Anterior Cruciate Ligament Injury: Physiotherapy Treatment
Table of Contents
Anterior cruciate ligament injury definition
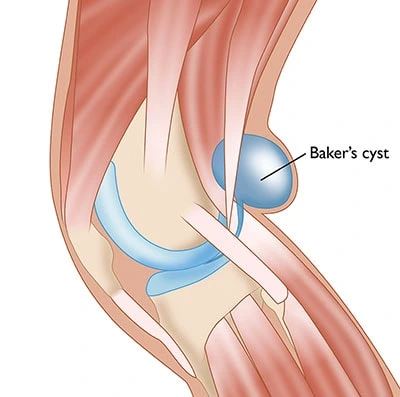
Anterior cruciate ligament injury is a tear or sprain of the anterior cruciate ligament (ACL) which one of the strong bands of tissue that help connect your femur to your tibia.
Sportsman who participate in high knee jerk’s movement related sports like Hockey, soccer, football, and basketball are more likely to injure their anterior cruciate ligaments. ACL injuries most commonly occur during sports that involve sudden stops or changes in direction, jumping and landing.
The anterior cruciate ligament (ACL) is one of four ligaments critical to stabilizing the knee joint. A ligament is made of tough fibrous material and functions to control excessive motion by limiting joint mobility. Of the four major ligaments of the knee, the ACL is the most frequently injured. When you have an injury to your ACL it often feels like the knee is “giving out.”
Depending on the grade of your ACL injury, treatment may include RICE Principle (Rest, Ice, Compression, Elevation) – Initially rest and after few days rehabilitation exercises to help you regain strength and mobility or surgery is the last option to replace the torn ligament followed by rehabilitation exercise.
A proper Physiotherapy exercise training program may help reduce the risk of an ACL injury.
Anatomy of Anterior cruciate ligament
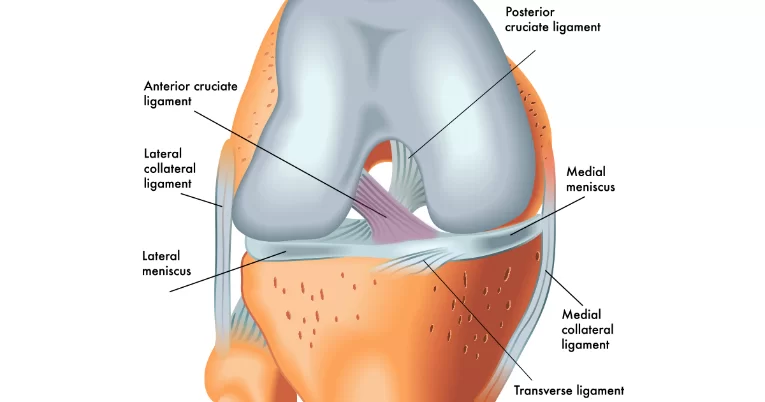
~ The ACL is a band of dense connective tissue which courses from the femur to the tibia and considered a key structure in the knee joint, as it resists anterior tibial translation and rotational loads.
~ The ACL arises from the posteromedial corner of medial aspect of lateral femoral condyle in the intercondylar notch and inserted anterior to the intercondyloid eminence of the tibia, blending with the anterior horn of the medial meniscus. The ACL courses anteriorly, medially, and distally across the joint as it passes from the femur to the tibia. As it does, it turns on itself in a slight outward (lateral) spiral.
~ There are two components of the ACL, the smaller anteromedial bundle (AMB) and the larger posterolateral bundle (PLB), named according to where the bundles insert into the tibial plateau. When the knee is extended the PLB is tight, while the AMB is moderately lax. However, as the knee is flexed, the femoral attachment of the ACL assumes a more horizontal orientation, causing the AMB to tighten and the PLB to loosen and thus leave the AMB as the restraint to anterior tibial load.
Mechanism ACL Ligament
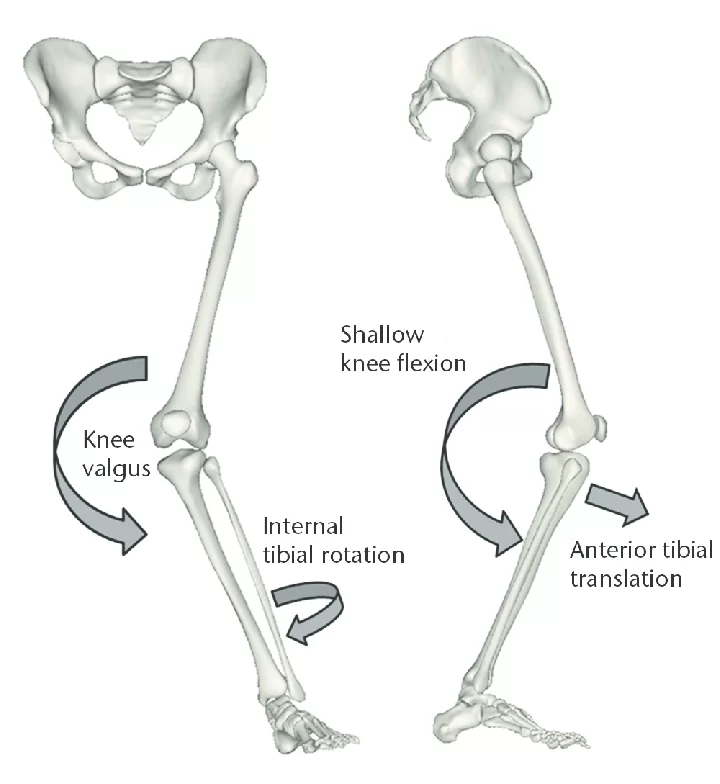
The ACL is to resist the motions of anterior tibial translation and internal tibial rotation; this is important in order to have rotational stability. This function prevents anterior tibial subluxation of the lateral and medial tibiofemoral joints, which is important for the pivot-shift phenomena.
The ACL has been proven to have mechanoreceptors that detect changes in direction of movement, position of the knee joint, changes in acceleration, speed, and tension. A key factor in instability after ACL injuries is having altered neuromuscular function secondary to diminished somatosensory information. For athletes who participate in sports involving cutting, jumping, and rapid deceleration it is important for the knee to be stable in terminal extension, which is the screw-home mechanism
Symptoms of ACL Injury
A loud “pop” or a “popping” sensation in the knee joint.
- Severe Knee pain and inability to continue activity
- Rapid swelling
- Loss of range of motion
- A feeling of instability or “giving way” with weight bearing
Grades of ACL Injury
When a ligament is injured, it is called a sprain. For the ACL, it is graded from 1 to 3:
- Grade 1 ACL injury: A grade 1 injury is a sprain. The ligament has mild damage and the knee joint is still stable.
- Grade 2 ACL injury: A grade 2 ACL sprain is a partial tear with the ligament stretched and damaged.
- Grade 3 ACL injury: A grade 3 sprain is a complete tear of the ligament and it is the most common type of ACL injury. Typically people with complete tears of the ACL consider surgical intervention for their injury.
Which are causes of Anterior cruciate ligament injury?
The anterior cruciate ligament can be injured in several ways :
- Changing direction rapidly
- Stopping suddenly
- Slowing down while running
- Landing from a jump incorrectly Direct contact or collision, such as a football tackle
Several studies have shown that female athletes have a higher incidence of ACL injury than male athletes in certain sports. It has been proposed that this is due to differences in physical conditioning, muscular strength, and neuromuscular control. Other suggested causes include differences in pelvis and lower extremity (leg) alignment, increased looseness in ligaments, and the effects of estrogen on ligament properties.
RISK FACTOR
There are a number of factors that increase your risk of an ACL injury, including:
- Being female — possibly due to differences in anatomy, muscle strength and hormonal influences
- Participating in certain sports, such as soccer, football, basketball, gymnastics and downhill skiing
- Poor conditioning
- Wearing footwear that doesn’t fit properly
- Using poorly maintained sports equipment, such as ski bindings that aren’t adjusted properly
- Playing on artificial turf surfaces
Diagnosis
- X-rays : X-rays may be needed to rule out a bone fracture. However, X-rays don’t show soft tissues, such as ligaments and tendons.
- Magnetic resonance imaging (MRI) : An MRI uses radio waves and a strong magnetic field to create images of both hard and soft tissues in your body. An MRI can show the extent of an ACL injury and signs of damage to other tissues in the knee, including the cartilage.
- Ultrasound : Using sound waves to visualize internal structures, ultrasound may be used to check for injuries in the ligaments, tendons and muscles of the knee.
2. SPECIAL TEST
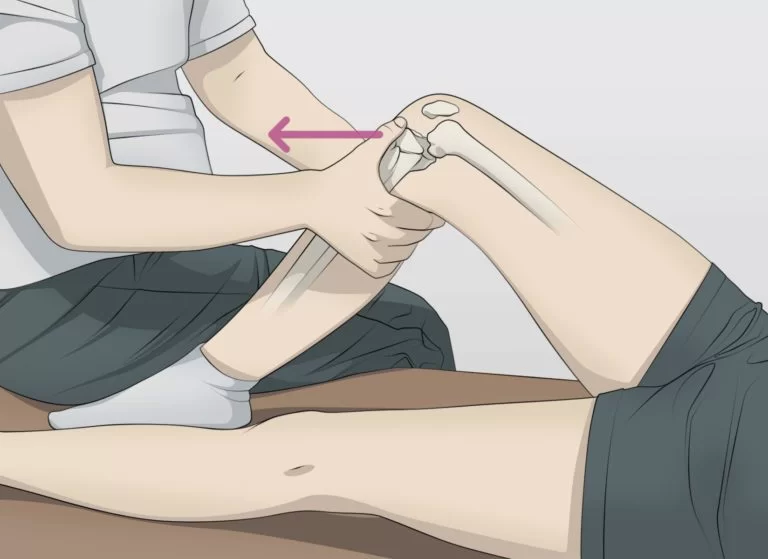
Anterior Drawer Test
The test is performed by lying down on your back with your knee bent. Another person grasps your tibia just behind your knee and gently pulls forward. Excessive motion of your tibia underneath your femur indicates a positive test and an ACL tear may be suspected.
Treatment for anterior cruciate ligament injury
Medical Treatment
- 1. Anti-inflammatory drugs can help to reduce swelling and pain.
- 2. Knee brace: Some people with a damaged ACL can get by wearing a brace on their knee when they run or play sports. It provides extra support.
- 3. inject your knee with steroid
Surgery for Anterior cruciate ligament injury
ACL RECONSTRUCTION
~ Your surgeon will remove your damaged ligament, and then replace it with a segment of tendon. This replacement tissue is called a graft and it comes from another part of your knee or a tendon from a deceased donor.
~ Your surgeon will drill sockets or tunnels into your thighbone and shinbone to accurately position the graft, which is then secured to your bones with screws or other fixation devices. The graft will serve as scaffolding on which new ligament tissue can grow.
Physiotherapy Treatment for Anterior cruciate ligament injury
Use of RICE Principles :
- Rest: Rest is important to relieve pain. Knee movement will aggravate your symptom’s.
- Ice Pack: When you’re awake, try to ice your knee at least every two hours for 20 minutes at a time.
- Compression: Wrap an elastic bandage or compression wrap around your knee.
- Elevation: Lie down with your knee propped up on pillows.
Ultrasound Therapy :
Ultrasound devices creates vibrations through the soft tissue increase the heat within the Ultrasound and Electrotherapy for ACL Rehabilitation tissue, which increases blood flow and reduces pain. The heat produced also relaxes muscles and improves the ability of soft tissues to stretch.
TENS (Transcutaneous Electrical Stimulation):
TENS works in two ways; 1. providing stimulation that the body responds differently than it would to pain and 2. Artificially making the muscle contract breaking up the spasm cycle. Research has shown that electrical stimulation coupled with exercise post ACL reconstruction increased range of motion for both extension and flexion of the knee.
Low Level Laser Therapy (LLLT) :
Using short wavelengths of light (600-1000 nm) which penetrates the tissue, LLLT facilitates the healing of tissue, reducing both pain and swelling. In a study published in Photomedicine and Laser Surgery, results showed that LLLT improved healing and tensile strength of the medial ligament.
Whirlpool Therapy
After the wounds of the ACL reconstruction have healed, hydrotherapy in the form of Whirlpool therapy can be useful to reduce pain and increase range of motion. ROM exercises performed while a patient is in a cold whirlpool can help increase motion for the knee.
Exercises for Anterior cruciate ligament injury :
1.PRIMARY GOALS OF BEFORE SURGERY ACL :

Restore normal function and strength to your quadriceps muscle so that it supports your knee properly.
Quad setting exercises :
Lie on your back and place a small towel under your knee. Tighten your quads by pressing the back of your knee into the towel. Hold for 5 seconds, and then relax.
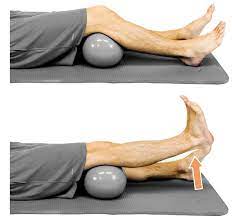
Short arc quads (SAQ)
Lie on your back and place a ball underneath your knee. Straighten your knee fully, keeping the back of your knee against the ball.
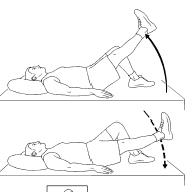
Straight leg raises :
Tighten your quad muscle on the top of your thigh and then slowly lift your straight leg up about 12 to 15 inches. Hold for 2 seconds, and then slowly lower your leg down.
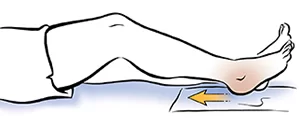
Heel slides
Lie on your back and slowly bend your knee and slide your heel up towards your buttocks.
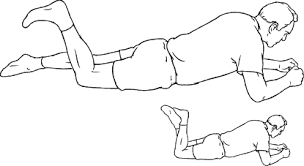
Prone knee bends
Lie on your stomach and slowly bend your injured knee up, using your hamstring on the back of your thigh.
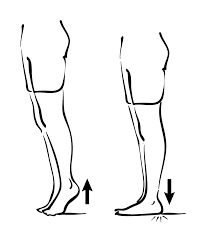
Heel raises :
Heel raises are done while standing. Start by placing one hand on the back of a chair for balance. Now slowly lift the heel of your injured leg up, standing on your tiptoes. Stay there for five to 10 seconds. Slowly lower your heels. Repeat 10 times.
2. After Surgery : (Post Operative Rehabilitation)
First Week 1 :
Regular icing and elevation are used to reduce swelling. The goal is full extension and 70 degrees of flexion by the end of the first week. The use of a knee brace and crutches are imperative.
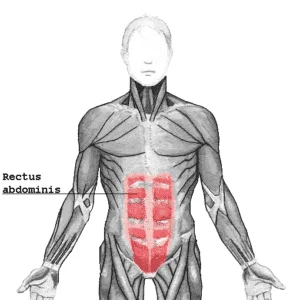
Multidirectional mobilizations of the patella should be included for at least 8 weeks. Other mobilization exercises in the first 4 weeks are passive extension of the knee (no hyperextension) and passive and active mobilization towards flexion. Strengthening exercises for the calf muscle, hamstring and quadriceps (vastus medialis) can be performed.
Week 3-4 :
The patient must try to genuinely increase the stance phase in an attempt to walk with one crutch. With good hamstring/quadriceps control, the use of crutches can be reduced earlier.
Week 5 :
The use of the knee brace is progressively reduced. Passive mobilizations should normalize motility but flexion should not yet be thorough. hamstrings and quadriceps (vastus medialis) can start in close chain exercises. The exercises should be started on light intensity (50% of maximum force) and progressively increased to 60-70%. The closed chain exercises should be built from less responsible positions (leg presses, step) to morecongested starting positions (ex.squad). The progress of the exercise depends on pain, swelling and quadriceps control.
Proprioception and coordination exercises can start if the general strength is good. This includes balance exercises on boards and toll.
Week 10 :
Forward, backward and lateral dynamic movements can be included as well as isokinetic exercises.
After Month 3 :
After 3 months, patient can move on to functional exercises as running and jumping. As proprioceptive and coordination exercises become
heavier, quicker changes in direction are possible. To stimulate coordination and control through afferent and efferent information processing, exercises should be enhanced by variation in visible input, surface stability , speed of exercise performance, complexity of the task, resistance, one or two-legged performance, etc.
Month 4-5 :
Final goal is to maximize endurance and strength of the knee stabilizers, optimize neuromuscular control with plyometric exercises and to add the sport-specific exercises. Acceleration and deceleration, variations in running and turning and cutting manoeuvers improve arthrokinetic reflexes to prevent new trauma during competition.
DO’S & DON’TS FOR ACL INJURY
~Get plenty of rest – Your body will need as much energy as it can get to repair the damaged tissues in your knee. Stay off your feet when possible and take it easy for the first few weeks after surgery, when healing is happening the fastest.
~Use cryotherapy – Cold therapy is proven to help reduce the pain and swelling that comes after knee surgery. Reducing swelling will help contribute to a faster recovery, so ice your knee regularly. If possible, use an active cold therapy system to get the most from cryotherapy.
~Use compression therapy – Compression bandages and modern active compression therapy systems help remove excess fluid from the area surrounding the knee joint to help accelerate healing.
~Do Regular physiotherapy – Work with a physical therapist to learn the strengthening and stretching exercises that will help you heal faster and prevent future injuries.
~Don’t do too much too soon – Although it may be tempting to return to normal activity as soon as possible, especially after the initial pain fades away, your body needs more time to heal fully. Follow your physical therapist’s instructions closely and don’t do more than they recommend.
~Don’t skip doctor visits – Keep the appointment schedule your doctor provides. It is important to stay on track throughout your recovery and only your doctor can confirm that the repairs they performed are healing correctly.
~Don’t end physiotherapy as early as possible – Because the pain subsides and you can get a comfortable range of motion back relatively quickly, many people are tempted to stop going to physical therapy sessions before they have fully recovered. Follow the entire course of care to ensure that the healing process is allowed to complete fully.



10 Comments