
- Muscle weakness: An ACL injury can cause muscle weakness in the affected leg, which can make it difficult to perform everyday activities.
If you experience any of these symptoms after a knee injury, it is important to take medical attention. A doctor can perform a physical examination and imaging tests to diagnose an ACL injury and recommend appropriate treatment.
Injuries of the anterior cruciate ligament
Activities that can cause an anterior cruciate ligament (ACL) injury typically involve sudden changes in direction, stopping quickly, or landing from a jump. Some common activities that can lead to ACL injuries include:

- Sports: High-impact sports such as football, basketball, soccer, and skiing put individuals at a higher risk of ACL injuries due to the sudden changes in direction and pivoting movements involved.
- Gymnastics: Gymnasts often perform high-risk maneuvers that require jumping, landing, and twisting, which can put significant stress on the knee joint and increase the risk of ACL injuries.
- Dance: Dancers may experience ACL injuries due to the repetitive stress placed on the knee joint during jumps and landings.
- Martial arts: Martial artists are at risk of ACL injuries due to the sudden changes in direction and pivoting movements involved in their training.
- Running: Runners may experience ACL injuries due to overuse or sudden changes in direction while running.
- Falls: Falling directly onto the knee or landing awkwardly after a fall can also cause ACL injuries.
It is important to note that ACL injuries can occur in anyone, regardless of their level of physical activity or fitness. However, individuals who participate in high-impact activities or sports are at a higher risk of experiencing an ACL injury.
Treatment of the anterior cruciate ligament injury
The anterior drawer test
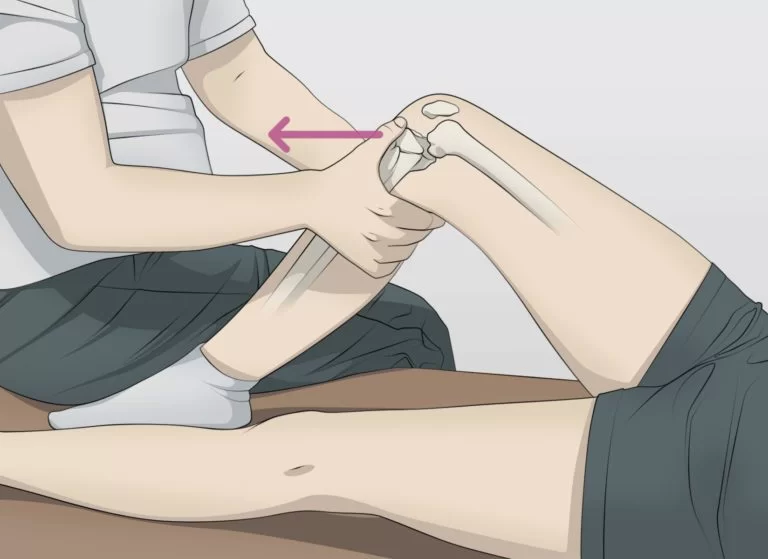
The anterior drawer test is a physical examination test helpful to examine the condition of the anterior cruciate ligament (ACL) in the knee joint. The ACL is one of the four major ligaments that stabilize the knee joint, and it is commonly injured during sports activities or sudden twisting movements.
During the anterior drawer test, the patient lies on their back with their knee bent at a 90-degree angle. The examiner sits on the foot of the affected leg and places both hands around the upper part of the lower leg, just below the knee joint.
The examiner then pulls the tibia (lower leg bone) forward while pushing the femur (thigh bone) backward. This motion simulates the movement of the tibia in relation to the femur during an ACL injury. If the ACL is intact, there should be minimal forward movement of the tibia.
However, if the ACL is torn or partially torn, there will be excessive forward movement of the tibia, indicating a positive test result. The degree of forward movement can be graded on a scale from 0 to 3, with 0 indicating no movement and 3 indicating significant movement.
It is important to note that the anterior drawer test is not always reliable and may produce false negative or false positive results. Therefore, it should be used in conjunction with other diagnostic tests such as MRI or arthroscopy to confirm an ACL injury.
Overall, the anterior drawer test is a simple and non-invasive test that can help to assess the integrity of the ACL in patients with suspected knee injuries.
Surgical treatment
Surgical treatment of the ACL typically involves reconstructing the ligament using a graft from another part of the body or from a donor. The surgery is usually performed under general anesthesia and may be done arthroscopically, which involves making small incisions and using a camera and specialized instruments to perform the procedure.
During the surgery, the torn ligament is removed, and tunnels are drilled into the thighbone and shinbone to place the graft in the same position as the original ACL. The graft is secured in place using screws, buttons, or other devices.
After surgery, patients will typically need to wear a brace and use crutches for a period of time to allow for healing. Physical therapy is also an important part of recovery, as it helps to restore range of motion, strength, and stability to the knee joint.
While surgical treatment of the ACL can be highly effective in restoring function to the knee joint, it does carry some risks, such as infection, blood clots, and nerve damage. It is necessary for patients to properly discuss these risks with their surgeon before undergoing the procedure.
Conservative treatment
Conservative treatment of the ACL involves non-surgical methods to manage the injury and promote healing. This approach is typically recommended for patients who have a partial tear or a mild to moderate sprain of the ACL, as well as those who may not be good candidates for surgery due to other health conditions.
The main components of conservative treatment for ACL injuries include:
- Rest: The first step in treating an ACL injury is to rest the knee and avoid activities that may cause further damage. This may involve using crutches to take weight off the knee and limiting physical activity for a period of time.
- Ice: Applying ice to the knee can help reduce swelling and inflammation, which are common symptoms of an ACL injury. Ice application should be for 20-30 minutes at a time, several times per day.
- Compression: Wearing a compression bandage or brace can help support the knee and reduce swelling. These devices should be worn as directed by a healthcare provider.
- Elevation: Elevating the leg above the heart level can also help reduce swelling and promote healing.
- Physical therapy: A physical therapist can work with patients to develop an exercise program that helps improve the range of motion, strength, and stability of the knee joint. This may include exercises to strengthen the quadriceps and hamstrings, as well as balance and agility training.
- Medications: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, may be recommended to manage pain and inflammation.
Conservative treatment for ACL injuries typically takes several weeks to several months, depending on the severity of the injury and the individual’s response to treatment. While this approach may not completely restore function to the knee joint, it can help reduce pain and improve mobility, allowing patients to return to their normal activities over time.
Physiotherapy treatment
Physiotherapy exercises for ACL (Anterior Cruciate Ligament) are an important part of the rehabilitation process. These exercises help to restore the strength, range of motion, and stability of the knee joint. Here are some physiotherapy exercises for ACL in detail:
Range of Motion Exercises
Range of motion exercises helps to improve the flexibility and mobility of the knee joint. These exercises include:
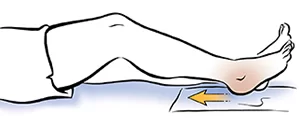
- Heel Slides: Lie on your back with your legs should be straight. Slowly bend your injured knee and slide your heel towards your buttocks. Hold for a few seconds and then slowly straighten your leg. Repeat 10 times.
- Knee Flexion Stretch: Sit on a chair with your feet flat on the ground. Slowly slide your injured foot back until you feel a stretch in your knee. maintain for a few seconds and then back to the initiate position. Repeat 10 times.
- Knee Extension Stretch: Sit on a chair with your feet flat on the ground. Straighten your injured leg and lift it off the ground. maintain for some seconds and then lower your leg back down. Repeat 10 times.
Strengthening Exercises
Strengthening exercises help to rebuild the strength of the muscles around the knee joint. These exercises include:

- Straight Leg Raises: Lie on your back with your legs straight. Slowly lift your injured leg off the ground and hold for a few seconds. Lower your leg back down and do it again 10 times.
- Wall Squats: Stand with your back opposite to a wall and your feet shoulder-width away. Slowly bend your knees and slide down the wall until your thighs are parallel to the ground. Hold for a few seconds and then push back up to the starting position. Repeat 10 times.
- Hamstring Curls: Lie on your stomach with a pillow beneath your hips. Bend your injured knee and lift your heel towards your buttocks. maintain for some seconds and then lower your leg back down. Repeat 10 times.
Balance and Proprioception Training
Balance and proprioception training help to improve the stability of the knee joint. These exercises include:

- Single Leg Stance: Stand on your injured leg with your other foot off the ground. Hold for a few seconds and then switch to the other leg. Repeat 10 times.
- Bosu Ball Squats: Stand on a Bosu ball with your feet shoulder-width away. Slowly bend your knees and squat down. Hold for a few seconds and then push back up to the starting position. Repeat 10 times.
- Walking on Uneven Surfaces: Walk on uneven surfaces such as grass, sand, or gravel to challenge your balance and coordination.
Gait Training
Gait training involves teaching the patient how to walk properly with their injured knee. These exercises include:
- Heel-to-Toe Walking: Walk in a straight line placing your heel directly in front of your toes on each step.
- Sidestepping: Walk sideways with your injured leg leading and then switch to the other side.
- Crossover Steps: Walk forward crossing one foot over the other with each step.
Functional Training
Functional training involves simulating real-life activities that the patient may encounter after recovery. These exercises include:
- Jumping: Jump over cones or small hurdles to improve your jumping ability.
- Running: Start with slow jogging and gradually increase your speed.
- Cutting and Pivoting: Practice cutting and pivoting movements to prepare for sports that involve sudden changes of direction.
In conclusion, physiotherapy exercises for ACL are an essential part of the rehabilitation process. These exercises help to restore the strength, range of motion, and stability of the knee joint. The physiotherapist will develop an individualized exercise program based on the patient’s specific needs and goals. It is important to follow the exercise program consistently and to communicate with the physiotherapist about any pain or discomfort during the exercises.
Risk factors of the anterior cruciate ligament injury
The ACL (Anterior Cruciate Ligament) is one of the four major ligaments in the knee joint. It connects the femur (thigh bone) to the tibia (shin bone) and is responsible for stabilizing the knee during movement. However, the ACL is also susceptible to injury, particularly in athletes who participate in high-impact sports such as soccer, basketball, and football. Here are some risk factors of ACL injury in detail:
- Gender: Females are at a higher risk of ACL injury compared to males. This is because females tend to have a wider pelvis and a smaller notch in the femur, which can lead to an increased angle between the thigh bone and shin bone, putting more stress on the ACL.
- Age: ACL injuries are more common in younger individuals, particularly adolescents and young adults. This is because their bones and muscles are still developing, making them more susceptible to injury.
- Sports Participation: Athletes who participate in high-impact sports such as soccer, basketball, and football are at a higher risk of ACL injury. These sports involve sudden stops, starts, and changes of direction, which can put stress on the knee joint.
- Previous Injury: ACL injuries that have already occurred are more likely to occur again in those people. This is because the ligament may not have fully healed or may be weakened from the previous injury.
- Poor Conditioning: Individuals who are not physically fit or have poor muscle strength and flexibility are at a higher risk of ACL injury. This is because weak muscles can’t support the knee joint properly, leading to increased stress on the ligaments.
- Footwear: Wearing improper footwear, such as shoes that do not provide adequate support or traction, can increase the risk of ACL injury.
- Playing Surface: Playing on surfaces that are too hard or too soft, such as concrete or sand, can increase the risk of ACL injury.
In the end, there are several risk factors for ACL injury, including gender, age, sports participation, previous injury, poor conditioning, footwear, and playing surface. It is important to take steps to reduce these risk factors, such as maintaining good physical fitness, wearing proper footwear, and playing on safe surfaces. Additionally, if an ACL injury does occur, seeking prompt medical attention and following a rehabilitation program can help to prevent further damage and promote healing.
How to prevent the anterior cruciate ligament injury
Preventing ACL injuries involves a combination of measures that address the risk factors discussed above. Here are some ways to prevent ACL injuries:
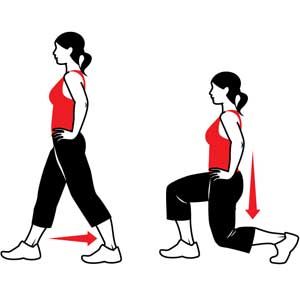
- Strengthening exercises: Strengthening the muscles around the knee joint, particularly the quadriceps and hamstrings, can help to support the knee and reduce the stress on the ACL. Exercises such as squats, lunges, and leg presses can be helpful.
- Flexibility exercises: Stretching exercises can help to improve flexibility and range of motion in the knee joint, reducing the risk of injury. Examples involve calf stretches, hamstring stretches, and quad stretches.
- Proper footwear: Wearing shoes that provide adequate support and traction can help to reduce the risk of ACL injury. Shoes with good arch support and a non-slip sole are recommended.
- Safe playing surface: Playing on safe surfaces such as grass or turf can help to reduce the risk of ACL injury. Avoid playing on hard or uneven surfaces such as concrete or sand.
- Proper technique: Using proper technique when playing sports can help to reduce the stress on the knee joint and decrease the risk of ACL injury. Coaches and trainers can provide guidance on proper technique.
- Protective gear: Wearing protective gear such as knee pads or braces can help to reduce the risk of ACL injury, particularly for athletes who have previously suffered an ACL injury.
- Rest and recovery: Taking time to rest and recover after intense physical activity can help to prevent overuse injuries such as ACL injuries. Adequate rest, hydration, and nutrition are important for overall health and injury prevention.
To conclude, preventing ACL injuries requires a multi-faceted approach that addresses the various risk factors involved. By following these preventative measures, individuals can reduce their risk of ACL injury and maintain good knee health.
FAQ
An ACL injury is typically diagnosed through a physical exam, including the anterior drawer test, and imaging tests such as MRI or X-ray.
Symptoms of an ACL injury may include pain, swelling, instability or a feeling of giving way in the knee, and difficulty walking or bearing weight on the affected leg.
Treatment for an ACL injury may include rest, ice, compression, and elevation (RICE), physical therapy, bracing, and in some cases, surgery to repair or reconstruct the ligament.
While it is not always possible to prevent an ACL injury, certain measures such as proper warm-up and stretching, using proper technique during sports or exercise, and wearing appropriate protective gear can help reduce the risk of injury.


5 Comments