Obesity: Physiotherapy Treatment
Table of Contents
Obesity define
Obesity is a medical condition in which excess body fat has accumulated to the extent that it may have an adverse effect on health. It is defined by body mass index (BMI) and further evaluated in terms of fat distribution via the waist–hip ratio and total cardiovascular risk factors.
It is the most common nutritional disorder in the United States. Obesity can have serious consequences for one’s quality of life and lifespan. Some East Asian countries use lower values. Obesity increases the likelihood of various diseases and conditions, particularly cardiovascular diseases, type 2 diabetes, obstructive sleep apnea, coronary heart disease, stroke, gallbladder disease, certain types of cancer, osteoarthritis, and depression.
Obesity is more common in older adults as their metabolism slows down; they tend to eat more and exercise less than those who are not obese.
Obesity causes :
Obesity is most commonly caused by a combination of excessive food intake, lack of physical activity, and genetic susceptibility. A few cases are caused primarily by genes, endocrine disorders, medications, or mental disorders. The view that obese people eat little yet gain weight due to a slow metabolism is not medically supported. On average, obese people have a greater energy expenditure than their normal counterparts due to the energy required to maintain an increased body mass.
Obesity BMI :
BMI (Body mass index) is widely used to diagnose obesity. To calculate BMI, multiply weight in pounds by 703, divide by height in inches, and then divide again by height in inches. Or other method is- divide weight in kilograms by height in meters squared.
To measure BMI online Clic Here(BMI Calculator)
Mostly, BMI provides average idea of body fat. However, BMI not able measure body fat, so some people, such as muscular athletes, may have a Higher BMI category even though they don’t have excess body fat.
Many doctors also measure a person’s waist/thigh/chest/arm/leg circumference to help guide treatment decisions. Obesity-related health conditions are more common in men with a waist circumference over 40 inches (102 centimeters) and in women with a waist measurement over 35 inches (89 centimeters).
Diagnostic method : BMI > 30 kg/m2
People are generally considered obese when their body mass index (BMI), a measurement obtained by dividing a person’s weight by the square of the person’s height, is over 30 kg/m2; the range 25–30 kg/m2 is defined as overweight.
BMI= m/h2
BMI (kg/m2) Classification
| BMI | Class |
| 18.5 or Under | underweight |
| 18.5 to 25 | Normal Weight |
| 25 to 30 | Overweight |
| 30 to 35 | class I obesity |
| 35 to 40 | class II obesity |
| 40 or Above | class III obesity (morbid or severe obesity) |

A BMI of = 35 kg/m2 and experiencing obesity-related health conditions or =40–44.9 kg/m2 is morbid obesity.
A BMI of = 45 or 50 kg/m2 is super obesity.
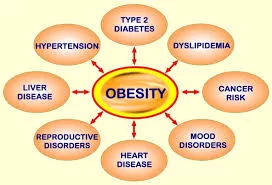
Obesity health risks
Excessive body weight is associated with various diseases and conditions, particularly cardiovascular diseases, diabetes mellitus type 2, obstructive sleep apnea, certain types of cancer, osteoarthritis, and asthma. As a result, obesity has been found to reduce life expectancy.
Mortality:
Obesity is one of the leading preventable causes of death worldwide, A number of reviews have found that mortality risk is lowest at a BMI of 20–25 kg/m2 in non-smokers and at 24–27 kg/m2 in current smokers, with risk increasing along with changes in either direction
Morbidity
Obesity increases the risk of many physical and mental conditions. These co-morbidities are most commonly shown in metabolic syndrome, a combination of medical disorders that includes: diabetes mellitus type 2, high blood pressure, high blood cholesterol, and high triglyceride levels.
Complications are either directly caused by obesity or indirectly related through mechanisms sharing a common cause such as a poor diet or a sedentary lifestyle. The strength of the link between obesity and specific conditions varies. One of the strongest is the link with type 2 diabetes. Excess body fat underlies 64% of cases of diabetes in men and 77% of cases in women.
Health consequences fall into two broad categories: those attributable to the effects of increased fat mass (such as osteoarthritis, obstructive sleep apnea, social stigmatization) and those due to the increased number of fat cells (diabetes, cancer, cardiovascular disease, non-alcoholic fatty liver disease). Increases in body fat alter the body’s response to insulin, potentially leading to insulin resistance. Increased fat also creates a proinflammatory state and a prothrombotic state.
Obesity is an important risk factor for many chronic physical and mental illnesses. The generally accepted view is that being overweight causes similar health problems to obesity
Cardiological:
HeartAttack (Myocardial infarct)
Ischemic heart disease: Obesity is associated with cardiovascular diseases including angina and myocardial infarction. A 2002 report concluded that 21% of ischemic heart disease is due to obesity while a 2008 European consensus puts the number at 35%.
Congestive heart failure Having obesity is associated to about 11% of heart failure cases in men and 14% in women.
High blood pressure: More than 85% of those with hypertension have a BMI greater than 25. The risk of hypertension is 5 times higher in the obese as compared to those of normal weight. A definitive link between obesity and hypertension has been found using animal and clinical studies, which have suggested that there are multiple potential mechanisms for obesity-induced hypertension. These mechanisms include the activation of the sympathetic nervous system as well as the activation of the renin–angiotensin–aldosterone system. The association between hypertension and obesity has been also well described in children.
Abnormal cholesterol levels: Obesity is associated with increased LDL cholesterol (bad cholesterol) and lowered HDL cholesterol (good cholesterol).
Deep vein thrombosis and pulmonary embolism: Obesity increases one’s risk of venous thromboembolism by 2.3 fold.
Dermatological: Obesity is associated with the incidence of stretch marks, acanthosis nigricans, lymphedema, cellulitis, hirsutism, and intertrigo.
Endocrine:
- Gynecomastia in an obese male.
- Diabetes mellitus
Gynecomastia: Obesity, according to a 2009 review, can be associated with elevated peripheral conversion of androgens into estrogens in some individuals.
Gastrointestinal
Gastroesophageal reflux disease: Several studies have shown that the frequency and severity of GERD symptoms are higher in those who are obese.
Cholelithiasis (gallstones) : According to NIH, obesity causes the amount of cholesterol in bile to rise, in turn the formation of stone can occur
Reproductive system (or genital system)
Polycystic ovarian syndrome (PCOS): Due to its association with insulin resistance, the risk of polycystic ovarian syndrome (PCOS) increases with adiposity. In the US approximately 60% of patients with PCOS have a BMI greater than 30. It remains uncertain whether PCOS contributes to obesity, or the reverse.
Infertility
Obesity leads to infertility in both men and women. This is primarily due to excess estrogen interfering with normal ovulation in women and altering spermatogenesis in men. It is believed to cause 6% of primary infertility. A review in 2013 came to the result that obesity increases the risk of oligospermia and azoospermia in men, with an of odds ratio 1.3. Being morbidly obese increases the odds ratio to 2.0.
Complications of pregnancy: Obesity is related to many complications in pregnancy including: haemorrhage, infection, increased hospital stays for the mother, and increased NICU requirements for the infant. Obese women have more than twice the rate of C-sections compared to women of normal weight. Obese women also have increased risk of preterm births and low birth weight infants.
Birth defects: Those who are obese during pregnancy have a greater risk of have a child with a number of congenital malformations including: neural tube defects such as anencephaly and spina bifida, cardiovascular anomalies, including septal anomalies, cleft lip and palate, anorectal malformation, limb reduction anomalies, and hydrocephaly.
Intrauterine fetal death: Maternal obesity is associated with an increased risk of intrauterine fetal death.
Neurological
MCA Territory Infarct (stroke)
Stroke
Ischemic stroke is increased in both men and women who are obese.
Meralgia paresthetica : Meralgia paresthetica is a neuropathic pain or numbness of the thighs, sometimes associated with obesity.
Migraines : Migraine and obesity are comorbid. The risk of migraine rises 50% by BMI of 30 kg/m2 and 100% by BMI of 35 kg/m2.The causal connection remains unclear.
Carpal tunnel syndrome : The risk of carpal tunnel syndrome rises 7.4% for each 1 kg/m2 increase of body mass index.
Dementia : Those who are obese have a rate of dementia 1.4 times greater than those of normal weight.
Idiopathic intracranial hypertension : Idiopathic intracranial hypertension, or unexplained high pressure in the cranium, is a rare condition that can cause visual impairment, frequent severe headache, and tinnitus. It is most commonly seen in obese women.
Multiple sclerosis : Women that are obese at age 18 have a greater than twofold increased risk of MS.
Cancer (or oncological)
Hepatocellular carcinoma 1: Many cancers occur at increased frequency in those who are overweight or obese. A study from the United Kingdom found that approximately 5% of cancer is due to excess weight.
These cancers include:
breast, ovarian esophageal, colorectal liver, pancreatic gallbladder, stomach endometrial, cervical prostate, kidney non-Hodgkin’s lymphoma, multiple myeloma.
A high body mass index (BMI) is associated with a higher risk of developing ten common cancers including 41% of uterine cancers and at least 10% of gallbladder, kidney, liver and colon cancers in the UK. For those undergoing surgery for cancer, obesity is also associated with an increased risk of major postoperative complications compared with those of normal weight.
Psychiatric :
Risk of suicide decreases with increased body mass index in the United States.
Depression : Obesity has been associated with depression.The relationship is strongest in those who are more severely obese, those who are younger, and in women.Suicide rate however decreases with increased BMI.
Social stigmatization: A 2011 systematic review indicated that obese people draw negative reactions, furthermore people are less willing to help the affected individual in any situation.
Respiratory system :
- Obstructive sleep apnea
- Obesity is a risk factor for obstructive sleep apnea.
Obesity hypoventilation syndrome
CPAP machine commonly used in OHS : Obesity hypoventilation syndrome is defined as the combination of obesity, hypoxia during sleep, and hypercapnia during the day, resulting from hypoventilation.
Chronic lung disease : Obesity is associated with a number of chronic lung diseases, including asthma and COPD. It is believed that a systemic pro-inflammatory state induced by some causes of obesity may contribute to airway inflammation, leading to asthma.
Complications during general anaesthesia : Obesity significantly reduces and stiffens the functional lung volume, requiring specific strategies for respiratory management under general anesthesia.
Obesity and Asthma : The low grade systemic inflammation of obesity has been show to worsen lung function in asthma and increase the risk of developing an asthma exacerbation.
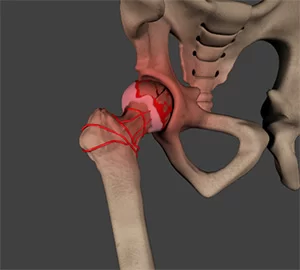
Rheumatological and orthopedic:
Gout : Compared to men with a BMI of 21–23, men with a BMI of 30–35 have 2.3 times more gout, and men with a BMI of greater than 35 have 3.0 times more gout. Weight loss decreases these risks.
Poor mobility : There is a strong association between obesity and musculoskeletal pain and disability.
Osteoarthritis : Increased rates of arthritis are seen in both weight-bearing and non-weight-bearing joints. Weight loss and exercise act to reduce the risk of osteoarthritis.
Low back pain: Obese individuals are twice to four times more likely to have lower back pain than their normal weight peers.
Traumatic injury : In women, class II obesity (i.e. BMI = 35) is a risk factor for osteoporotic fractures in general, as well as for upper arm fractures.
Urological and nephrological
Urinary system :
Urinary incontinence: Urge, stress, and mixed incontinence all occur at higher rates in the obese. The rates are about double that found in the normal weight population. Urinary incontinence improves with weight lost.
Chronic kidney disease : Obesity increases one’s risk of chronic kidney disease by three to four times.
Hypogonadism: In men, obesity and metabolic syndrome both increase estrogen and adipokine production. This reduces gonadotropin-releasing hormone, in turn reducing both luteinizing hormone and follicle stimulating hormone. The result is reduction of the testis’ production of testosterone and a further increase in adipokine levels. This then feeds back to cause further weight gain.
Erectile dysfunction: Obese men can experience erectile dysfunction, (as well as, in association with diabetes), however weight loss causes an improvement in their sexual functioning.
Management of obesity:
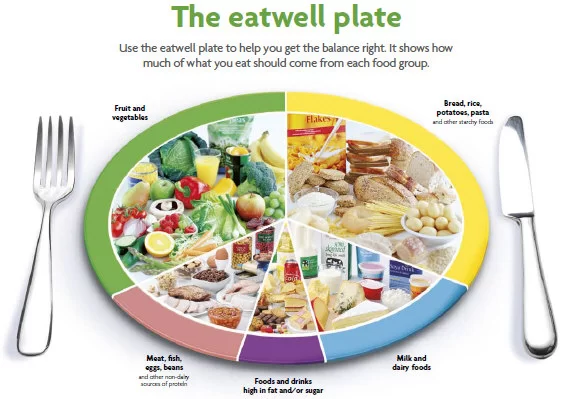
Dieting:
Dieting is the practice of eating food in a regulated and supervised fashion to decrease, maintain, or increase body weight, or to prevent and treat diseases, such as diabetes. A restricted diet is often used by those who are overweight or obese, sometimes in combination with physical exercise, to reduce body weight. Some people follow a diet to gain weight (usually in the form of muscle). Diets can also be used to maintain a stable body weight and improve health.
Diets to promote weight loss can be categorized as: low-fat, low-carbohydrate, low-calorie, very low calorie and more recently flexible dieting. A meta-analysis of six randomized controlled trials found no difference between low-calorie, low-carbohydrate, and low-fat diets, with a 2–4 kilogram weight loss over 12–18 months in all studies. At two years, all calorie-reduced diet types cause equal weight loss irrespective of the macronutrients emphasized. In general, the most effective diet is any which reduces calorie consumption.
Physiotherapy – Exercise :

Exercise is any bodily activity that enhances or maintains physical fitness and overall health and wellness. It is performed for various reasons, to aid growth and improve strength, preventing aging, developing muscles and the cardiovascular system, honing athletic skills, weight loss or maintenance, improving health and also for enjoyment. Many individuals choose to exercise outdoors where they can congregate in groups, socialize, and enhance well-being.
Physical exercises are generally grouped into three types, depending on the overall effect they have on the human body:
Aerobic exercise is any physical activity that uses large muscle groups and causes the body to use more oxygen than it would while resting. The goal of aerobic exercise is to increase cardiovascular endurance. Examples of aerobic exercise include running, cycling, swimming, brisk walking, skipping rope, rowing, hiking, dancing, playing tennis, continuous training, and long distance running.
Anaerobic exercise, which includes strength and resistance training, can firm, strengthen, and increase muscle mass, as well as improve bone density, balance, and coordination. Examples of strength exercises are push-ups, pull-ups, lunges, squats, bench press. Anaerobic exercise also include weight training, functional training, eccentric training, interval training, sprinting, and high-intensity interval training increase short-term muscle strength.
Resistance training involves lifting weights using either weight machines or free weights (dumbbells).
Flexibility exercises are a type of stretching that improves the movements of your muscles, joints, and ligaments.
Balance exercises improve your stability and reduce the chance of falling or other injuries. These exercises can be done without any equipment. For example, with single-leg balance, you balance on one foot for 15 seconds. A stand-sit involves standing up and sitting down without using your hands.
Your provider will design an exercise program for you that includes the frequency, intensity, time, and types of exercise. Typically, you’ll want to lose about 10% of your weight over a 6-month period. Be sure to set SMART goals (Specific, Measurable, Attainable, Realistic, Timely) to sustain the self-discipline required for long-term success. Also consider tracking your physical activity using a wearable device (eg, Fitbit) or a smartphone app. It lets you see your progress over time, helps you set new goals, and helps keep you motivated.
Flexibility exercises stretch and lengthen muscles. Activities such as stretching help to improve joint flexibility and keep muscles limber. The goal is to improve the range of motion which can reduce the chance of injury.
Physical exercise can also include training that focuses on accuracy, agility, power, and speed.
Sometimes the terms ‘dynamic’ and ‘static’ are used.[citation needed] ‘Dynamic’ exercises such as steady running, tend to produce a lowering of the diastolic blood pressure during exercise, due to the improved blood flow. Conversely, static exercise (such as weight-lifting) can cause the systolic pressure to rise significantly, albeit transiently, during the performance of the exercise.
Cardiovascular system:
The beneficial effect of exercise on the cardiovascular system is well documented. There is a direct correlation between physical inactivity and cardiovascular mortality, and physical inactivity is an independent risk factor for the development of coronary artery disease. Low levels of physical exercise increase the risk of cardiovascular diseases mortality.
Children who participate in physical exercise experience greater loss of body fat and increased cardiovascular fitness.
How does exercise help in the treatment of obesity?

The goal of treatment for obesity is weight loss. Exercise is an essential part of any weight-loss program and should become a permanent part of your lifestyle. The benefits of exercise can include:
- burning off calories and losing weight
- maintaining muscle tone
- increasing your metabolic rate (the amount of calories your body burns 24 hours a day)
- improving circulation
- improving heart and lung function
- increasing your sense of self-control
- reducing your level of stress
- increasing your ability to concentrate
- improving your appearance
- reducing depression
- suppressing your appetite
- helping you sleep better
- preventing diabetes, high blood pressure, and high cholesterol
- decreasing your risk of some cancers, such as breast, ovary, and colon cancer
BARIATRIC SURGERY:
Sleeve Gastrectomy :
The sleeve gastrectomy involves excision of approximately 80% of the stomach by using multiple firings of a linear stapler/cutter to separate a narrow tube or sleeve of the lesser curve of the stomach from the greater curve aspect. The antrum is preserved to maintain gastric emptying. A bougie is placed in the lesser curve segment during the resection to maintain adequate lumen yet achieve a standardised gastric remnant. The optimal size of this bougie is not yet agreed upon. A 36 French is the most common size but sizes from 30F to 50F are reported. The procedure is non-adjustable and non-reversible.
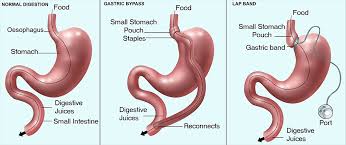
The procedure is a laparoscopic procedure, taking between 30 and 90 minutes. Some patients are treated on an outpatient basis but a one to two day stay is more common.
Gastric imbrication is a non-resectional variant of sleeve gastrectomy. The greater curve vascular pedicles are ligated and then the gastric wall is imbricated using two rows of sutures to create a narrow lumen, similar in size to the sleeve gastrectomy. The costs are reduced by avoiding the use of multiple firings of stapling devices and the risks are expected to be lower by the absence of the stapled closure of divided stomach.
Laparoscopic Adjustable Gastric Banding (LAGB):
The LAGB is placed laparoscopically. Commonly 3 x 5mm, 1 x 10mm and 1 x 15 mm ports are required. A path is developed from the top of the lesser curve of the stomach to the angle of His, the band is placed around this path, closed and then stabilized at this site with some sutures. The tubing passes to an access port, placed through a 3 cm incision over the left rectus abdominis muscle. The procedure takes 30 -50 minutes to complete and the patient is able to go home at a mean of 2 hours after completion of the procedure.
Roux en Y Gastric Bypass (RYGB):
Gastric bypass combines a marked reduction in the size of stomach available for food with a narrow stoma passing from the gastric pouch to a Roux-en-Y loop of jejunum diverting food from the duodenum and proximal jejunum. In a typical current laparoscopic version (figure 5), the stomach is divided completely by multiple firings of a device which places two rows of staples and cuts the gastric wall in between. This creates a small proximal gastric pouch of volume of 50ml or less and a large residual stomach, now excluded from the food. A Roux limb of jejunum is formed by dividing the proximal jejunum completely at about 50cm from the duodeno-jejunal flexure, taking the distal aspect of this point of division up to form a small anastomosis with the small gastric pouch and anastomosing the proximal aspect to the more distal jejunum at 50 cm below the gastro-jejunal anastomosis. The procedure takes 90 -150 minutes and the patient stays in hospital for 2 – 4 days.
Single anastomosis Gastric Bypass (SAGB):
This form of gastric bypass is increasingly popular as an alternative to the RYGB. It is variously known as the SAGB, OAGB (one anastomosis gastric bypass), OLGB (Omega loop gastric bypass) or MGB (Mini gastric bypass). It differs from the RYGB by having a loop of small bowel rather than a Roux limb, a long and narrow lesser curve gastric pouch and a longer bypass of the duodenum and proximal jejunum (typically, 150 cm rather than 40 cm)
Possible mechanisms of bariatric surgical effect:
Induce satiety, reduce appetite, control hunger
Change of taste preference – less sweet foods; lower fat content;
Restrict Intake
Diversion from upper GI tract
Malabsorption of macronutrients
Increased energy expenditure; Increased diet-induced thermogenesis
Aversion to food through side-effects
Inhibition of the metabolic adaptation to weight loss
Changes to the gut microflora
Changes to plasma bile acid levels
Changes in gut hormones: candidates include the incretins (GLP-1; GIP), ghrelin, CCK, Peptide YY,
Central mechanisms: Modify hedonics; central appetite control
Being overweight or obese causes osteoarthritis by increasing pressure on the knee and hip joints. Excessive weight can put stress on joints and promote the cartilage damage that often leads to osteoarthritis. Every pound of excess weight adds four pounds of pressure on the knees.
Obesity is one of the most common risk factors for osteoarthritis. Obesity causes an increase in mechanical stress and pressure on joints, which wears away the cartilage that normally protects the joints and causes pain and inflammation. Weight loss reduces the stress and the load on the hips, knees and lower back, thereby preventing or slowing the development of osteoarthritis in those joints.
While the exact cause of osteoarthritis isn’t known, being overweight or obese will accelerate it, due to the excess weight causing greater wear and tear on the joints.
For every pound you’re overweight, you’re adding four pounds of pressure on your knees and six pounds of pressure on your hips. The extra wear and tear from extra weight greatly increases your risk of eventually getting osteoarthritis in these joints.
Throw in a dose of inactivity and some weak leg muscles and you’ll almost certainly get OA. There’s an easy fix to this, though. Weight loss and a regular exercise program can help prevent OA and help you manage it better if you already have it.
Physiotherapy in osteoarthritis with obesity :
One of the most beneficial ways to manage OA is to get moving. While it may be hard to think of exercise when the joints hurt, moving is considered an important part of the treatment plan. Studies show that simple activities like walking around the neighborhood or taking a fun, easy exercise class can reduce pain and help maintain (or attain) a healthy weight.
Strengthening exercises build muscles around OA-affected joints, easing the burden on those joints and reducing pain. Range-of-motion exercise helps maintain and improve joint flexibility and reduce stiffness.
Aerobic exercise helps to improve stamina and energy levels and also help to reduce excess weight. Talk to a doctor before starting an exercise program.
Weight Management :
Excess weight adds additional stress to weight-bearing joints, such as the hips, knees, feet and back. Losing weight can help people with OA reduce pain and limit further joint damage. The basic rule for losing weight is to eat fewer calories and increase physical activity.
Stretching
Slow, gentle stretching of joints may improve flexibility, lessen stiffness and reduce pain. Exercises such as yoga and tai chi are great ways to manage stiffness.
Heart Disease and Stroke:
Extra weight makes you more likely to have high blood pressure and high cholesterol. Both of those conditions make heart disease or stroke more likely.
The good news is that losing a small amount of weight can reduce your chances of developing heart disease or a stroke. Losing even more weight has been shown to lower the risk even more.
Type 2 Diabetes:
Most people who have type 2 diabetes are overweight or obese. You can cut your risk of developing type 2 diabetes by losing weight, eating a balanced diet, getting adequate sleep, and exercising more.
If you have type 2 diabetes, losing weight and becoming more physically active can help control your blood sugar levels. Becoming more active may also reduce your need for diabetes medication.
Cancer :
Cancers of the colon, breast (after menopause), endometrium (the lining of the uterus), kidney, and esophagus are linked to obesity. Some studies have also reported links between obesity and cancers of the gallbladder, ovaries, and pancreas.
Gallbladder Disease
Gallbladder disease and gallstones are more common if you are overweight.
Ironically, weight loss itself, particularly rapid weight loss or loss of a large amount of weight, can make you more likely to get gallstones. Losing weight at a rate of about 1 pound a week is less likely to cause gallstones.
Gout:
Gout is a disease that affects the joints. It happens when you have too much uric acid in your blood. The extra uric acid can form crystals that deposit in the joints.
Gout is more common in overweight people. The more you weigh, the more likely you are to get gout.
Sleep Apnea :
Sleep apnea is a breathing condition that’s linked to being overweight.
Sleep apnea can cause a person to snore heavily and to briefly stop breathing during sleep. Sleep apnea may cause daytime sleepiness and make heart disease and stroke more likely.
Weight loss often improves sleep apnea.
Obesity Treatment in Type 1 Diabetes:
Obesity is increasingly common in patients with type 1 diabetes; in 1988, 25% of 40- to 49-year-olds with type 1 diabetes had overweight or obesity compared to 68% in 2007 (71). Patients with type 1 diabetes will need to continue to take their insulin and strive for a caloric reduction of 500–700 kcal/day to lose weight. The ADA recommends that adults with type 1 diabetes meet the CDC recommendations for physical activity for all adults—150 min/week of moderate aerobic activity and two sessions of resistance training per week (23). Patients with type 1 diabetes starting a new exercise regimen or caloric reduction will need to monitor closely for hypoglycemia. In addition, the weight loss medications described above can also be considered for patients with type 1 diabetes. Pramlintide may be considered in patients with type 1 diabetes as a means of reducing their insulin requirements and promoting weight loss.
hypoglycemia. In addition, the weight loss medications described above can also be considered for patients with type 1 diabetes. Pramlintide may be considered in patients with type 1 diabetes as a means of reducing their insulin requirements and promoting weight loss.
Diet, Physiotherapy for diabetes obese patients with type 2 :
Diet, physical activity, and behavioral therapy designed to achieve 5% weight loss should be prescribed for overweight and obese patients with type 2 diabetes ready to achieve weight loss.
Such interventions should be high intensity (≥16 sessions in 6 months) and focus on diet, physical activity, and behavioral strategies to achieve a 500–750 kcal/day energy deficit.
Diets that provide the same caloric restriction but differ in protein, carbohydrate, and fat content are equally effective in achieving weight loss.
For patients who achieve short-term weight loss goals, long-term (≥1-year) comprehensive weight maintenance programs should be prescribed. Such programs should provide at least monthly contact and encourage ongoing monitoring of body weight (weekly or more frequently), continued consumption of a reduced calorie diet, and participation in high levels of physical activity (200–300 min/week).
To achieve weight loss of >5%, short-term (3-month) high-intensity lifestyle interventions that use very low-calorie diets (≤800 kcal/day) and total meal replacements may be prescribed for carefully selected patients by trained practitioners in medical care settings with close medical monitoring. To maintain weight loss, such programs must incorporate long-term comprehensive weight maintenance counseling.
Among overweight or obese patients with type 2 diabetes and inadequate glycemic, blood pressure and lipid control, and/or other obesity-related medical conditions, lifestyle changes that result in modest and sustained
weight loss produces even greater benefits, including reductions in blood pressure, improvements in LDL and HDL cholesterol, and reductions in the need for medications to control blood glucose, blood pressure, and lipids .
Lifestyle Interventions:
Weight loss can be attained with lifestyle programs that achieve a 500–750 kcal/day energy deficit or provide approximately 1,200–1,500 kcal/day for women and 1,500–1,800 kcal/day for men, adjusted for the individual’s baseline body weight. Although benefits may be seen with as little as 5% weight loss, sustained weight loss of ≥7% is optimal.
These diets may differ in the types of foods they restrict (such as high-fat or high-carbohydrate foods) but are effective if they create the necessary energy deficit (13–16). The diet choice should be based on the patient’s Intensive behavioral lifestyle interventions should include ≥16 sessions in 6 months and focus on diet, physical activity, and behavioral strategies to achieve an ∼500–750 kcal/day energy deficit. Interventions should be provided by trained interventionists in either individual or group sessions .
Overweight and obese patients with type 2 diabetes who have lost weight during the 6-month intensive behavioral lifestyle intervention should be enrolled in long-term (≥1-year) comprehensive weight loss maintenance programs that provide at least monthly contact with a trained interventionist and focus on ongoing monitoring of body weight (weekly or more frequently), continued consumption of a reduced calorie diet, and participation in high levels of physical activity (200–300 min/week). Some commercial and proprietary weight loss programs have shown promising weight loss results.
When provided by trained practitioners in medical care settings with close medical monitoring, short-term (3-month) high-intensity lifestyle interventions that use very low-calorie diets (defined as ≤800 kcal/day) and total meal replacements may achieve greater short-term weight loss (10–15%) than intensive behavioral lifestyle interventions that typically achieve 5% weight loss.





10 Comments