Knee Joint Biomechanics
Table of Contents
What is knee joint biomechanics?
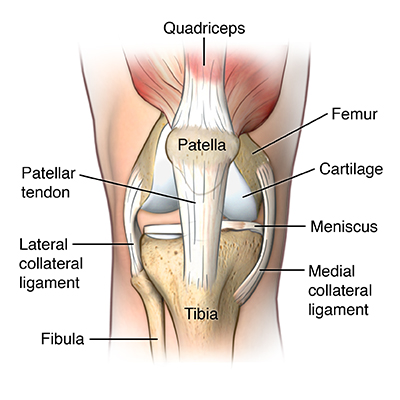
- A knee joint biomechanics- studies the coordination of the bones, muscles, ligaments, as well as tendons in Knee joint motions. A complex interaction of these structures allows a knee to withstand tremendous forces while various normal motions.
- The knee joint is the largest & one of the most complex joints in the human body. This is positioned between the hip & ankle joints, as well as this position makes it highly vulnerable to damage owing to the high moments that may be generated by the two long lever arms (femur and tibia) of adjacent joints. This is, hence, not surprising that the knee joint is one of the most frequently damaged, not only in terms of bone fracture but also in terms of soft tissue injuries (ligaments as well as cartilage).
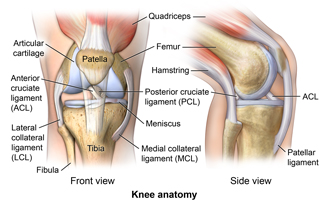
- Even though a knee joint is a single structure, from the practical point of view, this may be considered to be composed of two main joints: a tibiofemoral joint, which is a joint between a distal femur as well as a proximal tibial, & a patellofemoral joint, which is the joint between a posterior part of a patella & the femoral trochlear groove.
- However, from the biomechanical as well as functional point of view, this is more appropriate to consider a knee joint being composed of three joints, further subdividing a tibiofemoral joint into a medial & lateral tibiofemoral joint characterized by different shapes, different kinematics, & different relative kinetics.
- Overall, the kinematics of a knee is the complex three-dimensional roto-translational movement that is strongly related to a patient’s anatomy. In particular, the shape of the femoral condyles, a tibial plateau, as well as a patellar bone, & the morphological and mechanical properties & position of the soft tissue envelope are critical to producing this motion. For these reasons, knee kinetics, as well as kinematics, vary from individual to individual.
- A knee can be conceptualized as two joints, the tibiofemoral & the patellofemoral joint. A tibiofemoral joint allows transmission of the body weight from a femur to a tibia while providing hinge-like, sagittal plane joint rotation along with a small degree of tibial axial rotation.
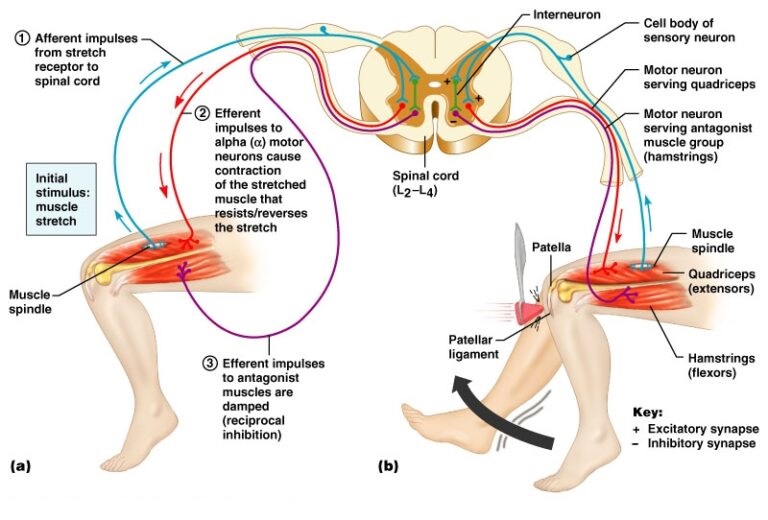
Functionally, the quadriceps muscle group & patellofemoral articulation along with a tibialis anterior as well as ankle joint act to dissipate forward momentum as the body enters a stance phase of a gait cycle.
Articulating Surfaces
- A knee joint consists of two articulations – tibiofemoral as well as patellofemoral. The joint surfaces are lined with hyaline cartilage & are enclosed within the single joint cavity.
- Tibiofemoral: Medial as well as lateral condyles of a femur articulate with the tibial condyles. This is the weight-bearing component of a knee joint.
- Patellofemoral: Anterior aspect of a distal femur articulates with a patella. This allows a tendon of the quadriceps femoris (knee extensor) to be inserted directly over a knee increasing an efficiency of a muscle.
- A patellofemoral articulation is commonly referred to as an extensor mechanism. Even though true that a concentric action of the motor unit is an extension of a knee, functionally, the quadriceps acts eccentrically while gait, running, or even jumping. Even though this is thought of less as the focus of treatment, the extensor mechanism can be involved in instances of knee dislocation, such as a buttonholing of a lateral femoral condyle through a lateral retinaculum that happens in the posterolateral dislocation or in the tears of the vastus medialis obliquus & vastus medialis that can happen with a capsular ligament injury.
- Moreover, the knowledge of a response of a plica or fat pad to injury assists to prepare a surgeon to deal with secondary sequelae of the knee dislocation.
- As a patella is both formed & resides within the quadriceps femoris tendon, this provides the fulcrum to increase the power of a knee extensor & serves as a stabilizing structure that decreases frictional forces placed on femoral condyles.
Menisci

- There are two menisci in the space between femoral & tibial condyles, which are crescent-shaped lamellae, each with the anterior & posterior horn, as well as they are triangular in cross-section. The surface of each meniscus is concave superiorly, providing a congruous surface to femoral condyles as well as it is flat inferiorly to accompany the relatively flat tibial plateau. The horns of the medial meniscus are further apart & meniscus appears ‘C’ shaped, than those of the lateral one where the meniscus appears more ‘O’ shaped. This is due to the increased size of the medial meniscus, which unfortunately leaves a large exposed part that in turn may be prone to injury.
- Menisci correct the lack of congruence between articular surfaces of a tibia & the femur increases a part of contact & increases weight distribution as well as shock absorption. They also assist to guide and coordinating knee movement making them very essential stabilizers of a knee.
- The arrangement of the fibers in menisci allows for axial loads to be dispersed radially reducing wear on hyaline articular cartilage. This is mandatory as the compressive load through the knee may reach 1-2 times body weight while gait as well as stair climbing & the astonishing 3-4 times body weight while running. Menisci are connected with the tibia by coronary ligaments. The medial meniscus is much less mobile during joint motion than the lateral meniscus because of in large part its firm attachment to the knee joint capsule & medial collateral ligament (MCL). On the lateral side, the meniscus is less firmly attached to the joint capsule as well as has no attachment to the lateral collateral ligament (LCL). In fact, the pThen of the lateral meniscus is separated entirely from the rolateral aspect of a knee joint capsule by the tendon of a popliteus muscle as it descends from a lateral epicondyle of the femur.
- During the first year of life, the menisci are fully vascularized but once weight-bearing commences vascularity diminishes to the outer third (red zone), the red zone being the only part having a slight ability to heal. The inner non-vascularized part (white zone) receives nutrition through the diffusion of synovial fluid in a knee joint.
Bursae of the Knee joint
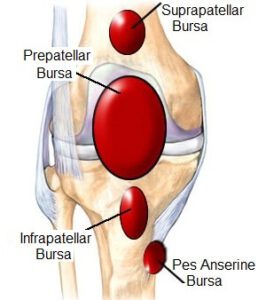
- The bursa is a synovial fluid-filled sac, found between moving structures in the joint to decrease as tears on those structures. There are four bursae found in a knee joint:
- Suprapatellar bursa: An extension of a synovial cavity of a knee, located between the quadriceps femoris as well as the femur.
- Prepatellar bursa: Found between an apex of a patella & the skin.
- Infrapatellar bursa: Split into deep as well as superficial. A deep bursa lies between a tibia & the patella ligament. A superficial lies between a patella ligament & the skin.
- Semimembranosus bursa: Located posteriorly in a knee joint, between a semimembranosus muscle & a medial head of the gastrocnemius.
Ligaments of the Knee joint
- The major ligaments in a knee joint are:
- Patellar ligament: The continuation of the quadriceps femoris tendon distal to a patella. This attaches to a tibial tuberosity.
- Collateral ligaments: Two strap-like ligaments, which act to stabilize a hinge motion of a knee, preventing excessive medial or even lateral movement.
- Tibial (medial) collateral ligament: Wide as well as flat ligament, found on the medial side of the joint. Proximally, this attaches to a medial epicondyle of a femur, distally it attaches to a medial condyle of the tibia.
- Fibular (lateral) collateral ligament: Thinner & rounder than tibial collateral, it attaches proximally to a lateral epicondyle of a femur, distally this attaches to the depression on a lateral surface of a fibular head.
- Cruciate Ligaments: These two ligaments connect a femur & a tibia. In doing so, they cross each other, thus term ‘cruciate’ (Latin for like a cross)
- Anterior cruciate ligament: Attaches at an anterior intercondylar region of a tibia where it blends with a medial meniscus. This ascends posteriorly to attach to a femur in an intercondylar fossa. This prevents anterior dislocation of a tibia onto a femur.
- Posterior cruciate ligament: Attaches at a posterior intercondylar region of a tibia & ascends anteriorly to attach to an anteromedial femoral condyle. This prevents posterior dislocation of a tibia onto a femur.
Movements of the Knee Joint
There are four main movements that a knee joint permits:
- Extension: Produced by a quadriceps femoris, which inserts into a tibial tuberosity.
- Flexion: Produced by the hamstrings, gracilis, sartorius as well as popliteus.
- Lateral rotation: Produced by a biceps femoris.
- Medial rotation: Produced by five muscles; semimembranosus, semitendinosus, gracilis, sartorius as well as popliteus.
Locking of the knee joint
- Closed kinematic chain extension from 30-degree knee flexion.
- A larger medial femoral condyle continue rolling & gliding posteriorly when the smaller lateral side stopped. This results in medial rotation of a femur on the tibia, in the last 5 degrees of an extension. The medial rotation of the femur at the final stage of extension is not voluntary or even produced by muscular force, which is referred to as “Automatic” or “Terminal Rotation”.
- The rotation within a knee joint brings the joint into a closed packed or locked position. The consequences of automatic rotation are also known as “locking mechanism” or “screw home mechanism.”
- Open kinematic chain: Lateral rotation of a tibia on a femur.
True Knee Locking
- True locking at the knee is where a knee gets physically stuck as well as a patient physically cannot move a knee for a person timeue knee locking is caused by a mechanical block where something gets caught inside a knee joint, preventing movement.
- A truly locked knee is fairly rare and typically happens as a patient moves the knee into full extension, for instance towards being fully straight.
Pseudo Knee Locking
- Pseudo-knee locking is much more common than true locking, & knee motion is limited by temporary muscle spasming as the body tries to protect itself in response to pain.
Unlocking the knee
- To initiate flexion, a knee should be unlocked.
- A flexion force will automatically result in a lateral rotation of the femur.
- Owing to the larger medial condyle will move before the shorter lateral condyle.
- Popliteus is the primary muscle to unlock a knee.
Muscle of the Knee joint
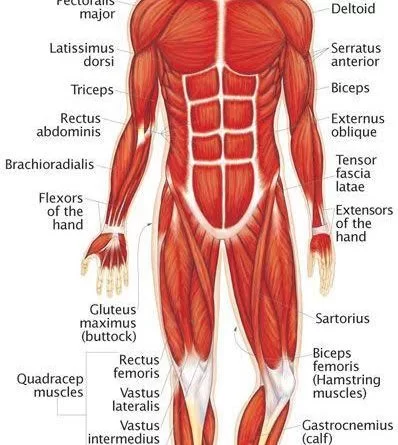
Extensors muscle of a knee:
- Articularis genus muscle
Origin: Distal end of an anterior femoral shaft.
Insertion: Proximal extension of the knee joint capsule.
Blood supply: Femoral artery.
Nerve supply: Femoral nerve.
Action: Pulling the suprapatellar bursa while an extension of a knee. - Quadriceps femoris muscle
Origin: Intertrochanteric line, greater trochanter, gluteal tuberosity, & linea aspera of a femur.
Insertion: Patella & Tibial tuberosity via a Patellar ligament.
Blood supply: Femoral artery.
Nerve supply: Femoral nerve.
Action: Extension of the knee; flexion of the hip (rectus femoris only).
Antagonist: Hamstring muscle.
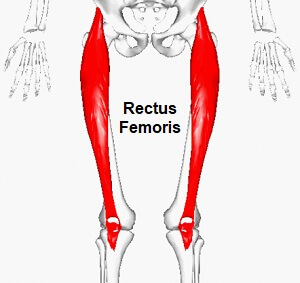
- Rectus femoris
Origin: Anterior inferior iliac spine as well as an exterior surface of the bony ridge which forms the iliac portion of an acetabulum.
Insertion: Patella & Tibial tuberosity via a Patellar ligament.
Blood supply: Femoral artery.
Nerve supply: Femoral nerve.
Action: Extension of a knee & flexion of a hip.
Antagonist: Hamstring muscle. - Vastus lateralis
Origin: Greater trochanter, Intertrochanteric line, as well as linea aspera of a femur.
Insertion: Patella & tibial tuberosity via a patellar ligament.
Blood supply: Femoral artery.
Nerve supply: Femoral nerve.
Action: Extends & stabilizes a knee.
Antagonist: Hamstring muscle. - Vastus intermediates
Origin: Superior 2/3 of anterior & lateral surfaces of a femur; also from a lateral intermuscular septum of a thigh.
Insertion: Lateral border of the patella; & forms a deep portion of the quadriceps tendon.
Nerve supply: Muscular branches of a femoral nerve.
Blood supply: Lateral circumflex femoral artery.
Action: Extension of a knee
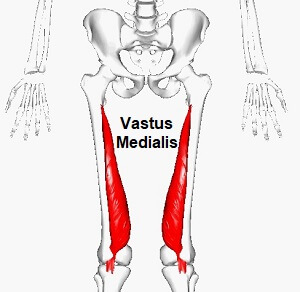
- Vastus medialis
Origin: Lower part of the intertrochanteric line, along with a spiral line to a medial lip of the linea aspera, the medial intermuscular septum & the aponeurosis of adductor Magnus.
Insertion: Into the medial side of the quadriceps tendon, joining with rectus femoris & the other quadriceps muscles, enveloping the patella, then by the patellar ligament into a tibial tuberosity.
Blood supply: Femoral artery.
Nerve supply: Femoral nerve.
Action: Extension of the knee.
Antagonist: Hamstring muscle.
Flexors of the Knee joint
Posterior compartment:
- Sartorius
Origin: Anterior superior iliac spine(ASIS) of a pelvis.
Insertion: Pes anserinus.
Blood supply: Superficial circumflex iliac artery, lateral femoral artery, deep femoral artery, descending geniculate artery, & the femoral artery.
Nerve supply: Femoral nerve.
Action: At the hip joint: flexion, lateral rotation & abduction. At a knee joint: flexion & medial rotation.
Antagonist: Quadriceps muscle (partly).
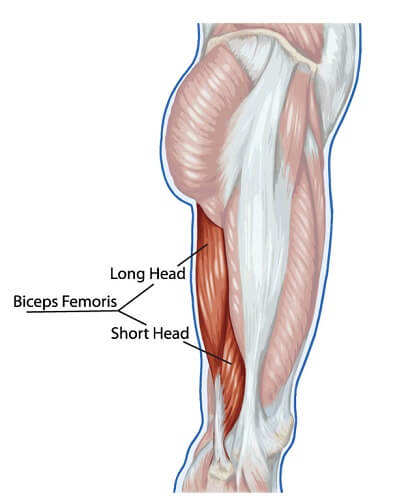
- Biceps femoris
Origin: Long head: Tuberosity of the ischium, short head: linea aspera on the femur.
Insertion: A head of the fibula articulates with the back of the lateral tibial condyle.
Blood supply: Inferior gluteal artery, perforating arteries, & popliteal artery.
Nerve supply: Long head: medial (tibial) part of a sciatic nerve, short head: the lateral (common fibular) part of a sciatic nerve.
Action: Flexion of a knee, laterally rotates leg at a knee (when the knee is in flexion), extends hip joint (long head only).
Antagonist: Quadriceps muscles. - Semitendinosus
Origin: Posteromedial impression of an Ischial tuberosity.
Insertion: Proximal end of a tibia below medial condyle via pes anserinus.
Action: At the hip joint: Thigh extension, thigh internal rotation, & stabilizes a pelvis, At a knee joint: Leg flexion, leg internal rotation.
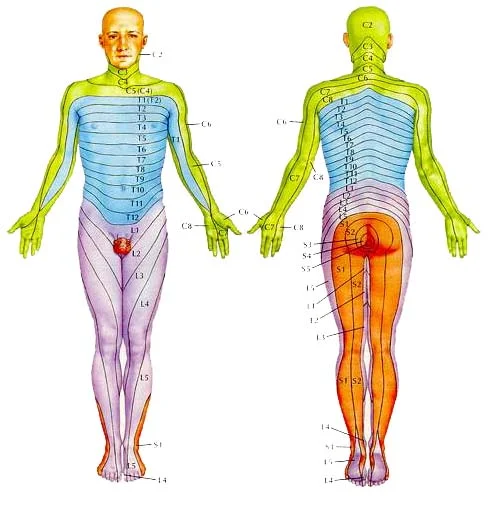
Nerve supply: Tibial division of sciatic nerve (L5-S2).
Blood supply: First perforating branch of a deep femoral artery, medial femoral circumflex artery, inferior gluteal artery & the inferior medial geniculate artery. - Semimembranosus
Origin: Superolateral impression of an ischial tuberosity.
Insertion: Medial condyle of a tibia bone.
Action: At hip joint: Thigh extension & internal rotation.
Knee joint: Flexion, & internal rotation of a leg, stabilizes a pelvis.
Nerve supply: Tibial division of the sciatic nerve (L5 – S2)
Blood supply: Perforating branches of femoral & popliteal arteries as well.

- Gastrocnemius
Origin: Lateral head: Posterolateral aspect of a lateral condyle of the femur. Medial head: Posterior surface of a medial femoral condyle, the popliteal surface of a femoral shaft.
Insertion: Posterior surface of the calcaneus via a calcaneal tendon.
Nerve supply: Tibial nerve (S1, S2).
Action: Talocrural joint: Foot plantar flexion & Knee joint: Leg flexion. - Plantaris
Origin: Lateral supracondylar line of a femur, oblique popliteal ligament of a knee.
Insertion: Posterior surface of a calcaneus via the calcaneal tendon.
Action: Talocrural joint: Foot plantar flexion & Knee joint: knee flexion.
Nerve supply: Tibial nerve (S1, S2).
Blood supply: Superficially: Lateral sural & popliteal arteries as well as Deeply: Superior lateral genicular artery. - Popliteus
Origin: Lateral condyle of a femur, posterior horn of a lateral meniscus of a knee joint.
Insertion: Posterior surface of a proximal tibia.
Nerve supply: Tibial nerve (L4-S1).
Blood supply: Inferior medial & lateral genicular arteries (popliteal artery), posterior tibial recurrent artery, posterior tibial
artery, nutrient artery of a tibia as well.
Action: Unlocks a knee joint; Knee joint stabilization.
Medial compartment:
Gracilis
Origin: Anterior body of a pubis, inferior pubic ramus, ischial ramus.
Insertion: Medial surface of a proximal tibia via pes anserinus.
Action: At the hip joint: Thigh flexion, thigh adduction; At a knee joint: leg flexion, leg internal rotation.
Nerve supply: Obturator nerve (L2-L3).
Blood supply: Deep femoral artery via artery to the adductors.
Function
Osteokinematics
- The ligaments, & menisci, provide static stability as well as the muscles & tendon dynamic stability.
- The main movement of a knee is flexion & extension. For that matter, a knee act as a hinge joint, whereby the articular surface of a femur roll and glide over a tibial surface. While a flexion as well as the extension of a knee, tibia & patella act as one structure in relation to a femur. The quadriceps muscle group is made up of 4 different individual muscles.
- They join together forming one single tendon that inserts into the anterior tibial tuberosity. Embedded in the tendon is the patella, a triangular sesamoid bone, as well as its function, is to improve the efficiency of the quadriceps contractions. Contraction of the quadriceps pulls the patella upwards & extends a knee.
Range of motion of Knee joint
- Knee extension 0 degrees. The hamstring muscle group consists of the biceps femoris, semitendinosus as well as semimembranosus. They are situated at the back of a thigh as well as their function is flexing or even bending a knee & providing stability on either side of a joint line. Range of motion: Knee flexion 135 degrees.
- Secondary movement is internal & external rotation of the tibia in relation to the femur, but it is possible only when the knee is flexed.
Extended position
- With the knee extended, both lateral & medial collateral ligaments, as well as an anterior part of the anterior cruciate ligament, is taut.
- During extension, the femoral condyles glide as well as roll into a position that causes the complete unfolding of the tibial collateral ligament.
- While the last 10 degrees of extension, an obligatory terminal rotation is triggered in which the knee is rotated medially 5 degrees. A final rotation is produced by a lateral rotation of the tibia in a non-weight-bearing leg, and by a medial rotation of the femur in a weight-bearing leg. A terminal rotation is made possible by the shape of a medial femoral condyle, assisted by the contraction of a popliteus muscle as well as the iliotibial tract & is caused by a stretching of the anterior cruciate ligament. Both cruciate ligaments are slightly unwinded as well as both lateral ligaments become taut.
Flexed position
- In a flexed position, collateral ligaments are relaxed while the cruciate ligaments are taut. Rotation is controlled by twisted cruciate ligaments; the two ligaments get twisted around each other whilst a medial rotation of the tibia which reducing the amount of rotation possible while they become unwound during lateral rotation of the tibia. Because of the oblique position of cruciate ligaments, at least part of one of them is always tense as well as these ligaments control the joint as the collateral ligaments are relaxed.
- Moreover, the dorsal fibers of the tibial collateral ligament become tensed while extreme medial rotation, as well as a ligament, also reduces a lateral rotation to 45–60 degrees.
Arthrokinematics
- Viewed in the sagittal plane, an articulating surface of a femur is convex whereas an articulating surface of a tibia is concave. The knee arthrokinematics is based on the rules of concavity & convexity as well as is described in terms of open & closed chain:
- Open kinetic chain: While the knee extension, a tibia glides anteriorly on a femur. More precisely, from 20 degrees knee flexion to full extension, a tibia rotates externally. While a knee flexion, a tibia glides posteriorly on a femur & from full knee extension to 20 degrees flexion, a tibia rotates internally.
- Closed kinetic chain: While knee extension, a femur glides posteriorly on a tibia. To be more specific, from 20 degrees knee flexion to full extension, while that time the femur rotates internally on a stable tibia. While knee flexion, a femur glides anteriorly on a tibia, and from full knee extension to 20 degrees flexion, the femur rotates externally on the stable tibia.
- The “screw home mechanism”
- The “screw-home” mechanism, considered to be a key element to knee stability, is the rotation between a tibia & the femur. It occurs at the end of a knee extension, between full extension (0 degrees) & 20 degrees of the knee flexion. A tibia rotates internally while an open-chain motions (swing phase) & externally while a closed-chain movement (stance phase). The external
- rotation occurs during a terminal degree of a knee extension and results in a tightening of both cruciate ligaments, which locks a knee. The tibia is then in the position of maximal stability with respect to the femur.