Popliteal Bursitis:
Table of Contents
What is popliteal bursitis?
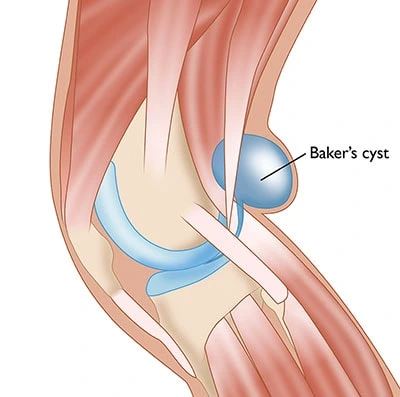
Popliteal bursitis develops from the capsule within the knee. It finishes up protruding into the tissues at the rear of the knee. Popliteal bursitis may be felt as a soft swelling within the back of the knee.
Definition:
A popliteal cyst, better called Baker’s cyst, could be a fluid-filled swelling that’s developed at the rear of the knee within the popliteal fossa region. some benign cystic tumors that originate from synovial tissue are known as ganglia. there are some common areas in the body for the cyst to develop for example at the wrist, hand, foot, and knee.
Some anatomical structures can feel pressure on them because of the cyst. the most commonly affected body part of the cyst is the venous blood vessel. which might become thrombophlebitis.
Clinically Relevant Anatomy:
A Baker’s cyst is an enlarged bursa that’s normally located between the medial head of the gastrocnemius and a capsular reflection of the semimembranosus, named the oblique popliteal ligament. the 2 requirements for cyst formation are anatomical communication and chronic effusion. knee effusions may replete the gastrocnemius-semimembranosus bursa with secretion and if the fluid outflow is hindered by a unidirectional mechanism, the gastrocnemius-semimembranosus bursa enlarges giving rise to a pseudocyst cavity, named as a Baker’s cyst.
Causes of Popliteal Bursitis:
The knee is formed of bone, tendons, and cartilage. The tendons and cartilage need lubrication, which they get from secretion – it helps the legs move smoothly and reduces friction.
There are various pouches, called bursae, in each knee, through which the synovia circulates. Between the popliteal bursa – a pouch at the rear of the knee – and therefore the genu, there’s a valve-like system that regulates the flow of secretion.
If the knee produces an excessive amount of synovia, there is often an accumulation of it within the popliteal bursa.
This can be caused by an inflammation of the hinge joint, usually thanks to an underlying condition, such as:
- Gout – levels of acid within the blood rise until the amount becomes excessive (hyperuricemia), causing urate crystals to make up around the joints. This causes inflammation and severe pain.
- Hemophilia – is an inherited medical condition where the blood doesn’t clot properly, resulting in internal bleeding and joint damage.
- Lupus – is an autoimmune disorder where the body’s system attacks normal, healthy tissue.
- Osteoarthritis – a type of arthritis caused by inflammation, breakdown, and also the eventual loss of cartilage within the joints – the cartilage wears down over time.
- Psoriasis – some patients who are suffering from psoriasis may feel pain and inflammation in their joints.
- Reactive arthritis –is a chronic (long-term) kind of arthritis that is present with inflamed joints, inflammation of the eyes, and inflammation of the genital, urinary, or systema digestorium.
- Rheumatoid arthritis – is an inflammatory variety of arthritis.
- Septic arthritis – is a joint inflammation that is caused by a bacterial infection.
- Injury – injury or trauma to the knee, like a cartilage tear, can result in a Baker’s cyst; they’re common among athletes.
Symptoms of Popliteal Bursitis:
Symptoms can include:
- Vague posterior pain
- Swelling and a mass within the popliteal space
- Limited range of motion
- Stiffness within the back of the knee sometimes increased by activity
- Tightness behind the knee.
Most cysts are found on the medial side of the popliteal space within the gastrocnemius-semimembranosus bursa, but they might be found within the popliteal bursa therefore the mass is found on the lateral side of the popliteal space. Also, there are some rare cases within which popliteal cysts extend superiorly or anteriorly.
Cysts may vary in size from small, from clinically, asymptomatic and not palpable, to large masses causing visible swelling of the patient’s knee. the scale of the cyst or pain can cause limitations in range of motion. If the cyst is large, it’s going to end in mechanical problems in knee flexion and limiting mobility. In rare cases, there’ll be signs and symptoms of a meniscal tear which may be tested by the McMurray test.
If it compresses the arteria poplitea or vein then it can lead to ischemia or thrombosis, and if the compression is on the tibial or peroneal nerve then it can lead to peripheral neuropathy.
A ruptured cyst can manifest as calf pain or perhaps swelling, it can even cause an itching feeling within the calf. These symptoms are more common in the patient suffering from an inflammatory pathology than in the patient suffering from degenerative pathology.
Diagnosis of Popliteal Bursitis:
Medical History and Physical Examination:
Your doctor will take a full medical record and ask you to explain your symptoms. He or she’s going to want to understand if you’ve got had a previous knee injury.
The doctor will carefully examine your affected knee while comparing it to your unaffected knee. During the examination he or she is going to look for the following changes:
- Swelling
- Instability of the joint
- A clicking or popping noise once you bend your knee
- Joint stiffness and limited range of motion
Patients with a Baker’s cyst commonly have symptoms of meniscal or chondral pathology which might be tested by the McMurray test. Symptoms associated with a popliteal cyst are rare. the foremost common symptoms are popliteal swelling and posterior aching. Patients might also complain of pain that happens with terminal knee extension. During the examination testing of knee flexion is useful.
A palpable cyst is commonly firm in full knee extension and soft in knee flexion. This finding is thought of as “Foucher’s sign” and is because of cyst compression. With the extension, the gastrocnemius and therefore the semimembranosus muscles approximate one another, and also the joint capsule compresses the cyst against the deep fascia. The mechanism of Foucher’s sign is beneficial for distinguishing Baker’s cysts from lesions like arteria poplitea aneurysms, adventitial cysts, ganglia, and sarcomas, that the palpation of the mass is unaffected by the knee position, therefore this is often considered the test for locating a Baker’s cyst.
Imaging Tests:
There are some imagining tests that can be performed to help in confirming the diagnosis and to gain more information about the patient’s conditions.
- The x-rays-These test provides information about the dense structures in the body like bones. Although a cyst can not be seen on an x-ray, one is also ordered in order that your doctor can search for narrowing of the joint space and other signs of arthritis within the joint.
- Ultrasound-This test uses sound waves to make images of structures inside the body. Ultrasound imaging can be helpful to determine whether the cyst is solid or full of fluid.
- Magnetic resonance imaging (MRI) scans– These tests are more helpful to have an idea of the body’s soft tissue. Doctors often suggest these tests to find out more about the cyst, tear, or any underlying disease.
Differential Diagnosis of Popliteal Bursitis:
Baker’s cysts are often mistaken for several other injuries within the knee. The patient’s history, in addition, because the clinical investigation and imaging afford proper medical diagnosis of the disease:
Popliteal Cyst may be confused with lipoma which might represent less resisting pressure in comparison to a Baker’s cyst or aneurysm differentiated by Doppler evaluation (ultrasound).
If the popliteal cyst becomes infected, this could often lead to a painful mass behind the knee. In such cases, it can be difficult to create a diagnosis, and also the infected cyst will be mistaken for a neoplasm. The cyst can rupture (split open) leading to severe calf pain, and decreased motion at the ankle, and cause similar symptoms as a deep vein thrombosis (evident on ultrasound or venogram).
It is important to diagnose a ruptured Baker’s cyst early so as to see the most effective treatment and avoid complications, like compartment syndrome, and to differentiate from:
- Muscle strain or tear-It is present with palpable mass/tenderness, swelling/warmth, pain on contraction and/or stretch of muscle
- Muscle contusion or hematomas-it presents with local damage to muscle (bleeding, swelling), and painful muscle contraction/stretch. If the hematoma is chronic, organized thickening can be developed
- Muscle spasm or cramp- it presents with painful palpable lump/thickening, the possible range of motion restriction, pain on the stretch of muscle
- Fascial tear with muscle herniation-it presents with palpable soft mass, severe muscle pain with increased activity, localized swelling after activity
- Myositis ossificans– it presents with a palpable painful mass within the muscle, micro tears within the muscle fibers that cause pain and swelling with contraction or stretch, loss of motion from restricted muscle function
- Deep vein thrombosis (DVT)- Constant pain, pain on passive dorsiflexion (Homan’s sign), localized warmth, localized tenderness on calf palpation and possible swelling, elevated blood heat
- Benign tumor- it presents with localized pain and tenderness, is also palpably soft or hard, and may cause movement dysfunction (location dependent)
- Malignant tumor- it presents with generalized malaise, possible sudden weight loss, localized pain, and/or swelling of various sizes and consistency
- Hemangioma- it present for an extended time, slow changes in size over time, palpable lump, could also be painful, which may/may not limit motion
Treatment of Popliteal Bursitis:
Treatment of a Baker’s cyst usually starts with conservative treatment. One time-honored method that sports doctors and orthopedic surgeons have relied on for many years to appease swelling from joint damage is the RICE method: Rest, Ice, Compression, and Elevation. Medications and Physiotherapy treatment also help to cure the disease and reduce the chances of surgery.
Medical treatment of Popliteal Bursitis:
Often, your healthcare provider will suggest that you simply start with nonsurgical treatment of your Baker’s cyst. These generally stuff you can do on your own, that may improve your symptoms.
Nonsurgical treatment options can include the RICE method:
- Resting your leg whenever possible.
- Applying ice to your knee.
- Using compression wraps on your knee decreases the number of joint swelling.
- Elevating your knee while you’re resting.
Other conservative treatment options for a Baker’s cyst can include:
Taking an anti-inflammatory medication, like ibuprofen.
Maintaining a healthy weight, which may help put less pressure on your joints.
Avoiding activities that strain your knee. This includes avoiding high-impact sports like jogging.
Using a crutch or cane for your walk.
Getting a physiotherapy treatment for strengthening your knee and body
Your healthcare provider may additionally offer you a steroid injection. This involves cortisone being injected into your hinge joint, which may reduce inflammation (swelling) and pain.
Physiotherapy treatment for Popliteal Bursitis:
A program can improve the control of the articulatio genus by a range of motion exercises. it’ll increase the motion of the joint additionally and increases flexibility. The physiotherapist will provide mobility, a hamstring stretching program, and a concurrent quadriceps strengthening program that must repeat several times every day. this may end in less pain at about 6-8 weeks.
Seated hamstring stretches:
How to do it:

- While seated, rest your heel on the ground along with your knee straight.
- Gently lean forward until you’re feeling a stretch behind your knee and thigh.
- Why it helps: This stretch is often useful to improve knee extension if it is limited.
Heel slide:
How to do it:
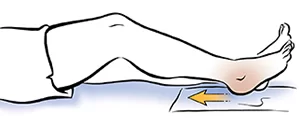
- Lie on your back with your knees straight.
- Bring your heel toward your buttock while sliding as you bend your knee.
- Hold a mild stretch during this position and so return to the original position
Why it helps: This exercise is accustomed to gently improving knee flexion if it’s limited.
Standing calf stretch:
How to do it:

- Start by standing near a wall.
- Step forward with one foot and keep both feet facing toward the wall.
- Keep the knee of your back leg straight.
- Bring your body forward toward the wall and support yourself with your on-the-wall arms as you permit your front knee to bend until you are feeling a delicate stretch along the rear of your straight leg.
- Move closer or farther faraway from the wall to manage the stretch of the rear leg.
Why it helps: after you have a Baker’s cyst, the backside of the leg will be tight. This stretch will help release a number of the strain within the lower leg.
Wall squat:
How to do it:

- Lean against a wall or a door, so your feet are about a foot far from you.
- Slide your body down towards the floor while keeping your back against the wall.
- Hold for 3 seconds, then return back to an upright position.
Why it helps: Squats help in the strengthening of quadriceps muscles which support the knee. Strength within the lower body is important for managing a Baker’s cyst.
Side-stepping:
How to do it:

- Begin with or without a resistance band around your ankles and your knees should be slightly bent.
- Keep your weight on your heels as you slowly take a step out to the side and permit the opposite leg to follow without losing tension in the band.
Why it helps: This exercise helps in strengthening the gluteal muscles, which helps stabilize your hip and knee.
Straight Leg Raise:
How to do it:
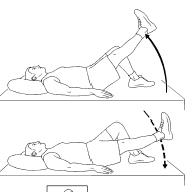
- Lie on your back along with your hips square and your legs laid out comfortably on the ground.
- Bend the knee of your non-injured leg at a 90-degree angle, planting the foot flatly on the ground.
- Stabilize the muscles of your affected leg by contracting your quadriceps (the group of muscles on the front of your thigh).
- Inhaling slowly, lift the straight leg six inches or to the level of your unaffected leg off the bottom.
- Hold for 3 seconds.
- Exhaling slowly, lower the leg to the ground with control.
- Relax and repeat 10 times more.
- When done correctly, you may feel the strain in your hip, thigh, and abdomen throughout the movement
Bridging exercise:
How to do it:

- Find an open space on the ground and lie on your back, employing a mat if you have got one.
- Rest your hands at your sides, bend your knees, and place your feet flat on the ground, beneath your knees.
- Tighten your abdominal and buttock muscles by pushing your low into the bottom.
- Raise your hips upward to form a line from your knees to your shoulders.
- Squeeze your core muscles and pull your belly button backward to your spine.
- Hold for 20 to 30 seconds. Lower your hips and relax.
Clamshell for External Hip Rotation:
How to do it:

- Lie on one side of the body (with your spine in an exceedingly neutral position) with your hips should be in a flexion position and your feet together.
- According to your strength level, perform the exercise with or without using an exercise band tied around your knees.
- Slowly raise your knee upward as far as you’ll be able to without rolling your pelvis backward.
- Keep your core engaged. the sole movement should be from your knee lifting up. don’t let the exercise band advance on top of the painful swelling area.
- Perform this exercise once a day with 15 to 20 seconds of hold.
Clamshell for Internal Hip Rotation:
How to do it:

- Lie on your side (with your spine in an exceedingly neutral position) along with your hips flexed and your feet together.
- According to your strength level, perform the exercise with or without an exercise band tied around your ankles.
- Slowly raise your foot upward as far as you’ll be able to without rolling your pelvis backward.
- Keep your core engaged. the sole movement should be from your ankle lifting up.
- Perform this exercise once a day with 15 to 20 seconds of hold.
Surgical Treatment of Popliteal Bursitis:
Even though surgery isn’t the first line of treatment to treat a Baker’s cyst, there are some cases where surgery can be recommended. Surgery could also be wont to repair the source of your knee damage.
Your provider might suggest a surgical choice to you if:
Your knee pain is severe.
You’re unable to maneuver your knee well (limited range of motion).
In many cases, your provider will treat the reason for your condition so as to mend your Baker’s cyst. To treat Popliteal bursitis your orthopedic will perform the surgery to correct the damage to your knee or treat the injury. In many cases, your orthopedic will concentrate on treating the cyst itself.
Surgical options for Baker’s cysts can include:
- Cyst draining: In this technique, your orthopedic can drain the fluid out of the cyst with a needle.
- Arthroscopic Knee Surgery: This procedure may be wont to both diagnose and proper knee damage. Your surgeon will make a tiny low cut in your knee and insert a tool called an arthroscope (a flexible tool with a camera on the end). this can be also called knee scoping.
- Knee Osteotomy: During this procedure, your surgeon cuts a part of the bone so as to correct damage to your knee. This surgery is an option for those with arthritis and knee pain.
Recovery after the surgery of Popliteal Bursitis:
Recovery times can vary from person to person. What one person experiences when recovering from knee surgery might not be what you experience.
Some tips to stay in mind as you recover can include:
- Avoiding strenuous activities.
- Keep your knee elevated for some days after surgery to decrease swelling or any pain you will feel.
- Taking all of your pain and antibiotic medications as instructed by your orthopedic surgeon.
- Going to your follow-up appointment together with your provider several days after your surgery.
- Doing physiotherapy treatment to continue strengthening your knee if it’s been suggested by your provider.
After surgery, you’ll feel a bit of tenderness and throbbing pain in your knee. Reach immediately to your orthopedic if this, or any of the pain, continues as you recover. you must be able to drive period of time after your surgery. consult with your provider about once you can do other activities.
The complication of Popliteal Bursitis if left untreated:
Not all Baker’s cysts are treated. you may feel that pain in the area of the popliteal bursa is mild so you will leave it untreated. The cyst might get away on its own if it isn’t treated.
However, there are other complications that will happen if a Baker’s cyst is left untreated, including:
- The pain getting worse.
- The cyst increases in size.
- The cyst burst, causing bruising within the lower leg.
If the cyst doesn’t depart, reach bent to your healthcare provider. It’s important to induce the proper diagnosis and confirm it’s a Baker’s cyst. This condition may be mistaken for something more serious sort as a tumor or artery aneurysm, which could be a medical emergency.
Prevention:
The best thanks to preventing a Baker’s cyst is to forestall knee injuries. some ways you’ll be able to prevent an injury to your knee include:
- Wearing proper footwear.
- Using the balls of your feet to show rather than your knees.
- Warming up properly before you exercise and cooling down after the exercise.
- Stopping immediately after you get a knee injury. It’s important to follow the RICE protocol after the injury. seek advice from your healthcare provider about any knee injuries to create sure you’re caring for them correctly.
FAQs:
How long do Baker’s cysts usually last?
A Baker’s cyst can sometimes rupture (burst), leading to fluid leaking down into your calf. This causes a pointy pain in your calf, which becomes swollen, tight, and red, but redness may be harder to determine on brown and black skin. The fluid will gradually be reabsorbed into the body within some weeks.
Does a hot pad help a Baker’s cyst?
There are several ways to scale back your pain and discomfort if you’ve got been diagnosed with a baker’s cyst: Ice your knee for about 20 minutes two to 3 times each day, as long as pain and swelling persist. employing a warmer once on a daily basis or taking a warm bath can even help relieve swelling.
Is massage good for a Baker’s cyst?
Massage doesn’t really help in the treatment of Baker’s cyst. Because it’s a fluid-filled mass with a one-way valve, mechanical pressure on the cyst won’t do anything to assist the fluid moving out of it and will after all irritate the matter further.
Can a Baker’s cyst cause a blood clot?
DVT related to Baker’s cyst is very common and these two conditions are thought to be causally related. Baker’s cyst is the most frequent mass lesion within the popliteal region. we recommend that Baker’s cyst could be a risk factor for PE likewise as surgery and trauma.
Can a Baker’s Cyst’s pain spread downwards to the leg?
In some cases, a Baker cyst causes no pain, and you will not notice it. If you are doing have symptoms, they could include: Swelling behind the knee, and sometimes within the leg. Knee pain.
How painful is it to empty a Baker’s cyst?
Most patients don’t report any pain during the procedure but you’ll feel slight pressure when the needle is inserted into the cyst. Once the procedure is complete, your doctor may put a little bandage on the location.
Can a knee cyst be cancerous?
Periarticular cysts and cystic soft tissue lesions around the knee are common. Synovial sarcoma may be a rare and malignant soft tissue tumor accounting for roughly 5% of soppy tissue sarcoma.