Coronary Artery Disease (CAD)
Table of Contents
What is coronary artery disease (CAD)?
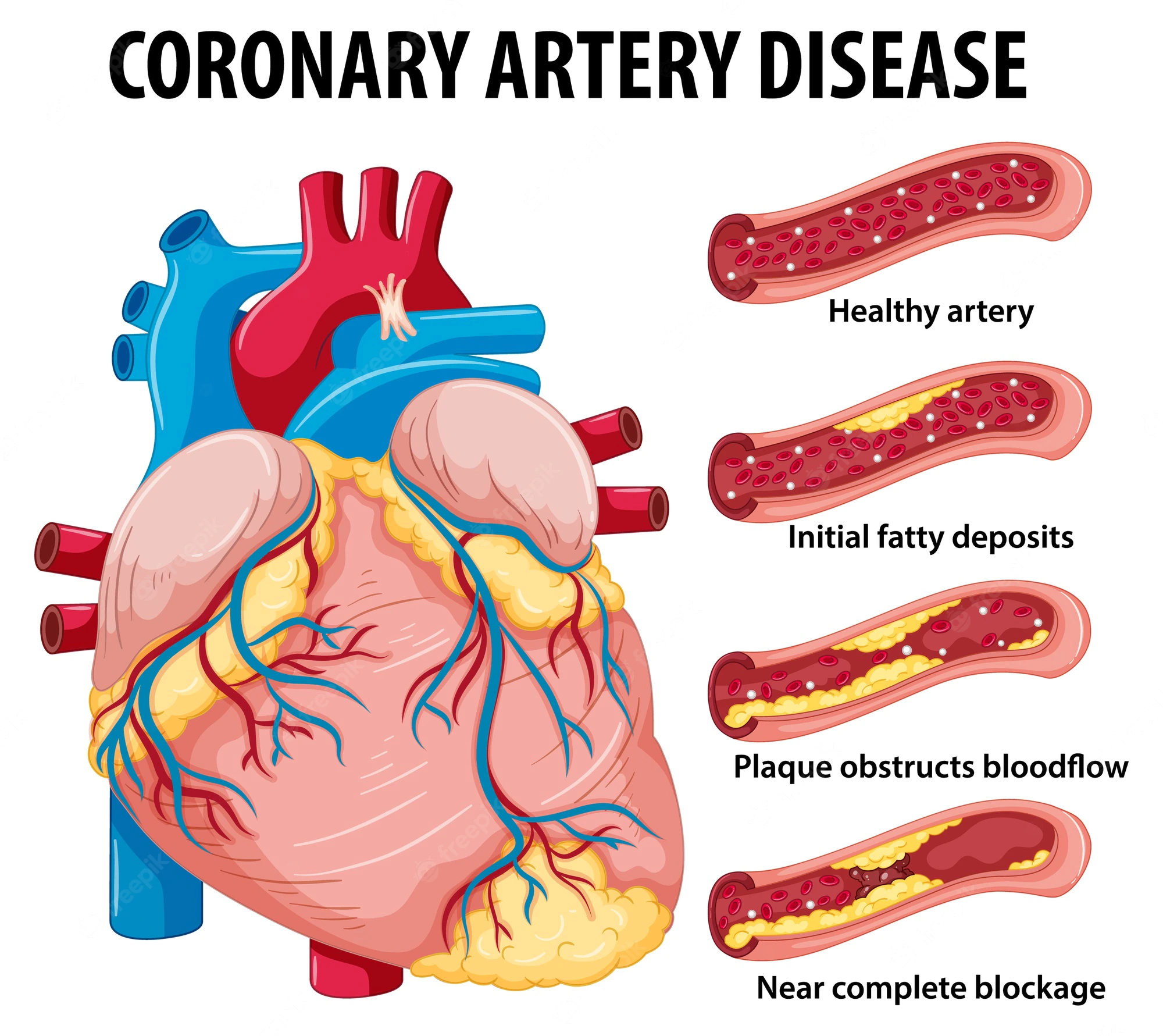
- Coronary artery disease (CAD) is a usual heart condition. The major blood vessels that supply the heart (coronary arteries) struggle to make enough blood, oxygen, & nutrients to the heart muscle. Cholesterol deposits (plaques) in the heart arteries & inflammation are commonly the cause of coronary artery disease (CAD).
- Signs & symptoms of coronary artery disease (CAD) occur when the heart does not get enough oxygen-rich blood. If you have coronary artery disease (CAD), reduced blood flow to the heart can cause chest pain (angina) & shortness of breath. A complete blockage of blood flow can cause a heart attack (HA).
- Coronary artery disease (CAD) sometimes develops over decades. Symptoms may go unnoticed until a significant blockage causes problems or a heart attack happens. Following a heart-healthy lifestyle can assist prevent coronary artery disease.
- Coronary artery disease (CAD) may also be known as coronary heart disease.
- Coronary artery disease (CAD) causes impaired blood flow in the arteries that supply blood to the heart. Also called coronary heart disease (CHD), CAD (coronary heart disease) is the most usual form of heart disease & affects approximately 16.5 million trusted Source Americans over the age of 20.
- It is also the leading trusted Sourceuse of deathTrusted Source for both men & women in the United States. It is estimated that every 36 seconds trusted Source, someone in the United States has a heart attack.
- A heart attack can come from uncontrolled coronary heart disease (CAD).
- Coronary artery disease (CAD) is a condition that harms your coronary arteries, which supply blood to your heart. With coronary artery disease (CAD), plaque buildup smalls or blocks one or more of your coronary arteries.
- Chest discomfort (angina) (Pain) is the most usual symptom. Coronary artery disease (CAD) can conduct in a heart attack or other complications like arrhythmia or heart failure.
- The common cause is the build-up of plaque. This causes coronary arteries to small, limiting blood flow to the heart.
- Coronary artery disease can range from no symptoms to chest pain )chest angina), to a heart attack.
- Treatments involve lifestyle changes, medication, angioplasty, and surgery.
Coronary artery disease (CAD) symptoms
- When your heart does not get enough arterial blood, you may experience a variety of symptoms. Angina (chest discomfort) is the most common symptom of coronary artery disease (CAD).
Certain people describe this discomfort as:
- chest pain
- heaviness
- tightness
- burning
- squeezing.
- These symptoms can be mistaken for heartburn or indigestion (acidity).
Other symptoms of coronary artery disease (CAD) include:
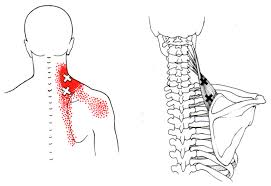
- pain in the arms or shoulders
- shortness of breath
- sweating
- dizziness.
- You may experience extra symptoms when your blood flow is more restricted. If a blockage cuts off blood flow completely or nearly completely, your heart muscle will begin to die if not restored. This is a heart attack.
- Do not ignore any of these symptoms, especially if they are excruciating or last longer than five minutes. Immediate medical treatment is required.
- Symptoms may go unrecognized at 1st, or they may only happen when the heart is beating hard like during exercise. As the coronary arteries continue to small, less & less blood gets to the heart, & symptoms can become more severe or frequent.
- Chest pain (angina): You may sense pressure or tightness in your chest. Certain people say it feels like someone is standing on their chest. The chest pain commonly occurs on the middle or left side of the chest. Activity & strong emotions can trigger angina. The pain commonly goes away within minutes after the triggering event ends. In certain people, especially women, the pain may be brief or sharp and felt in the neck, arm, or back.
- Shortness of breath: You may feel like you can not catch your breath.
- Fatigue: If the heart can not pump enough blood to meet your body’s needs, you may feel uncommonly tired.
- Heart attack: A completely blocked coronary artery will cause a heart attack (HA). The classic signs & symptoms of a heart attack involve crushing chest pain or pressure, shoulder or arm pain, shortness of breath, and sweating. Women may have decreased typical symptoms, such as neck or jaw pain, nausea, & fatigue. Some heart attacks do not cause any noticeable signs or symptoms.
Symptoms of coronary artery disease (CAD) for women
Women may also experience the above symptoms, yet they are also more likely to have:
- nausea
- vomiting
- back pain
- jaw pain
- shortness of breath without feeling chest pain.
- Men have a higher risk trusted Source of developing heart disease than women, however.
Due to the decreased blood flow, your heart may:
- become weak
- develop abnormal heart rhythms (arrhythmia) or rates
- fail to pump as much blood as your body requires
- Your doctor will diagnose these heart abnormalities during diagnosis.
Causes of coronary artery disease (CAD)
- The most common cause of coronary artery disease (CAD) is a vascular injury with cholesterol plaque buildup in the arteries, known as atherosclerosis. Reduced blood flow happens when one or more of these arteries becomes partially or completely blocked.
- Coronary artery disease begins when fats, cholesterols, and other substances collect on the inner walls of the heart arteries. This condition is known as atherosclerosis. The buildup is known as plaque. Plaque can cause the arteries to small, blocking blood flow. The plaque can also burst, conducting a blood clot.
Besides high cholesterol, harm to the coronary arteries may be caused by:
- Diabetes or insulin resistance
- High blood pressure (HBP)
- Not getting enough exercise (sedentary lifestyle)
- Smoking or tobacco use.
Other rare causes of harm or blockage to a coronary artery also limit blood flow to the heart.
When to see a doctor
- If you think you are having a heart attack, immediately call 911 or your local emergency number. If you do not have access to emergency medical services, have someone drive you to the closest hospital. Drive yourself only as a rear option.
- Smoking or having high blood pressure, high cholesterol, diabetes, obesity, or a strong family history of heart disease creates you more likely to get coronary artery disease (CAD). If you are at high risk of coronary artery disease (CAD), talk to your healthcare provider. You may require tests to check for narrowed arteries & coronary artery disease (CAD).
Coronary artery disease diagnosis
- Diagnosing coronary artery disease (CAD) requires a review of your medical history, a physical examination, & other medical testing.
These tests involve:
- Electrocardiogram: This test monitors electrical signals that move through your heart. It may assist your doctor to determine whether you have had a heart attack.
- Echocardiogram: This imaging test uses ultrasound waves to create a picture of your heart. The results of this test reveal whether some things in your heart are functioning properly.
- Stress test: This particular test calculates the stress on your heart during physical activity & while at rest. The test monitors your heart’s electrical activity while you stroll on a treadmill or ride a stationary bike. Nuclear imaging or echocardiographic (ECG) imaging may also be performed for a portion of this test. For those unable to perform physical exercise, some medications can be used instead for stress testing.
- Cardiac catheterization (left heart catheterization): During this procedure, your doctor injects a special dye into your coronary arteries through a catheter inserted between an artery in your groin or wrist. The dye assists enhance the radiographic image of your coronary arteries to identify any blockages.
- Heart CT scan: Your doctor may use this imaging test to examine for calcium deposits in your arteries.
Coronary artery disease risk factors
- Understanding the risk factors for coronary artery disease (CAD) can help with your plan to prevent or decrease the likelihood of developing the disease.
Risk factors involve:
- high blood pressure (HBP)
- high blood cholesterol levels
- tobacco smoking,
- insulin resistance/hyperglycemia/diabetes mellitus (DM)
- obesity
- inactivity
- unhealthy eating habits
- obstructive sleep apnea
- emotional stress
- excessive alcohol consumption
- history of preeclampsia during pregnancy.
- The risk for coronary artery disease (CAD) also increases with age. Based on age alone as a risk factor, men have a greater risk for the disease starting at age 45 & women have a greater risk beginning at age 55. The risk for coronary artery disease (CAD) is also higher if you have a family history of the disease.
- Age: Getting older increases the risk of damaged and smaller arteries.
- Sex: Men are generally at greater risk of coronary artery disease (CAD). However, the risk for women increases later in menopause.
- Family history: A family history of heart disease makes you more likely to get coronary artery disease (CAD). This is especially right if a close relative (parent, sibling) developed heart disease at an early age. The risk is highest if your father or a brother had heart disease previous age 55 or if your mother or a sister developed it previous age 65.
- Smoking: If you smoke, quit. Smoking is bad for heart health. People who smoke have a remarkably increased risk of heart disease. Breathing in secondhand smoke also increases injury.
- High blood pressure: Uncontrolled high blood pressure can create arteries hard and stiff (arterial stiffness). The coronary arteries may become small, slowing blood flow.
- High cholesterol: Too much bad cholesterol in the blood can increase the risk of atherosclerosis. Bad cholesterol is known as low-density lipoprotein (LDL) cholesterol. Not enough good cholesterol — called high-density lipoprotein (HDL) — also conducts to atherosclerosis.
- Diabetes: Diabetes increases the risk of coronary artery disease (CAD). Type 2 diabetes and coronary artery disease share certain risk factors, such as obesity & high blood pressure.
- Overweight or obesity: Increasing body weight is bad for overall health. Obesity can conduct to type 2 diabetes & high blood pressure (HBP). Ask your healthcare provider or doctor what a healthy weight is for you.
- Chronic kidney disease: Having long-term kidney disease increases the risk of coronary artery disease (CAD).
- Not getting enough exercise: Physical activity is special for good health. A lack of exercise (sedentary lifestyle) is linked to coronary artery disease (CAD) and some of its risk factors.
- A lot of stress: Emotional stress may damage the arteries & worsen other risk factors for coronary artery disease (CAD).
- Unhealthy diet: Eating foods with a lot of saturated fat, trans fat, salt & sugar can increase the risk of coronary artery disease (CAD).
- Alcohol use: Heavy alcohol use can conduct to heart muscle damage. It can also worsen other risk factors of coronary artery disease (CAD).
- Amount of sleep: Too small & too much sleep have both been linked to an increased risk of heart disease.
Risk factors often happen together. One risk factor may trigger another one.
- When grouped together, some risk factors make you even more likely to develop coronary artery disease. For example, metabolic syndrome — a cluster of conditions that involves high blood pressure, high blood sugar, excess body fat around the waist & high triglyceride levels — increases the risk of coronary artery disease (CAD).
- Sometimes coronary artery disease (CAD) develops without any classic risk factors.
Other possible risk factors for coronary artery disease may involve:
- Breathing pauses during sleep (obstructive sleep apnea): This condition causes breathing to stop and begin during sleep. It can cause unexpected drops in blood oxygen levels. The heart must work harder. Blood pressure goes up.
- High-sensitivity C-reactive protein (hs-CRP): This protein appears in higher-than-usual amounts when there is inflammation somewhere in the body. High hs-CRP (C-reactive protein) levels may be a risk factor for heart disease. It is thought that as coronary arteries narrow, the level of hs-CRP (C-reactive protein) in the blood goes up.
- High triglycerides: This is a type of fat (lipid) in the blood. High levels may increase the risk of coronary artery disease (CAD), especially for women.
- Homocysteine: Homocysteine is an amino acid the body uses to create protein and to build and maintain tissue. Yet high levels of homocysteine may increase the risk of coronary artery disease (CAD).
- Preeclampsia: This pregnancy complication causes high blood pressure (HBP) and increased protein in the urine. It can conduct in a higher risk of heart disease later in life.
- Other pregnancy complications: Diabetes or high blood pressure during pregnancy are also known risk factors for coronary artery disease (CAD).
- Certain autoimmune diseases: People who have conditions like rheumatoid arthritis & lupus (and other inflammatory conditions) have an increased risk of atherosclerosis.
Complications of coronary artery disease (CAD)
Coronary artery disease can conduct to:
- Chest pain (angina): When the coronary arteries are small, the heart may not get enough blood when it needs it most — like when exercising. This can cause chest pain (angina) or shortness of breath.
- Heart attack: A heart attack can occur if a cholesterol plaque breaks open and causes a blood clot to form. A clot can block blood flow. The lack of blood can injure the heart muscle. The amount of damage depends on the area on how quickly you are treated.
- Heart failure: Narrowed arteries in the heart or high blood pressure (HBP) can slowly make the heart weak or stiff so it is harder to pump blood. Heart failure is when the heart does not pump blood as it should.
- Irregular heart rhythms (arrhythmias): Not enough blood to the heart can change normal heart signaling, causing irregular heartbeats.
Prevention of coronary artery disease (CAD)
- The same lifestyle habits used to assist treat coronary artery disease (CAD) can also help prevent it. A healthy lifestyle can assist keep the arteries strong and clear of plaque.
To increase heart health, follow these tips:
- Quit smoking
- Control high blood pressure (HBP), high cholesterol & diabetes
- Exercise often
- Maintain a healthy weight
- Eat a decrease-fat, low-salt diet that is rich in fruits, vegetables & whole grains
- Reduce & manage stress.
Coronary artery disease (CAD) anatomy
The 4 primary coronary arteries are located on the surface of the heart:
- right main coronary artery
- left main coronary artery
- left circumflex artery,
- left anterior descending artery.
- These arteries take oxygen (O2) & nutrient-rich blood to your heart. Your heart is a muscle that is responsible for pumping blood throughout your body and requires oxygen all the time. A healthy heart progresses approximately 3,000 gallons of blood through your body every day.
- Like any other organ or muscle, your heart must receive an adequate, dependable supply of blood in order to take out its work. Decreased blood flow to your heart can cause symptoms of coronary artery disease (CAD).
What is the treatment for coronary artery disease (CAD)?
- Treatments involve lifestyle changes, medication, angioplasty, and surgery.
- It is important to reduce or control your risk factors and seek treatment to lower the chance of a heart attack or stroke if you are diagnosed with coronary artery disease (CAD).
- Treatment also turns on your current health condition, risk factors, & overall well-being. For example, your doctor may prescribe medication therapy to treat high cholesterol or high blood pressure (HBP), or you may receive medication to control blood sugar if you have diabetes.
- Medications are the most common treatment for coronary artery disease (CAD).
- Lifestyle changes can also decrease your risk of heart disease and stroke.
For example:
- quit smoking tobacco,
- decrease or stop your consumption of alcohol,
- exercise regularly,
- decrease the weight to a healthy level,
- eat a healthy diet (decrease in saturated fat, sodium, & added sugar).
- If your condition does not increase with lifestyle changes & medication, your doctor may recommend a procedure to increase blood flow to your heart.
These procedures may be:
- balloon angioplasty: to widen blocked arteries and smooth down the plaque buildup, commonly performed with the insertion of a stent to assist keep the lumen open after the procedure.
- coronary artery bypass graft surgery: to restore the blood flow to the heart in open chest surgery.
- enhanced external counterpulsation: to stimulate the formation of new little blood vessels to naturally bypass clogged arteries in a noninvasive procedure.
Physiotherapy treatment of coronary artery disease (CAD)
- Cardiovascular diseases are the conducting cause of disability globally & despite the advances in clinical care & medicine, continue to be the principal cause of morbidity & mortality.
- Cardiac Rehabilitation is a complex intervention that requires the input of a multidisciplinary team to deliver the recommended seven core components.
- Physiotherapists have the appropriate training, knowledge, & skills to deliver the exercise component of cardiac rehabilitation & assist patients to return to their activities of daily life.
- However, cardiac rehabilitation remains underutilized due to poor referral & enrollment post-discharge. Evidence has demonstrated the beneficial role of physiotherapy in cardiac rehabilitation.
- Rehabilitation later a heart attack may take several months or more. The Physiotherapist will explain relaxation techniques, breathing exercises, and exercises to gradually strengthen leg and trunk muscles. Gradually, gentle activity like walking is introduced. Throughout the program, the Physiotherapist aims to rebuild the person’s confidence, improve exercise tolerance, & teach them to recognize the signs & symptoms of excess exercise.
- Regular aerobic exercise decreases the heart rate and blood pressure (BP) at rest and during exercise. This assists to reduce the workload on the heart and anginal symptoms may be alleviated. Regular exercise increases muscle function and the ability to take in and utilize oxygen better.
What is the outlook for coronary artery disease (CAD)?
- Everyone’s outlook on coronary artery disease (CAD) is different. You have better chances of preventing extensive damage to your heart the earlier you can begin your treatment or implement lifestyle changes.
- It is main to follow your doctor’s instructions. Take medications as directed and create the recommended lifestyle changes. If you have a higher risk for coronary artery disease (CAD), you can assist to prevent the disease by reducing your risk factors.
FAQs
Dizziness or weakness. Heart palpitations, or sensations of your heart racing or fluttering. Nausea or sweating. Shortness of breath.
After 45, men may have a lot of plaque buildup. Signs of atherosclerosis in women are likely to appear after age 55. Plaque is dangerous because it can break off and form a clot that blocks your artery and stops blood flow to your heart, brain, or legs. That might cause a heart attack, stroke, or gangrene.
Following the onset of heart disease, women can expect to live 7.9 years and men can expect to live 6.7 years, according to the Health and Retirement Survey study. (The survey defined “heart disease” as coronary artery disease, angina, congestive heart failure, or other heart problems.)
Coronary artery disease, also called CAD, is a condition that affects your heart. It is the most common heart disease in the United States. CAD happens when coronary arteries struggle to supply the heart with enough blood, oxygen, and nutrients. Cholesterol deposits, or plaques, are almost always to blame.
Plaques and blood clots can reduce blood flow through an artery. A buildup of fatty plaques in the arteries (atherosclerosis) is the most common cause of coronary artery disease. Risk factors include a poor diet, lack of exercise, obesity, and smoking.
Smoking. Smoking is a major risk factor for coronary heart disease.
High blood pressure. High blood pressure (hypertension) puts a strain on your heart and can lead to CHD.
Cholesterol drugs.
Aspirin.
Beta-blockers.
Calcium channel blockers.



8 Comments